Author:
Clyde Lopez
Date Of Creation:
18 June 2021
Update Date:
1 July 2024
Content
- Steps
- Part 1 of 4: How to Ease Pain
- Part 2 of 4: How to Improve Nutrition
- Part 3 of 4: How to Follow a Low FODMAP Diet
- Part 4 of 4: Understanding IBS Symptoms and Risk Factors
- Tips
- Warnings
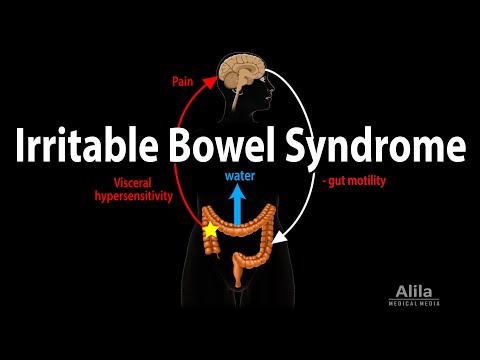
We all suffer from diarrhea or constipation from time to time, but irritable bowel syndrome (IBS) can turn these digestive disorders into a daily problem. IBS is a chronic disorder of the colon. Although IBS resembles a disease, it does not cause any noticeable changes in the colon. In fact, irritable bowel syndrome describes a whole range of symptoms. There are three types of IBS: diarrhea-predominant IBS (IBS-D), constipation-predominant IBS (IBS-C), and mixed IBS when constipation alternates with diarrhea (IBS-C). Since IBS is not a disease in the strict sense of the word, your doctor may recommend that you change your diet to relieve your symptoms.
Steps
Part 1 of 4: How to Ease Pain
 1 Apply warm compresses. The pain of IBS-induced cramps can be reduced by using heat. Apply a heating pad or heating pad to your stomach. This will relieve painful cramps. Keep the heating pad on your stomach for about 20 minutes. Never put a heating pad on bare skin.
1 Apply warm compresses. The pain of IBS-induced cramps can be reduced by using heat. Apply a heating pad or heating pad to your stomach. This will relieve painful cramps. Keep the heating pad on your stomach for about 20 minutes. Never put a heating pad on bare skin. - You can also take a hot bath to relieve pain. If your IBS is constipated, you can add Epsom salts to your bath.
 2 Take medication. Ask your doctor to prescribe medications for you to help relieve your symptoms. For constipation, your doctor may prescribe lubiprostone. If you are suffering primarily from diarrhea, your doctor may prescribe alosetron. For acute IBS, your doctor may recommend that you take small doses of an antidepressant, which will weaken the pain signals that travel from the gut to the brain rather than relieve the symptoms themselves.
2 Take medication. Ask your doctor to prescribe medications for you to help relieve your symptoms. For constipation, your doctor may prescribe lubiprostone. If you are suffering primarily from diarrhea, your doctor may prescribe alosetron. For acute IBS, your doctor may recommend that you take small doses of an antidepressant, which will weaken the pain signals that travel from the gut to the brain rather than relieve the symptoms themselves. - Alosetron is still the only drug approved for the treatment of IBS-D. It is believed to decrease the contractility of the colon. Alosetron can cause some serious side effects, such as ischemic colitis (insufficient blood supply to the intestines) and severe constipation, in which case hospital treatment may be required. In addition, it can interact with other medications, such as antihistamines and some antidepressants.
- You can also take over-the-counter medications, such as diarrhea medications, to relieve symptoms.
 3 Get exercise. Regular exercise promotes proper intestinal motility. Try moderate exercise for 30 minutes, five days a week, to help relieve stress, improve mood, and maintain optimal body weight, among other things. If you find that exercising is making your symptoms worse, consult a doctor who can help you choose a different type of exercise.
3 Get exercise. Regular exercise promotes proper intestinal motility. Try moderate exercise for 30 minutes, five days a week, to help relieve stress, improve mood, and maintain optimal body weight, among other things. If you find that exercising is making your symptoms worse, consult a doctor who can help you choose a different type of exercise. - Moderate exercise includes bicycling, brisk walking, water aerobics, and gardening.
- Train yourself to exercise regularly at the same time. For example, you can run daily before breakfast or swim in the pool on weekends.
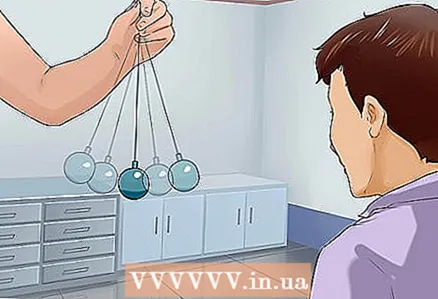 4 Learn to tolerate pain. If conventional pain relief methods are not working, you will have to deal with it with other methods. Learn to cope with pain through relaxation techniques or hypnotherapy. Cognitive behavioral therapy is also considered to be an effective method for managing pain in IBS. In addition, this therapy helps to reduce feelings of anxiety and anxiety caused by IBS symptoms.
4 Learn to tolerate pain. If conventional pain relief methods are not working, you will have to deal with it with other methods. Learn to cope with pain through relaxation techniques or hypnotherapy. Cognitive behavioral therapy is also considered to be an effective method for managing pain in IBS. In addition, this therapy helps to reduce feelings of anxiety and anxiety caused by IBS symptoms. - Unlike medication and dietary changes, these pain management methods have no side effects.
 5 Take peppermint oil. Peppermint oil capsules help relieve not only stomach pain from IBS, but also diarrhea and bloating. Follow the directions for use and adhere to the recommended dosage. Peppermint oil has long been used to calm the stomach and digestive system. This oil facilitates the elimination of gases from the intestines.
5 Take peppermint oil. Peppermint oil capsules help relieve not only stomach pain from IBS, but also diarrhea and bloating. Follow the directions for use and adhere to the recommended dosage. Peppermint oil has long been used to calm the stomach and digestive system. This oil facilitates the elimination of gases from the intestines. - In addition to peppermint, herbal teas can be used to relieve abdominal pain. Try teas with ginger, fennel, cinnamon and cardamom.
Part 2 of 4: How to Improve Nutrition
 1 Eat more soluble fiber. If your IBS is accompanied by diarrhea or constipation, eat soluble fiber. They dissolve in water, resulting in a thick jelly in the colon that slows down diarrhea. Soluble fiber also relieves constipation by making it easier to pass stools and relieving pain. The recommended amount of dietary fiber depends on age and gender. According to the Institute of Medicine (USA), the daily intake of dietary fiber should be about 25 and 38 grams for adult women and men, respectively. To provide your body with soluble dietary fiber, eat the following foods:
1 Eat more soluble fiber. If your IBS is accompanied by diarrhea or constipation, eat soluble fiber. They dissolve in water, resulting in a thick jelly in the colon that slows down diarrhea. Soluble fiber also relieves constipation by making it easier to pass stools and relieving pain. The recommended amount of dietary fiber depends on age and gender. According to the Institute of Medicine (USA), the daily intake of dietary fiber should be about 25 and 38 grams for adult women and men, respectively. To provide your body with soluble dietary fiber, eat the following foods: - Oatmeal
- Barley
- Okra (abelmos edible)
- Beans
- Legumes: chickpeas, lentils, soybeans
- Oat flakes
- Nuts and seeds
- Fruits: apples, peaches, berries
 2 Include insoluble fiber in your diet. If your IBS is mostly constipated, gradually increase your intake of insoluble fiber (those that don't dissolve in water). Increase the fiber content in your diet by 2-3 grams per week until you eat 25-60 grams per day. Increasing your intake of insoluble dietary fiber too dramatically can cause gas production. Dietary fiber supports the growth of beneficial gut bacteria, which improves bowel function. To increase your intake of insoluble dietary fiber, eat the following foods:
2 Include insoluble fiber in your diet. If your IBS is mostly constipated, gradually increase your intake of insoluble fiber (those that don't dissolve in water). Increase the fiber content in your diet by 2-3 grams per week until you eat 25-60 grams per day. Increasing your intake of insoluble dietary fiber too dramatically can cause gas production. Dietary fiber supports the growth of beneficial gut bacteria, which improves bowel function. To increase your intake of insoluble dietary fiber, eat the following foods: - Whole (unprocessed) grain foods: They contain both soluble and insoluble dietary fiber
- Carrot
- Zucchini
- Celery
- Flax seeds
- Beans
- Lentils
 3 Eat probiotics and prebiotics. Probiotics and prebiotics provide nutrition and support for beneficial gut bacteria. They also serve as protection against harmful bacteria that irritate the intestines. Since it is difficult to determine how many colony forming units (CFUs) are in a regular food, eat a variety of foods that contain probiotics and prebiotics. To include probiotics in your diet, eat green leafy vegetables (kale, spinach, beetroot, watercress, mustard greens), broccoli, cauliflower, and cabbage. Prebiotics are found in the following foods:
3 Eat probiotics and prebiotics. Probiotics and prebiotics provide nutrition and support for beneficial gut bacteria. They also serve as protection against harmful bacteria that irritate the intestines. Since it is difficult to determine how many colony forming units (CFUs) are in a regular food, eat a variety of foods that contain probiotics and prebiotics. To include probiotics in your diet, eat green leafy vegetables (kale, spinach, beetroot, watercress, mustard greens), broccoli, cauliflower, and cabbage. Prebiotics are found in the following foods: - Chicory root
- Jerusalem artichoke
- Dandelion leaves
- Garlic
- Leek
- Asparagus
- Wheat bran
- Wheat Flour Baking
- Bananas
 4 Choose the right probiotic supplement. Look for a supplement that contains many different strains of beneficial bacteria (at least L. acidophilus, L. Fermentum, L. rhamnosus, B. longum and B. bifidum). Some supplements contain yeast Saccharomyceswhich serves as a defense for beneficial gut bacteria. These supplements can be taken in any form: solution, capsule, tablet, or powder. Choose Dissolution Controlled Supplements so they don't dissolve in the stomach prematurely.
4 Choose the right probiotic supplement. Look for a supplement that contains many different strains of beneficial bacteria (at least L. acidophilus, L. Fermentum, L. rhamnosus, B. longum and B. bifidum). Some supplements contain yeast Saccharomyceswhich serves as a defense for beneficial gut bacteria. These supplements can be taken in any form: solution, capsule, tablet, or powder. Choose Dissolution Controlled Supplements so they don't dissolve in the stomach prematurely. - Specialists often recommend nutritional supplements from brands such as Florastor and Align.
- Check the expiration date and make sure the supplement contains at least 25 billion colony forming units (CFU). The daily allowance for adults is 10-20 billion CFU.
- Choose nutritional supplements that are approved by the Ministry of Health or other well-known and reputable organizations.
 5 Supplement your diet with unpasteurized fermented foods. Fermented foods promote the growth of beneficial microbes in the intestines. Choose unpasteurized foods as pasteurization kills beneficial bacteria (probiotics). Although there is no scientifically based dietary guideline for unpasteurized foods, researchers recommend including them in your diet.Fermented foods include the following foods:
5 Supplement your diet with unpasteurized fermented foods. Fermented foods promote the growth of beneficial microbes in the intestines. Choose unpasteurized foods as pasteurization kills beneficial bacteria (probiotics). Although there is no scientifically based dietary guideline for unpasteurized foods, researchers recommend including them in your diet.Fermented foods include the following foods: - Tempeh: fermented soybeans
- Kimchi: fermented Chinese cabbage
- Miso: fermented barley paste
- Sauerkraut: Fermented Cabbage
- Yoghurt: fermented milk with active bacterial cultures
- Kefir: fermented milk
- Kombucha: black or green fermented tea with added fruits and spices
Part 3 of 4: How to Follow a Low FODMAP Diet
 1 Change your diet. Eat a diet low in FODMAPs. The English acronym FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides and polyols. These substances are thought to worsen the symptoms of IBS. Avoid foods containing them or limit them to 1-3 servings per day. A low-fat, complex carbohydrate diet is generally recommended. For example, eat whole grains, lactose-free dairy products, gluten-free foods, fish, chicken and other meats, certain fruits and vegetables (bok choy kale, carrots, bananas, cucumbers, grapes, tomatoes).
1 Change your diet. Eat a diet low in FODMAPs. The English acronym FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides and polyols. These substances are thought to worsen the symptoms of IBS. Avoid foods containing them or limit them to 1-3 servings per day. A low-fat, complex carbohydrate diet is generally recommended. For example, eat whole grains, lactose-free dairy products, gluten-free foods, fish, chicken and other meats, certain fruits and vegetables (bok choy kale, carrots, bananas, cucumbers, grapes, tomatoes). - Eat a low FODMAP diet for at least 4-6 weeks. You may feel immediate relief of abdominal pain, or it will happen over time.
- Talk to your doctor about what you can and cannot eat with this diet.
- It is believed that carbohydrates with a short molecular chain are poorly absorbed by the intestine and are rapidly fermented by intestinal bacteria. This causes increased gassing.
 2 Limit your sugar (fructose) intake. Fructose is poorly absorbed by the intestines, which can cause cramps and diarrhea. Avoid fruits that contain simple sugars such as apples (and applesauce), apricots, blackberries, cherries, cherries, canned fruits, dates, figs, pears, peaches, and watermelons. You should also avoid foods that contain high fructose corn syrup, such as pastries and sugary drinks.
2 Limit your sugar (fructose) intake. Fructose is poorly absorbed by the intestines, which can cause cramps and diarrhea. Avoid fruits that contain simple sugars such as apples (and applesauce), apricots, blackberries, cherries, cherries, canned fruits, dates, figs, pears, peaches, and watermelons. You should also avoid foods that contain high fructose corn syrup, such as pastries and sugary drinks. - Don't forget to eliminate artificial sweeteners from your diet: xylitol, sorbitol, maltitol, and mannitol (these contain polyols that irritate the digestive system).
- You should also avoid vegetables, which can negatively affect digestion. These are artichoke, asparagus, broccoli, beets, Brussels sprouts, cabbage and cauliflower, garlic, fennel, leeks, mushrooms, okra, onions, peas.
 3 Eat less dairy products. Milk contains lactose, a carbohydrate that, when broken down, produces sugar. Lactose can irritate the sensitive digestive system. If you suspect that you are hypersensitive to lactose, you may actually be lactose intolerant, which also causes digestive problems, including IBS. Try limiting your intake of milk, ice cream, most yogurt, sour cream, and cheese.
3 Eat less dairy products. Milk contains lactose, a carbohydrate that, when broken down, produces sugar. Lactose can irritate the sensitive digestive system. If you suspect that you are hypersensitive to lactose, you may actually be lactose intolerant, which also causes digestive problems, including IBS. Try limiting your intake of milk, ice cream, most yogurt, sour cream, and cheese. - Soy-based yoghurts can be consumed as they are lactose-free. However, soybeans should be avoided at the same time.
 4 Pay attention to the proportion of grains and legumes in your diet. Some cereals contain fructans (polymers of fructose molecules) that can irritate the digestive system. Try to limit your intake of grains that contain gluten - these are wheat, spelled, rye, barley. You should also reduce the proportion of legumes in the diet, as they contain galactans, which can also irritate the digestive system. Galactans and fructans can cause symptoms of IBS such as gas and bloating. Try not to eat the following legumes:
4 Pay attention to the proportion of grains and legumes in your diet. Some cereals contain fructans (polymers of fructose molecules) that can irritate the digestive system. Try to limit your intake of grains that contain gluten - these are wheat, spelled, rye, barley. You should also reduce the proportion of legumes in the diet, as they contain galactans, which can also irritate the digestive system. Galactans and fructans can cause symptoms of IBS such as gas and bloating. Try not to eat the following legumes: - Beans
- Chickpeas (chickpeas)
- Lentils
- Red beans
- Bean stews
- Soya beans
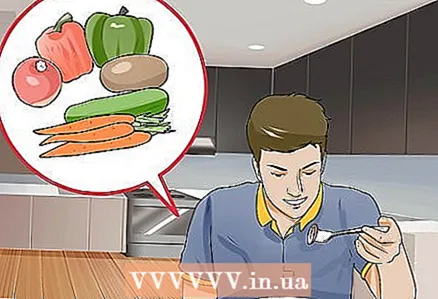
 5 Eat fruits and vegetables. A diet low in FODMAPs allows you to consume a variety of fruits and vegetables.They contain few carbohydrates, so the body does not have to make special efforts to break them down. From fruits, you can eat bananas, berries, melons (but not watermelons), citrus fruits, grapes, kiwi, passion fruit. You can also eat a variety of vegetables that do not irritate the digestive system. Try to include some vegetables in each main course. The following vegetables are suitable:
5 Eat fruits and vegetables. A diet low in FODMAPs allows you to consume a variety of fruits and vegetables.They contain few carbohydrates, so the body does not have to make special efforts to break them down. From fruits, you can eat bananas, berries, melons (but not watermelons), citrus fruits, grapes, kiwi, passion fruit. You can also eat a variety of vegetables that do not irritate the digestive system. Try to include some vegetables in each main course. The following vegetables are suitable: - Bell pepper
- Cucumbers
- Eggplant
- Green beans
- Chives and green onions
- Olives
- Pumpkin
- Tomatoes
- Root and tuberous vegetables: carrots, parsnips, potatoes, radishes, sweet potatoes, turnips, yams, ginger
- Green vegetables: cabbage, lettuce, spinach, Chinese cabbage
- Water chestnut (sweet marsh)
- Zucchini
 6 Include meat and grains in your diet. Get the proteins you need from a variety of sources such as meat, fish, eggs, nuts, and seeds (excluding pistachios). You shouldn't think that you shouldn't eat almost anything. Just make sure that meats and grains do not contain added sugar or wheat, as these ingredients can irritate the digestive system. Choose meat from animals that have not been fed grains and high fructose corn syrup (these foods are high in FODMAPs). The following grains can be consumed:
6 Include meat and grains in your diet. Get the proteins you need from a variety of sources such as meat, fish, eggs, nuts, and seeds (excluding pistachios). You shouldn't think that you shouldn't eat almost anything. Just make sure that meats and grains do not contain added sugar or wheat, as these ingredients can irritate the digestive system. Choose meat from animals that have not been fed grains and high fructose corn syrup (these foods are high in FODMAPs). The following grains can be consumed: - Corn
- Oats
- Rice
- Quinoa
- Sorghum
- Tapioca (cassava flour)
Part 4 of 4: Understanding IBS Symptoms and Risk Factors
 1 Take a closer look at the symptoms of IBS. Different people may have different symptoms of IBS, and their intensity may change over time. The most common symptoms of IBS include the following:
1 Take a closer look at the symptoms of IBS. Different people may have different symptoms of IBS, and their intensity may change over time. The most common symptoms of IBS include the following: - Abdominal pain and cramps, which may be better after a bowel movement
- Bloating and gas
- Constipation (may alternate with diarrhea)
- Diarrhea (may alternate with constipation)
- Strong urge to defecate
- Feeling like you need to have a bowel movement even though you've just done so
- Mucus in stool
 2 Consider risk factors. IBS is a "functional" digestive disorder. This means that the functioning of the digestive system changes for unknown reasons. However, these changes do not lead to any damage to the digestive system. Usually, in parallel with IBS, the following diseases and disorders are observed:
2 Consider risk factors. IBS is a "functional" digestive disorder. This means that the functioning of the digestive system changes for unknown reasons. However, these changes do not lead to any damage to the digestive system. Usually, in parallel with IBS, the following diseases and disorders are observed: - Impaired transmission of nerve signals between the brain and the colon
- Problems with peristalsis (pushing food through the digestive tract)
- Depression, anxiety, or panic disorder
- Digestive system infection
- Overgrowth of bacteria (such as bacterial overgrowth in the small intestine)
- Changes in hormone levels
- Increased food sensitivity
 3 Consult your doctor. Since there is no test or test to diagnose IBS unequivocally, your doctor will do a general examination. Depending on the specific situation, the doctor may order a blood test, stool test, or some kind of imaging study. These tests and tests will help rule out other possible illnesses.
3 Consult your doctor. Since there is no test or test to diagnose IBS unequivocally, your doctor will do a general examination. Depending on the specific situation, the doctor may order a blood test, stool test, or some kind of imaging study. These tests and tests will help rule out other possible illnesses. - If your doctor thinks you have IBS, they may recommend that you change your diet accordingly. Your doctor may prescribe medications (such as muscle relaxants, antidepressants, filler laxatives, or diarrhea medications) to help relieve symptoms.
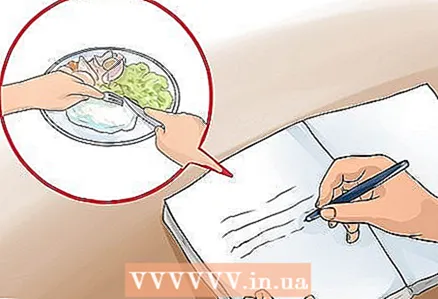 4 Keep a food diary. Write down everything you ate and mark the foods that aggravate the symptoms. Try to avoid this food in the future. For most people with IBS, digestion is impaired by eating the following foods:
4 Keep a food diary. Write down everything you ate and mark the foods that aggravate the symptoms. Try to avoid this food in the future. For most people with IBS, digestion is impaired by eating the following foods: - Fatty food
- Products with artificial sugar substitutes
- Foods that cause gas or bloating (such as cabbage, some legumes)
- Some dairy products
- Alcohol
- Caffeine
Tips
- If you are looking for a prebiotic dietary supplement that contains insulin and fructose oligosaccharides, it should also contain galactooligosaccharides.
- The low FODMAP diet was developed for people with IBS at Monash University in Australia.
- Talk to your doctor about taking nutritional supplements. Always follow the recommended dosage.
Warnings
- Increase your fiber intake gradually. This will help your body get used to the changes in your diet. Increasing fiber too quickly can worsen IBS symptoms.