Author:
Randy Alexander
Date Of Creation:
25 April 2021
Update Date:
1 July 2024

Content
Breast cancer is the leading cause of death among women in this country, according to the US Centers for Disease Control and Prevention. Breast cancer is easier to treat when it is found early, so to ensure breast health you must be aware of its condition. There are several ways to check your breasts for potential abnormalities. Be aware that men can get breast cancer, although it is uncommon, so you should see your doctor right away if you are a man and see any changes in breast tissue.
Steps
Method 1 of 4: Breast self-examination
Increase breast awareness. Observe regularly and be aware of the "normal" condition of the breast. The concept of "normal" is unique to each person, so you need to know how your "normal" breast looks and feels. Become familiar with the shape, feel, border, size, and so on, so you can see the change and let your doctor know. In addition, awareness of your breast condition also helps you take initiative in your health.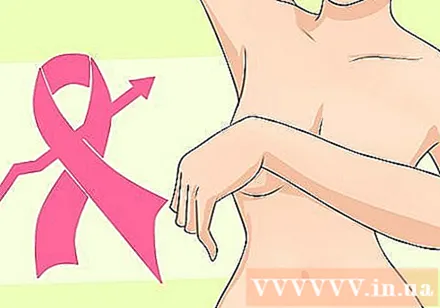
- Raising awareness is one of the best things you can do if you're concerned about the possibility of breast cancer. If you know what is normal to you, you will be able to judge what is unusual.
- Note that problems like breast imbalance, meaning that one side is slightly different in size or in a different position, are usually not of concern either. It is worrisome when there is a change from the normal condition (for example, a noticeably larger developed breast and so on).
- If you have a partner, ask them to participate in the screening process to become more aware of the breast condition together. This is especially important because they see and touch your body from a different angle and can see places you don't see. Ask them to report any noticeable or palpable changes.

Breast self-examination is also a controversial issue. In the past all women were encouraged to do monthly breast self-exams. However, in 2009, the US Preventive Services Task Force recommended against directing women to do breast self-exams after many large studies concluded that breast self-exams did not reduce deaths and also there is no increase in cancer cases detected. Subsequent studies confirmed that self-examination did not play an important role in detecting malignancies in the breast.- The American Cancer Society and the American Preventive Services Task Force are now recommending everyone to consider having a breast self-exam. They also emphasize that the real key is knowing what's normal with your breasts.
- Part of the reason for the stance against breast self-examination is the possibility of unnecessary testing (such as a biopsy), which is detrimental to the patient as well as an additional financial burden. Medical care system. The problem is that after self-examination one can notice benign tumors, while a mammogram can identify a malignant tumor that is the real cause of concern and treatment.
- You should also know that self-examination is never a substitute for a clinical examination or a mammogram. The benefit of a self-exam is to help you better know what is normal with your breasts to assist your doctor in detecting changes.

Know what to pay attention to. There are a few signs you should look for when examining your breasts with your eyes or hands for cancer, including:- Change the size and shape of the breast - Swelling caused by tumor or infection can change the shape and size of the breast. This usually occurs on only one breast, but in some cases can occur in both. Breasts also change in size at some point in the menstrual cycle, so knowing what's "normal" for you at a specific time of the month is also helpful.
- Nipple discharge - If you don't breastfeed, your nipples will not produce discharge. If you have a discharge, especially when you don't need to squeeze your nipple or breast tissue, let your doctor know.
- Swelling - Increased and invasive breast cancer also causes the chest, area around the collarbone or the armpit to swell. In some cases, swelling occurs before a lump can be felt.
- Sunken - Lumps in the breast near the surface of the skin or the nipple may cause a change in the shape of the breast, such as a sunken or wrinkled skin (like an orange peel). Note that when a new nipple is indented, this is also a worrying sign. (Some women have naturally recessed nipples, this is not a concern, only a change in the normal state is of concern.)
- Redness, warmth, or itching Inflammatory breast cancer is a rare form but is an advanced cancer that presents with symptoms similar to that of breast infection: warmth, itching, or redness.
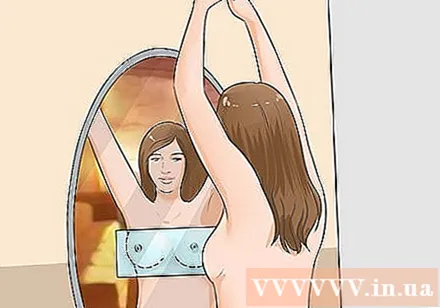
Eye self-examination. You can take the test whenever you want, although it's better that after your period is over, your breasts are less painful to the touch and less swollen. Try to check in every month at the same time. You should even make notes in the diary every time you check for convenience.- Sit or stand in front of a mirror, wearing no blouse or bra. Raise and lower your arms. Look for changes in the size, shape, tenderness and appearance of breast tissue, and then use these markers to evaluate.
- Next, place your palms on your hips and bend your chest muscles, looking for sunken spots, wrinkles or other abnormalities.
Self-examination of the breasts by hand. Set aside a set time each month to check your breasts manually. If you are still having a period, the best time is a few days after your period is over, at which point your breasts will be least tender. You should perform a lying test because in this position the breast tissue is more stretched, so it will be thin and easy to feel by hand. Another way is to check in the shower, where soap and water help you move your fingers across your skin. You can test using both methods to maximize accuracy. Follow these steps:
- Lie flat and place your right hand under your head. Use the first three fingers of the left hand to feel the muscle tissue of the right breast. Remember to use the inside of your fingers, not just the tips. Find anything that feels stiff and round inside the breast.
- Start in the armpits and work towards the midpoint of each breast. Move your hand across the middle part of your body until you feel the sternum.
- Use three different levels of force to feel the breast: gentle pressure on the surface examining the tissue just below the skin, moderate pressure to examine the tissue in the middle of the breast, and stronger pressure to feel the tissue close to the chest wall. You must check each area with the correct pressure before proceeding.
- After examining one breast, continue with the other. Place your left hand under your head and perform the same test on your left breast.
- Squeeze each nipple gently to see if there is a discharge.
- Remember that breast tissue extending to the area near the armpit can also develop tumors or cancer so you should also consider this during manual examination.
Method 2 of 4: Schedule a breast clinic
Annual "checkup". You usually have a well-exam each year that includes a pelvic exam with your general practitioner and gynecologist. You should attend this routine checkup even though you still feel fine. This is especially important because as age increases, the risk of developing certain cancers including breast cancer increases.
- At the time of your visit, let your doctor know about your most recent medical history. Breast cancer is often inherited, so breast exams will be even more necessary if your family has a history of breast cancer, especially in a mother or sister.
Clinical examination of the mammary glands. During a routine checkup, your doctor will usually examine your breast manually for suspicious lumps or any changes. If the doctor does not, then you should ask. They know how to check the breasts, understand what to look for and what to look for. That is why you should never replace this checkup with one of your own.
- If you are concerned you can have a nurse or family member present at the exam. If you are seeing a male doctor, this is a common procedure.
Evaluate the breast appearance. The doctor first looks at the outside of the breast, they will ask you to raise your arms above your head, then let your arms drop while checking the size and shape of the breast.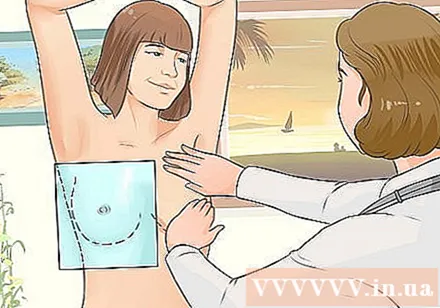
- They don't comment on any of your breast's aesthetic features, but check to see if the breasts are the same size and size, or if there are areas of concern.
Check the health of the mammary glands. While you lie on the examination table, the doctor uses the inside of his fingers to examine the entire chest area, including the armpits and collarbones. Exam time only lasts a few minutes.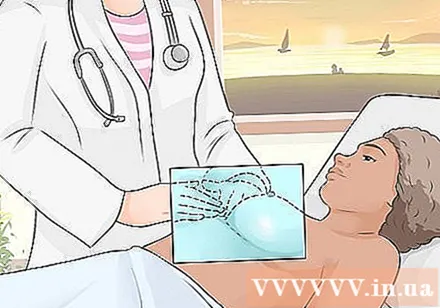
Keep calm and breathe. If you feel restless, take a deep breath and remind yourself that this is an essential process to maintain and take initiative in your health.
- Remember, breast cancer has a higher rate of success if detected early, before it spreads to other organs, tissues, and bones.
- You can always check with your doctor about why they are performing a particular exercise. If you feel stressed or uncomfortable, let your doctor know.
Method 3 of 4: Mammogram
Get a mammogram every year when you turn 40. The National Breast Cancer Foundation recommends that women get mammograms every 1-2 years after turning 40. If you have had breast cancer, have a family history of this disease or feel lumps. On self-examination, you should start having mammograms before you reach 40 years of age.
- Screening of the mammary glands of women 75 years of age and older depends on their general health. If there is a health problem, even if cancer is found, they are not subject to treatment. So you should consult your doctor about screening if you are over the age of 75.
- Through genetic testing, if you carry a mutation that causes cancer (BRCA1 and BRCA2 genes), you should have a screening exam from the age of 25, and combine an MRI of breast tissue next to a mammogram.
Understand the benefits of a mammogram. This is a scan that uses low-intensity x-rays and allows the doctor to see breast tissue. It is common to find a lump in the breast before you can feel it through photographs.
- Although doctors often purposefully look for tumors that can cause cancer, but scans also help detect calcification, fibroids and cysts in the breast.
Prepare before having a mammogram. Ask your doctor for requirements to do before an x-ray. You should not use deodorants, perfumes, or body oils on the day of your x-ray, as this may affect the quality of your photos.
- Wear a loose-fitting T-shirt for easy removal before shooting.
- If in doubt, learn more about x-ray techniques to feel more secure. This procedure is somewhat uncomfortable but lasts only a few minutes.
Talk to your doctor about a mammogram. They need to know if you have had breast implants or if you are menstruating.
Proceed to shoot. For this procedure you must place the breast on a flat surface and then the breast tissue is squeezed out by the propeller on top, keeping the tissue in place during the scan and allowing low-intensity x-rays to penetrate.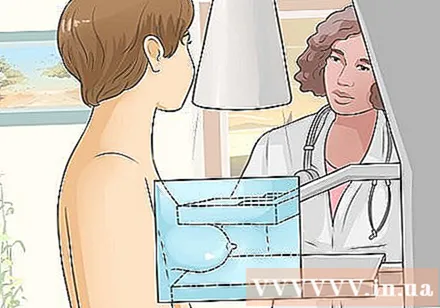
- You often feel pressure and discomfort during the shoot, but only temporarily.
- A mammogram is done on both breasts so the doctor can compare.
Wait for results. If the scans show possible breast cancer, you may need additional tests, such as an ultrasound to find a cyst or an MRI scan to evaluate and distinguish a suspicious tumor from a benign one.
- If the x-ray and MRI detect the tumor, the doctor will recommend a biopsy directed by ultrasound to determine the type of tumor cell and the necessary treatment (surgery, chemotherapy material, radiation and so on). To do a biopsy they must take tissue from an area of suspected cancer in the breast and analyze it in a laboratory. The breast biopsy procedure is usually outpatient and you do not have to stay in the hospital overnight.
Method 4 of 4: Identify risk factors
Understand the basic risk factors for breast cancer. Being a woman is the leading risk factor, but there are a number of other factors that increase your risk of developing breast cancer, including:
- Age: The risk increases with age. Most people with breast cancer are over 45 years old. Your chances of getting sick will increase 10 times every decade since you turn 50.
- Periods: If you started menstruating before age 12 or entered menopause after passing age 55, your risk is slightly higher. In both of these cases, the more fertile cycle is the cause of the increased risk.
- Pregnant: Both early pregnancy or multiple pregnancies reduce the risk of breast cancer. Not having a baby or getting pregnant after age 40 increases your risk.
- Hormone replacement therapy (HRT): Currently or having been using this therapy for more than 10 years may increase your risk of breast cancer.
Lifestyle also affects your chances of getting sick. Obesity, smoking, drinking, and shift work are all risk factors.
- To find out if you are overweight or obese you can use the Body Mass Index (BMI). BMI is calculated by dividing body mass (kg) by square of height (m). A BMI of 25-29.9 is considered overweight and over 30 is obese. BMI over 30 is considered a risk factor for breast cancer because fat cells secrete estrogen, the hormone that feeds breast cancer cells.
- There is recently some evidence that long-term heavy smoking is associated with an increased risk of breast cancer. The risk is particularly high for certain groups of people, such as women who started smoking before their first birth. Currently, work is still being done to determine the exact relationship between smoking and breast cancer.
- Alcohol has also been linked to an increased risk of developing breast cancer, the more you drink, the higher the risk. Women who drink 700-1750 ml of beer (5% alcohol) per day are 1.5 times more likely to be drinking beer.
- Recent research shows that women who work the night shift (such as nurses) may have a higher risk of breast cancer because of varying melatonin levels. However, more research is needed to be able to formally conclude these findings.
Personal and family medical history. There are also a number of risk factors associated with yourself, a family history of the disease and your genetics, including:
- Personal medical history: If you have been diagnosed with breast cancer in the past, the risk of developing cancer in that breast or the other breast is 3-4 times higher.
- Family history: Breast cancer is more likely to occur if you have one or more close family members who have had breast, ovarian, uterine or colon cancer. The risk doubles if you have a close relative (sister, mother, daughter) with the disease, and triples if two people have it.
- Genes: A genetic defect that occurs in the BRCA1 and BRCA2 genes also significantly increases the risk of developing breast cancer. To find out if you have these mutant genes you can contact a gene mapping service.In general, approximately 5-10% of cases are related to genetics.
Remember, most women diagnosed with breast cancer do NOT have any risk factors. Most do not exhibit any of the factors mentioned and are not more or less likely to develop breast cancer than others. So it is important that they follow the above guidelines on breast health and let their doctor know if any breast changes are detected. advertisement
Advice
- Remember that all breast exams including self-exams, physical exams, or mammograms are not perfect. They can give false positive or negative results. Consult with your doctor about all treatment options and the likelihood of success.
- A mammogram or screening is not usually helpful for men. However, if you are a man and a family of people with breast cancer, you should consult your doctor to learn how to self-check for early warning signs.
Warning
- Always have a doctor diagnose your condition. You cannot diagnose breast cancer at home or based on self-tests. So you should not worry too much before finding the correct answer to make the right decision.