Content
- Steps
- Part 1 of 3: Giving insulin with a syringe
- Part 2 of 3: Giving insulin with an insulin pen
- Part 3 of 3: Find out exactly how much insulin you need
- Tips
- A warning
Insulin is a hormone produced by the pancreas that moves glucose (sugar) from the bloodstream to the cells in the body, which use glucose for energy. In people with diabetes, insulin is either not produced at all (type 1 diabetes) or not enough (type 2 diabetes). For this reason, diabetics require daily injections of synthetic insulin. In addition, they should follow a specific diet and exercise regularly. If you or your child have diabetes and need to inject insulin on a regular basis, you will need to learn how to properly administer insulin injections. Before you start injecting yourself, you should seek the advice of your doctor. Your healthcare provider will show you how to inject correctly. In addition, only a doctor will be able to determine what dose of insulin you need to inject daily, and will also help you choose the best way to administer this drug.
Steps
Part 1 of 3: Giving insulin with a syringe
 1 Prepare everything you need for injection. Before injecting yourself or your child, you will need to prepare a small glass container of insulin (vial), a syringe, and alcohol wipes for injection. Check the label on the drug vial to make sure you are taking the correct type of insulin. Insulin medications vary in duration of action; they are of three types: short-acting, medium-acting and long-acting. Your healthcare provider will prescribe the type of insulin that's right for you. There are several ways to administer the drug: using syringes of various sizes, an insulin pen, a pump, or a needleless insulin injector.
1 Prepare everything you need for injection. Before injecting yourself or your child, you will need to prepare a small glass container of insulin (vial), a syringe, and alcohol wipes for injection. Check the label on the drug vial to make sure you are taking the correct type of insulin. Insulin medications vary in duration of action; they are of three types: short-acting, medium-acting and long-acting. Your healthcare provider will prescribe the type of insulin that's right for you. There are several ways to administer the drug: using syringes of various sizes, an insulin pen, a pump, or a needleless insulin injector. - Most often, insulin is injected using syringes. They are inexpensive and are provided free of charge to patients under the Free Health Care program.
- Syringes vary in volume and needle diameter. Most often, syringes are made of plastic (disposable) and the needle is already attached to the tip of the syringe.
- There is a general rule for choosing the right syringe: if you need to inject from 50 to 100 units of insulin, use a 1 ml syringe; if a single dose is from 30 to 50 units, the volume of the syringe is 0.5 ml. If you inject less than 30 units at a time, take a 0.3 ml syringe.
- The usual needle length for an insulin syringe is 12.7 mm, but shorter needles (4 to 8 mm) are equally effective and cause less discomfort during injection.
 2 Take your insulin out of the refrigerator. Insulin vials are usually kept in the refrigerator.At low temperatures, insulin does not deteriorate and does not lose its effectiveness, and with such storage, this hormone retains its properties longer. However, for the introduction of insulin, the drug solution must be at room temperature. Therefore, you need to take the bottle out of the refrigerator about 30 minutes before the injection time so that the liquid in the bottle has time to warm up to room temperature. Never place a bottle in a microwave oven or boiling water to warm the insulin solution quickly. When heated, the hormone is destroyed.
2 Take your insulin out of the refrigerator. Insulin vials are usually kept in the refrigerator.At low temperatures, insulin does not deteriorate and does not lose its effectiveness, and with such storage, this hormone retains its properties longer. However, for the introduction of insulin, the drug solution must be at room temperature. Therefore, you need to take the bottle out of the refrigerator about 30 minutes before the injection time so that the liquid in the bottle has time to warm up to room temperature. Never place a bottle in a microwave oven or boiling water to warm the insulin solution quickly. When heated, the hormone is destroyed. - When a cold insulin solution is injected, the person experiences more discomfort. In addition, with the introduction of a cold drug, the effectiveness of insulin decreases slightly. For best results, always add a solution at room temperature.
- Once you have opened the bottle and started using insulin, you can store it at room temperature. The drug can be stored under such conditions for at least a month, during which the insulin retains all its properties and does not deteriorate.
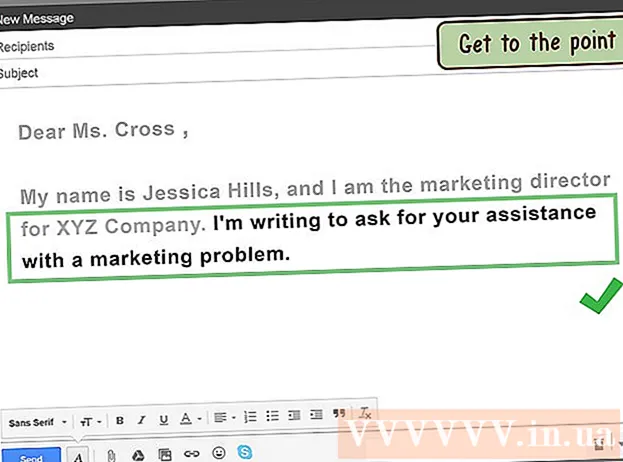
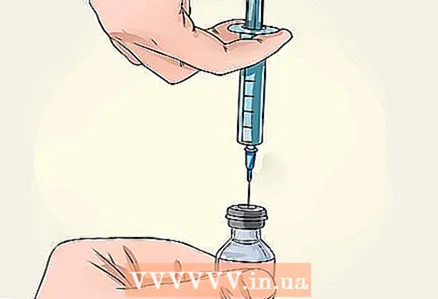 3 Draw the same type of insulin into the syringe. Before drawing insulin into the syringe, carefully read the label on the vial to make sure you have the correct type of insulin and to check the expiration date of the drug. The insulin solution should be clear, without any flakes or sediment. Wash your hands thoroughly before removing the plastic packaging from the bottle. Then wipe the top of the bottle with an alcohol wipe to disinfect the surface. After that, remove the protective cap from the syringe needle and pull the syringe plunger up to the mark that corresponds to the required volume of insulin solution. Pierce the rubber cap of the vial with a needle and push the syringe plunger down until it stops. While holding the needle inside the bottle, turn the bottle upside down, then pull the plunger out again to draw the required dose of insulin into the syringe.
3 Draw the same type of insulin into the syringe. Before drawing insulin into the syringe, carefully read the label on the vial to make sure you have the correct type of insulin and to check the expiration date of the drug. The insulin solution should be clear, without any flakes or sediment. Wash your hands thoroughly before removing the plastic packaging from the bottle. Then wipe the top of the bottle with an alcohol wipe to disinfect the surface. After that, remove the protective cap from the syringe needle and pull the syringe plunger up to the mark that corresponds to the required volume of insulin solution. Pierce the rubber cap of the vial with a needle and push the syringe plunger down until it stops. While holding the needle inside the bottle, turn the bottle upside down, then pull the plunger out again to draw the required dose of insulin into the syringe. - The short-acting insulin solution is completely transparent and should not contain any undissolved particles. Do not use the drug if flakes or separate undissolved particles are visible in the vial.
- Medium-acting insulin is a cloudy suspension. Before use, the bottle with the drug must be rolled between the palms so that the suspension becomes homogeneous. It is not necessary to shake the bottle vigorously, as this can lead to the formation of large flakes.
- Check for air bubbles in the syringe. If you notice bubbles in the syringe, gently tap on the barrel so that the bubbles rise to the point of attachment of the needle, and then by lightly pressing the plunger, squeeze the air from the syringe back into the vial.
- When there are no air bubbles left in the syringe, carefully remove the filled syringe from the vial and proceed to choosing the injection site.
 4 Filling the syringe with two types of insulin. Some types of insulin can be mixed with each other. You need to know that not all types of this drug can be mixed, so you need to do this only as directed by a doctor, while you must be shown how exactly insulins are mixed. The doctor should explain to you in what proportions you need to mix different types of insulin. In this case, you need to calculate how much the total volume of solution is obtained by adding the assigned volumes of each type, and then "charge" the syringe according to the scheme described above. In addition, your doctor will explain to you which type of insulin you should draw first, and you should definitely follow this prescription. Typically, short-acting insulin is drawn into the syringe earlier than medium-duration insulin, and long-acting insulin, respectively, after medium-duration insulin.
4 Filling the syringe with two types of insulin. Some types of insulin can be mixed with each other. You need to know that not all types of this drug can be mixed, so you need to do this only as directed by a doctor, while you must be shown how exactly insulins are mixed. The doctor should explain to you in what proportions you need to mix different types of insulin. In this case, you need to calculate how much the total volume of solution is obtained by adding the assigned volumes of each type, and then "charge" the syringe according to the scheme described above. In addition, your doctor will explain to you which type of insulin you should draw first, and you should definitely follow this prescription. Typically, short-acting insulin is drawn into the syringe earlier than medium-duration insulin, and long-acting insulin, respectively, after medium-duration insulin. - Since the short-acting insulin solution is clear and the long-acting insulin is cloudy, you can memorize the syringe filling sequence using the mnemonic rule: "Clear at the beginning, cloudy at the end."
- Mixing different types of insulins is necessary to provide a combined effect of insulins on high blood glucose levels.
- When using a syringe, you can mix different types of insulin, while other injection methods (such as an insulin pen) do not.
- The introduction of a mixture of different types of insulin for an effective therapeutic effect is shown only in some forms of diabetes. In addition, some patients find this method too complicated and time-consuming. Typically, this method is used when diabetes progresses over time and the patient needs a higher dose of insulin to provide a therapeutic effect.
- The doctor who prescribes insulin for you must teach you how to administer the drug. You will have the opportunity to learn this method under the guidance of a healthcare professional, and only then can you inject yourself.
 5 Choose where you will inject the hormone. Insulin needs to be injected into the fatty tissue just under the skin. This layer is called subcutaneous fat. That is why areas of the body are chosen for injections, which are characterized by significant development of this layer. Most often, the injection is done in the abdomen, thighs, buttocks, and the inner surface of the upper arm. People who inject insulin daily should remember to change the injection site from time to time to prevent tissue damage called lipodystrophy. You can give injections in different parts of the same area of the body (in this case, it is necessary that there is at least 2.5 cm between the injection points). In addition, you can change the area of the body where you are injecting the drug from time to time.
5 Choose where you will inject the hormone. Insulin needs to be injected into the fatty tissue just under the skin. This layer is called subcutaneous fat. That is why areas of the body are chosen for injections, which are characterized by significant development of this layer. Most often, the injection is done in the abdomen, thighs, buttocks, and the inner surface of the upper arm. People who inject insulin daily should remember to change the injection site from time to time to prevent tissue damage called lipodystrophy. You can give injections in different parts of the same area of the body (in this case, it is necessary that there is at least 2.5 cm between the injection points). In addition, you can change the area of the body where you are injecting the drug from time to time. - If you inject insulin deeper into muscle tissue, the hormone is absorbed too quickly, which can lead to too much lowering of glucose levels and the development of a potentially dangerous condition - hypoglycemia.
- If you give injections to the same area too often, this can provoke the development of lipodystrophy, when the layer of subcutaneous adipose tissue either becomes thinner or, conversely, develops excessively. This must be taken into account as lipodystrophy affects the absorption of insulin. If you inject insulin into an area affected by lipodystrophy, the active ingredient does not have the desired effect on blood glucose levels. That is why the injection site must be changed periodically.
- The insulin injection site should be at least 2.5 centimeters from any scars and more than 5 centimeters above the lower abdomen. Never inject into a sensitive area or areas with swelling or bruising.
 6 Inject insulin. Once you have chosen the injection site, you need to give it an insulin injection. The skin area must be absolutely clean. If you are in doubt about the cleanliness of your skin, wash it with soap and water (but do not wipe it with an alcohol solution). Gather the fold with two fingers, grasping the skin and the subcutaneous fat underneath. Pull back the fold slightly so that it moves away from the muscle layer. Insert the needle into the crease at a 90 degree angle (perpendicular to the skin surface if the crease is thick enough). If the fat layer is underdeveloped (which is typical for type 1 diabetes), insert the needle at a 45-degree angle to reduce discomfort at the injection site. Insert the needle completely under the skin, then release the skin fold. Press down on the plunger slowly and evenly until there is no solution in the syringe.
6 Inject insulin. Once you have chosen the injection site, you need to give it an insulin injection. The skin area must be absolutely clean. If you are in doubt about the cleanliness of your skin, wash it with soap and water (but do not wipe it with an alcohol solution). Gather the fold with two fingers, grasping the skin and the subcutaneous fat underneath. Pull back the fold slightly so that it moves away from the muscle layer. Insert the needle into the crease at a 90 degree angle (perpendicular to the skin surface if the crease is thick enough). If the fat layer is underdeveloped (which is typical for type 1 diabetes), insert the needle at a 45-degree angle to reduce discomfort at the injection site. Insert the needle completely under the skin, then release the skin fold. Press down on the plunger slowly and evenly until there is no solution in the syringe. - When you inject the drug, place the used needle and / or syringe in a special plastic container and keep it out of the reach of children. Never reuse needles and syringes.
- Regularly keep records of which areas of your body you injected on that day.Your healthcare provider may recommend a pictorial table or graphical diagram to help you keep your records.
 7 Do not pull the needle out from under your skin for 5 seconds. After injecting insulin, leave the syringe in the same place for a while without removing the needle from under the skin. This will allow the hormone to be absorbed into the tissue in full and will not allow the injected solution to flow out of the wound. As long as the needle remains under the skin, try to keep the part of the body where you are giving the injection still to prevent discomfort. If the sight of the needle makes you fearful and trembling in your knees, look away and do not look at the syringe for these 5 seconds and only then carefully pull the needle out.
7 Do not pull the needle out from under your skin for 5 seconds. After injecting insulin, leave the syringe in the same place for a while without removing the needle from under the skin. This will allow the hormone to be absorbed into the tissue in full and will not allow the injected solution to flow out of the wound. As long as the needle remains under the skin, try to keep the part of the body where you are giving the injection still to prevent discomfort. If the sight of the needle makes you fearful and trembling in your knees, look away and do not look at the syringe for these 5 seconds and only then carefully pull the needle out. - If you notice that the insulin solution is leaking from the wound, take a clean cloth and press firmly to the injection site for 5-10 seconds. During this time, the adipose tissue absorbs the hormone, and it will cease to protrude from the wound.
- Remember to remove the needle at the same angle as you inserted it (90 or 45 degrees) to prevent tissue damage.
Part 2 of 3: Giving insulin with an insulin pen
 1 Consider using a special insulin pen instead of a syringe. Contrary to popular belief, a person does not experience significant pain when injecting insulin with an ordinary syringe. However, administering the hormone with an insulin pen is more convenient and less discomforting. In addition, with this method, there is no need to draw the solution from the vial with a needle; The required dose is easy to draw into the pen, and the pen is suitable for most types of insulin delivery. The main disadvantage of this method is that you will not be able to mix different types of insulin in the pen, if the doctor prescribed you just such an injection of the drug.
1 Consider using a special insulin pen instead of a syringe. Contrary to popular belief, a person does not experience significant pain when injecting insulin with an ordinary syringe. However, administering the hormone with an insulin pen is more convenient and less discomforting. In addition, with this method, there is no need to draw the solution from the vial with a needle; The required dose is easy to draw into the pen, and the pen is suitable for most types of insulin delivery. The main disadvantage of this method is that you will not be able to mix different types of insulin in the pen, if the doctor prescribed you just such an injection of the drug. - The pen syringe is the best choice for school children who need insulin injections at school. The pen is easy to take with you and your child does not need to take insulin out of the refrigerator.
- Today, there are different models of syringe pens on sale. You need to choose the one that suits your needs. There are both disposable pens and models with replaceable needles and cartridges.
- Syringe pens and cartridges for them are usually more expensive than conventional syringes and insulin in vials.
 2 Prepare a pen syringe. Check the pen to make sure the drug matches your prescription and is within the expiration date. Wipe the tip of the pen with an alcohol wipe. Remove the protective cap from the needle and screw it onto the handle. Your doctor must write you a prescription for both the pen and the needles.
2 Prepare a pen syringe. Check the pen to make sure the drug matches your prescription and is within the expiration date. Wipe the tip of the pen with an alcohol wipe. Remove the protective cap from the needle and screw it onto the handle. Your doctor must write you a prescription for both the pen and the needles. - If you are injecting short-acting insulin, the drug solution should be completely clear and free of any particles, cloudiness or discoloration. Open the handle. A needle appears, which you need to wipe with an alcohol wipe for injection.
- The intermediate and long acting insulin solution is cloudy and must be shaken gently before injection. Roll the pen gently between your palms and turn the pen up and down ten times to mix the solution properly.
 3 Remove the cap. Remove the outer needle cap, which you can reuse, and the inner cap, which you will need to discard. Never use the injection needle multiple times. ,
3 Remove the cap. Remove the outer needle cap, which you can reuse, and the inner cap, which you will need to discard. Never use the injection needle multiple times. ,  4 Prepare the handle mechanism. Hold the pen up with the needle. Tap the housing gently so that any air bubbles that may be in the handle rise upward. Turn the dosage selector, which is usually located next to the start button, to position "2". Then press the trigger and hold until a drop of solution appears at the tip of the needle.
4 Prepare the handle mechanism. Hold the pen up with the needle. Tap the housing gently so that any air bubbles that may be in the handle rise upward. Turn the dosage selector, which is usually located next to the start button, to position "2". Then press the trigger and hold until a drop of solution appears at the tip of the needle. - If air bubbles remain inside the pen, this could cause you to inject the wrong amount of insulin.
 5 Select the correct dose of insulin. The dose selector, located at the end of the handle, near the piston, will help you do this. You will be able to control how much insulin you give. Set the dosage indicator to the amount of insulin your doctor has prescribed for you.
5 Select the correct dose of insulin. The dose selector, located at the end of the handle, near the piston, will help you do this. You will be able to control how much insulin you give. Set the dosage indicator to the amount of insulin your doctor has prescribed for you.  6 Choose where you will inject the hormone. Insulin needs to be injected into the fatty tissue just under the skin. This layer is called subcutaneous fat. That is why areas of the body are chosen for injections, which are characterized by significant development of this layer. Most often, the injection is done in the abdomen, thighs, buttocks, and the inner surface of the upper arm. People who inject insulin daily should remember to change the injection site from time to time to prevent tissue damage called lipodystrophy. You can give injections in different parts of the same area of the body (in this case, it is necessary that there should be at least 2.5 cm between the injection sites). In addition, you can change the area of the body where you are injecting the drug from time to time.
6 Choose where you will inject the hormone. Insulin needs to be injected into the fatty tissue just under the skin. This layer is called subcutaneous fat. That is why areas of the body are chosen for injections, which are characterized by significant development of this layer. Most often, the injection is done in the abdomen, thighs, buttocks, and the inner surface of the upper arm. People who inject insulin daily should remember to change the injection site from time to time to prevent tissue damage called lipodystrophy. You can give injections in different parts of the same area of the body (in this case, it is necessary that there should be at least 2.5 cm between the injection sites). In addition, you can change the area of the body where you are injecting the drug from time to time. - If you inject insulin deeper into the muscle tissue, it will be absorbed too quickly, which can lead to a dangerous drop in glucose levels (hypoglycemia).
- If you give injections to the same area too often, this can provoke the development of lipodystrophy, when the layer of subcutaneous adipose tissue either becomes thinner or, conversely, develops excessively.
- The insulin injection site should be at least 2.5 centimeters from any scars and more than 5 centimeters above the lower abdomen. Never inject into a sensitive area or areas with swelling or bruising.
 7 Get an injection. Grasp the body of the pen with your fingers, and place your thumb on the start button. Place the needle against the folded skin with the fingers of your other hand. The needle should be at an angle of 45 or 90 degrees to the surface of the skin (ask your doctor at what angle it is recommended to insert the needle with your type of pen). Press the start button and hold it for at least 10 seconds.
7 Get an injection. Grasp the body of the pen with your fingers, and place your thumb on the start button. Place the needle against the folded skin with the fingers of your other hand. The needle should be at an angle of 45 or 90 degrees to the surface of the skin (ask your doctor at what angle it is recommended to insert the needle with your type of pen). Press the start button and hold it for at least 10 seconds.  8 Dispose of the used needle. Put the protective cap on the needle and unscrew it from the pen. The needle should be discarded, but do not throw away the insulin pen itself until it runs out of insulin solution. Typically, the pen contains enough insulin to deliver over 28 days, but this period may vary depending on the type of insulin. Never leave the needle in the pen until the next injection.
8 Dispose of the used needle. Put the protective cap on the needle and unscrew it from the pen. The needle should be discarded, but do not throw away the insulin pen itself until it runs out of insulin solution. Typically, the pen contains enough insulin to deliver over 28 days, but this period may vary depending on the type of insulin. Never leave the needle in the pen until the next injection. - As with using a syringe, you need to determine a special place where you will store your used needles. Store them in a special container made of metal or thick plastic (remember to affix the warning label on it). When the container is full, secure the lid with tape and dispose of the container according to the rules for medical waste disposal. You can go to a healthcare facility and learn how to dispose of sharps.
Part 3 of 3: Find out exactly how much insulin you need
 1 Difference between the two types of diabetes. Diabetes is a condition in which blood glucose (sugar) levels are higher than normal levels. This condition is called hyperglycemia and is caused by a lack of insulin or an impaired tissue sensitivity to this hormone. In general, type 1 diabetes is considered a more serious condition because the pancreas is then unable to produce insulin. In type 2 diabetes, the body does not use insulin efficiently or produces insufficient amounts of it. If left untreated, both forms of diabetes can lead to death.
1 Difference between the two types of diabetes. Diabetes is a condition in which blood glucose (sugar) levels are higher than normal levels. This condition is called hyperglycemia and is caused by a lack of insulin or an impaired tissue sensitivity to this hormone. In general, type 1 diabetes is considered a more serious condition because the pancreas is then unable to produce insulin. In type 2 diabetes, the body does not use insulin efficiently or produces insufficient amounts of it. If left untreated, both forms of diabetes can lead to death. - For all forms of type 1 diabetes, patients need to inject themselves with insulin daily.Type 2 diabetes can often be compensated for with diet, exercise and weight loss.
- Type 2 diabetes is much more common than type 1 diabetes and is associated with obesity. Obesity causes a decrease in the sensitivity of body tissues to the effects of insulin - a significant resistance to its effects.
- Insulin cannot be taken in pill form (by mouth) to lower blood glucose levels. The enzymes in saliva affect the action of this hormone.
 2 Recognize the symptoms of type 1 diabetes. In people with type 2 diabetes, symptoms of the disease increase gradually, and this form of the disease is usually associated with being overweight. Type 1 diabetes develops very quickly and its symptoms are much stronger. The most common symptoms of this type of diabetes include: increased thirst, frequent urination, severe hunger, unexplained weight loss, sweet breath smell (due to ketone bodies), extreme tiredness, irritability, blurred vision, slow healing wounds, and frequent infections.
2 Recognize the symptoms of type 1 diabetes. In people with type 2 diabetes, symptoms of the disease increase gradually, and this form of the disease is usually associated with being overweight. Type 1 diabetes develops very quickly and its symptoms are much stronger. The most common symptoms of this type of diabetes include: increased thirst, frequent urination, severe hunger, unexplained weight loss, sweet breath smell (due to ketone bodies), extreme tiredness, irritability, blurred vision, slow healing wounds, and frequent infections. - Type 1 diabetes can develop at any age, but it usually appears during childhood or adolescence. Children with diabetes tend to look thin, tired and haggard.
- Type 2 diabetes can develop at any age, but it usually occurs in obese people over the age of 40.
- Without insulin therapy, diabetes will rapidly progress and the patient may develop severe organ damage such as damage to the nervous system (neuropathy), heart disease, kidney damage, blindness, poor circulation in the extremities, and various skin conditions.
 3 Learn more about the risks of insulin injections. If a person has diabetes and needs daily insulin injections, it sometimes feels like balancing on a tightrope. Injecting too much insulin can cause hypoglycemia because too much glucose is excreted from the bloodstream. On the other hand, if not enough insulin is injected, it can lead to the development of hyperglycemia due to the large amount of glucose remaining in the blood. Your doctor can calculate the optimal amount of the hormone, but in practice it depends on your diet. For this reason, people with diabetes must independently measure their blood glucose levels and determine exactly when to inject the drug.
3 Learn more about the risks of insulin injections. If a person has diabetes and needs daily insulin injections, it sometimes feels like balancing on a tightrope. Injecting too much insulin can cause hypoglycemia because too much glucose is excreted from the bloodstream. On the other hand, if not enough insulin is injected, it can lead to the development of hyperglycemia due to the large amount of glucose remaining in the blood. Your doctor can calculate the optimal amount of the hormone, but in practice it depends on your diet. For this reason, people with diabetes must independently measure their blood glucose levels and determine exactly when to inject the drug. - Hypoglycemia manifests itself in the following symptoms: increased sweating, trembling, weakness, hunger, dizziness, headache, blurred vision, increased heart rate, irritability, slurred speech, drowsiness, confusion, fainting, and seizures.
- Skipping meals or exercising too much can also lead to hypoglycemia.
- You can cope with an attack of hypoglycemia on your own. To do this, you need to eat foods rich in easily digestible carbohydrates, for example, drink fruit juice, eat a ripe fruit or a slice of white bread with honey. Alternatively, you can take glucose tablets with or separately.
Tips
- Many people choose to inject insulin into their abdomen. Such an injection is less painful, and the active substance is absorbed faster and in the correct amount.
- If you are injecting into the buttocks, do not put the needle into the part where you are sitting. On the contrary, try to inject into the upper part of the buttocks. To locate the correct injection site, imagine where the back pockets of the jeans are located.
- If you apply an ice cube to the skin 1-2 minutes before the injection, it will reduce the sensitivity of the skin in this area and significantly reduce the pain during the injection.
- Dispose of needles properly after injection. Place the cap over the used needle.Store used needles together with the caps in a small box, glass jar or container. When the container is full, close the lid tightly and wrap the container of needles in a plastic bag. Then you can throw the container of needles in the trash. Never dispose of used needles without caps in the trash.
A warning
- This article is for educational purposes only. Check with your healthcare provider or diabetes care specialist for advice that is right for you.