Author:
Laura McKinney
Date Of Creation:
6 August 2021
Update Date:
22 June 2024

Content
Varicose veins are dilated blood vessels that mainly occur in the legs and affect about half of the adult US population. The disease occurs because pressure in the veins weakens and over time damages the tiny valves and walls of the blood vessels. Usually varicose and spider veins (also known as varicose veins) only make the legs unsightly, but sometimes they also cause a lot of pain when walking and standing, with severe cases causing skin ulcers. Although there is no sure way to prevent varicose veins, there are steps you can take to reduce this risk.
Steps
Method 1 of 3: Take basic precautions
Identify your risk factors. Some people seem to experience varicose veins more easily than others. If you are aware of the risk factors you can choose a healthy lifestyle to prevent this disease. However, if there are multiple risk factors, you should consult your doctor about how to control them.
- Age. Age is a key factor in whether you are likely to have varicose veins or not. The aging process causes the veins to lose elasticity, the valves in them no longer work as efficiently as before. This condition facilitates the development of varicose veins.
- Sex. Women are more prone to varicose veins than men, perhaps because they often experience hormonal changes, such as during menopause or during pregnancy.
- Genetic. If a member of your immediate family has varicose veins, you are at higher risk of developing the disease. Also, if you are born with a weak venous valve, there is a higher risk.
- Fat. Being overweight puts a lot of pressure on your veins and can develop varicose veins.
- Sedentary. You are at higher risk of varicose veins if you regularly stand or sit for long periods of time. When you stay standing or sitting for too long, your veins have more pressure to pump blood back to your heart.
- Foot injury. If you have had a previous leg injury, such as a blood clot, you are at a higher risk of developing varicose veins.

Maintain a healthy weight. Excess weight puts a lot of pressure on your legs and circulatory system, so if you are obese, you should lose weight to reduce your risk of varicose veins.
Build healthy eating habits. Avoid foods that are high in calories and low in nutrients. Eat a high-fiber diet. Several studies have demonstrated that a low-fiber diet is associated with varicose veins. Eating plenty of fiber also helps lower cholesterol and lower blood pressure.
- Avoid adding salt if possible. Reducing the amount of salt consumed has the effect of reducing swelling in the dilated veins, while also reducing the body's water retention.

Exercise regularly. Walking or jogging can improve blood circulation in the legs, which helps to fight the risk of varicose veins or prevent further disease. Average blood pressure will drop and the health of the whole circulatory system improves if you exercise regularly.- Jogging also prevents varicose veins from manifesting on the skin's surface and improves blood circulation in the legs.
- Give up smoking. Smoking contributes to many health problems. Many studies show that high blood pressure caused by smoking is also the cause of varicose veins. Smoking is also linked to "venous insufficiency", a condition in which blood does not circulate normally, leading to a buildup in the legs.

Avoid taking birth control pills high in estrogen. Long-term use of birth control pills containing high levels of estrogen and progesterone may increase the risk of varicose veins. Hormone replacement therapy works just as well. You should consult with your doctor about which option is best for you.- Long-term use of estrogen and progesterone can weaken the venous valve and alter blood circulation in the legs.
- Contraceptive methods that use less estrogen can hardly lead to varicose veins or blood clots.
Stay out of the sun. For people with light skin, too much sun exposure is likely to cause spider veins. Sun exposure also creates the same risks as skin cancer.
- The Centers for Disease Control and Prevention recommends that everyone wear sunglasses at all times when outdoors. Especially you should avoid the sun at noon when the sun is at its highest.
Method 2 of 3: Take care of your feet
Avoid standing for too long. Standing still for a long time increases the pressure in the veins in your legs and feet, and over time this pressure weakens the blood vessel walls. Varicose veins get worse if you regularly stand for a long time, even increasing the number of varicose veins.
- Since some jobs require a long standing, you must minimize your damage by frequently changing positions when the opportunity arises. At least every 30 minutes you should get up and walk back and forth.
Sit properly. Sit up straight and don't cross your legs. Correct sitting posture enhances blood circulation, on the contrary, if you cross your legs, blood will limit circulation in and out of your legs.
- Avoid sitting at work for too long without taking breaks. Every half hour you should get up and stretch your arms or legs or walk around.
Raise your feet if you can. Relaxing and “lifting feet” help you reduce your risk of varicose veins, so try to lift your legs 15 minutes higher than your heart each time, working 3-4 times a day. This exercise improves blood circulation and reduces pressure in the legs.
- If possible, you should raise your legs when sitting or sleeping.
- Other options are to use an inverted table or raise the foot of the bed so that the foot is slightly higher than the head while sleeping. Check with your doctor before using any of these methods.
Redesigned clothing. Increase blood circulation to your lower body by avoiding tight clothing. Especially not to wear tight clothing around the waist, legs and groin area. Tight clothing worsens varicose veins and increases the risk of new varicose veins.
- Wear low-heeled shoes instead of high heels. Low sole shoes help tighten calves, so blood easily circulates through the veins. In addition, the shoe size must also fit the foot to ensure the foot is not locked.
Wear pressed socks. If varicose veins are progressing, you should try to wear pressure socks as often as possible. Compression socks are available at medical equipment stores or drugstores, and there are a variety of different types to choose from. Consult your physician before buying or wearing pressure socks.
- Use a measuring tape to get the correct size when buying socks. The right pressure sock must create enough pressure, but not too much.
- If you are going away, consult your doctor about wearing pressure socks, as this can reduce the pressure in your legs and will prevent and limit varicose veins from getting worse.
Method 3 of 3: Find medical treatment
Identify the symptoms of varicose veins. Usually varicose veins do not cause serious health problems. However, the disease causes discomfort, pain and unsightly feet. Even if the disease poses no danger, you may want to find a way to manage the condition. The common symptoms of varicose veins are:
- Pain and soreness in the legs
- Throbbing pain or cramping
- Feeling heavy or swollen in the leg
- Skin itchy, uncomfortable, or becomes darker
- Legs feel restless, restless
Know when to see a doctor. While most varicose veins pose no health threat, there are sometimes problems that you should intervene with. If you have varicose veins and experience any of the following symptoms, you should seek medical attention:
- Sudden swelling of the leg
- Redness or warmth around veins
- Change in skin thickness or color
- Bleeding around or at a varicose vein site
- A palpable lump appears in the leg
- Open sores
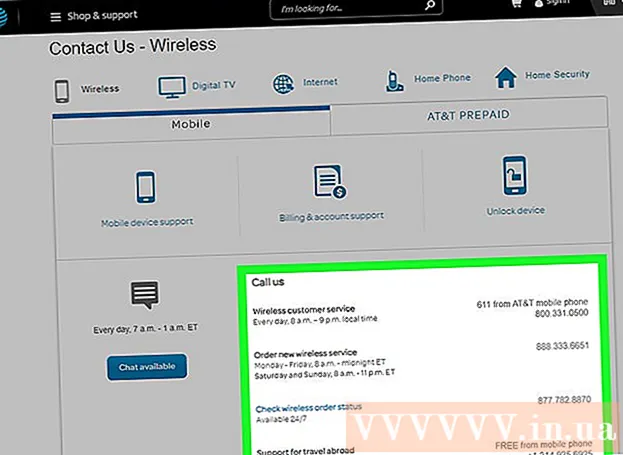
Explore other treatment options. After making some adjustments to your daily routine and your condition does not improve, consider treatment options. Consult your doctor about appropriate options.
- Sclerotherapy. This is the most common treatment for varicose veins. They will inject chemicals into a dilated vein, causing it to swell and close. After a few weeks the vein turns into scar tissue and fades. This procedure can be done in the clinic.
- Laser surgery. This technique is less common because it doesn't work for all skin types and skin tones. Laser surgery is also ineffective for veins larger than 3mm.
- Intravenous intervention technique. Usually applied to severely dilated or deepened veins, which are performed immediately in the clinic and require local anesthesia.
- Surgery. Surgery is usually the only solution to very large or very dilated veins. Consult with your doctor to consider if this is the right solution for you.
Advice
- Although varicose veins are usually not a serious health problem, they are sometimes a sign of another more dangerous condition. If you find that varicose veins are progressing, you should have a physical exam and consult your doctor.
- Varicose veins are more common in women, but more men do. The greater the age, the higher the risk, but the disease can develop at any age, and genetics is a contributing factor.
- Most insurance plans in the US will accept payment for varicose veins, sometimes including spider veins. For other countries you should check with your insurance provider.
- The padlock sock and ankle loops are easy to put on the leg so it will be more suitable for some people.
- Some people think that squeezing with apple cider vinegar can reduce discomfort caused by varicose veins. However, it is likely that the elevation of the legs, the massage and the compressing are the cause of the symptom relief, not the apple cider vinegar. So far, there are no studies proving that apple cider vinegar can treat varicose veins.
- Contrary to popular belief, applying almond oil does not have the effect of improving blood circulation and is not a scientifically recognized treatment, however. eat Almonds can improve blood pressure and blood circulation.
Warning
- See your doctor right away if you have varicose veins and develop chest pain, difficulty breathing or breathing problems. This is a sign that the blood clot is moving to the lungs and heart.
- Beware of expensive and unusual therapies. Even though those "therapies" are not harmful, they are also ineffective. Likewise, you should be wary of supplements that are advertised as curing varicose veins. Some types can actually prevent or cure disease, but there is very little scientific research to prove that. Many dietary supplement companies make claims that are not proven to be valid, so you should consult your doctor before using it. The doctors may not be able to confirm and deny the claims of herb experts, but they know the potentially harmful side effects of some herbs.
- You should not try to "break" the varicose veins with any mechanical methods such as massage or vibration, as this will cause capillary embolism and lead to heart attack. The embolizer can also become trapped in the brain and cause a stroke, or trapped in the lung leading to a lung infarction. These are potentially fatal medical problems.
- See your doctor right away if varicose veins begin to bleed, if you experience sudden pain or swelling in your legs or feet, or if a lump develops around or in a varicose vein.