Author:
John Stephens
Date Of Creation:
22 January 2021
Update Date:
1 July 2024

Content
Dengue is a viral infection transmitted by two species of mosquitoes, mosquito(Aedes aegypti) and Asian tiger mosquito(Aedes albopictus). The number of people infected with dengue each year has reached global reach. A recent World Health Organization estimate shows that there are 400 million new cases of dengue each year. An estimated 500,000 people, most of them children, develop more severe forms of dengue fever and require hospitalization. Sadly, of these, about 12,500 people died. The primary focus of treatment is the use of supportive measures and attention to identifying more serious conditions of the disease for timely care.
Steps
Part 1 of 5: Recognize the symptoms of dengue fever

Expect an incubation period of 4 to 7 days. When a person is bitten by a mosquito that carries the dengue virus, the average time for symptoms to start appearing is 4 to 7 days.- Although the average incubation period is 4 to 7 days, early symptoms can appear within 3 days or as late as 2 weeks after a mosquito bite.
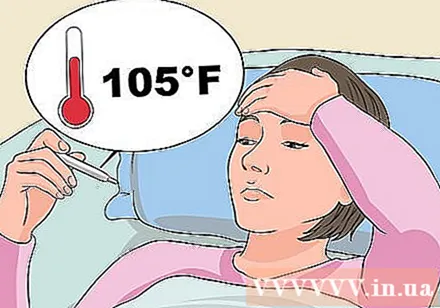
Measure body temperature. High fever is the first symptom to appear.- Dengue fever usually has a high temperature, between 38.9 ° C and 40.6 ° C.
- The high fever lasts 2 to 7 days, then returns to normal or even slightly lower than usual, but the fever may return. The fever may return and last for many more days.

Watch for flu-like symptoms. The symptoms that appear first after a fever are usually nonspecific, and manifest as a cold.- The most common symptoms following a fever include severe headaches in your frontal area, pain behind your eyes, muscle pain and severe joint pain, nausea and vomiting, fatigue, and rash.
- Dengue was once known as a "bone fracture fever" due to the terrible pain that patients sometimes feel in the muscles and joints.
Watch for bleeding abnormal symptoms. Other common symptoms caused by the virus can cause hemodynamic changes, or changes in blood circulation in the body.
- Some changes in blood circulation in dengue include nosebleeds, bleeding from the roots of the teeth, and bruises on the body.
- Additional symptoms associated with changes in blood circulation may be evident in red areas in the eyes, pain and swelling in the throat.
Watch for a rash. The rash usually appears within 3 to 4 days after the fever, can go away in a day or two, but can come back afterward.
- The first flare-up usually starts on the face and can be in the form of reddened areas or red spots. The rash is not itchy.
- A second episode of rash begins in the torso, then spreads to the face, arms, and legs. This form can last from two to three days.
- In some cases, the rash is small spots called petechiae, which can appear anywhere on the body once the fever has subsided. Other types of rash that occur sometimes are an itchy rash on the palms of the hands and soles of the feet.
Part 2 of 5: Diagnosis of dengue fever
See a doctor. When you experience symptoms consistent with dengue, you should see your doctor as soon as possible to be diagnosed.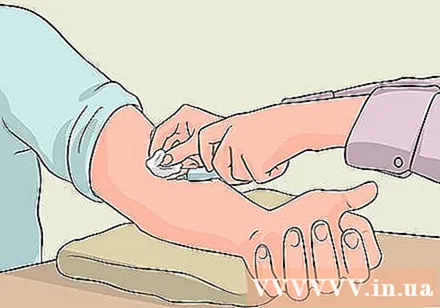
- Blood tests can help your doctor determine if you have been exposed to dengue fever.
- The doctor will analyze the blood to confirm the presence of dengue antibodies. Full results from blood tests take weeks to come.
- Your doctor may check for changes in platelet count to confirm the diagnosis. People infected with dengue have a lower platelet count than normal.
- Another additional test is the tourniquet test, which can give your doctor information about the condition of the capillaries. This test is not decisive, but can be used to supplement the diagnosis.
- Research is currently underway to develop new tests for the diagnosis of dengue fever, including rapid local tests. Rapid spot tests can be done in the clinic or during hospital stay and help quickly confirm infection.
- The signs and symptoms are often enough for your doctor to determine you have a dengue infection, provide supportive treatment, and monitor your progress.
Consider the geographic limit of dengue fever. Although dengue is a global problem, there are areas that are frequently endemic and others that have never been reported.
- You are more likely to be bitten by a dengue carrier if you live in tropical regions such as Puerto Rico, Latin America, Mexico, Honduras, Southeast Asia and the Pacific Islands.
- The World Health Organization confirms the places where dengue fever is also reported are in Africa, South America, Australia, the countries of the eastern Mediterranean and the western Pacific islands.
- Recently recorded cases occurred in Europe, France, Croatia, Portugal's Madeira Islands, China, Singapore, Costa Rica and Japan.
Consider areas of high risk in America. There were several cases of dengue recorded in Florida in 2013.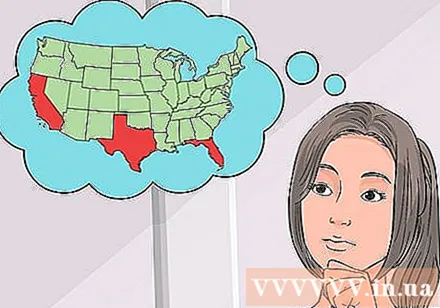
- A recent report in July 2015 found that there were no cases recorded in Florida in 2015.
- Ten counties in California have reported cases of dengue in the past two years.
- Until July 2015, new cases were recorded in Texas, along the border with Mexico.
- So far, cases occurring in the US have been limited to Florida, California, and today Texas. Dengue fever has not been reported in any other region of the US.
Think about your recent trips. If you think you have dengue fever, think about the areas you have been to in the past two weeks, or where you live.
- If you live in the US, your symptoms are probably not dengue unless you are in California, Texas, or Florida, have been to those states for the past few weeks, or have been to one of the above areas. There are mosquitoes that carry dengue fever in the world.
Know which mosquitoes carry disease. Mosquitoes that carry dengue have distinctive features.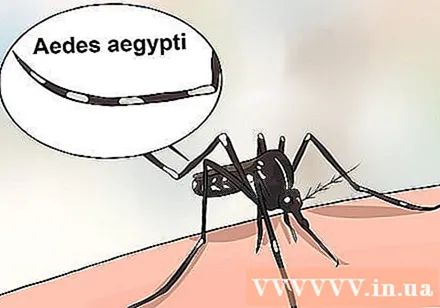
- Mosquito Small and black, with white stripes on the legs. They also have silver or white patterns on their bodies that resemble an instrument called a lute.
- You may also remember that you were bitten by the mosquito described above. If you remember the form of the mosquito that bitten you, that information can be useful for diagnosis.
Part 3 of 5: Treatment of dengue fever
Seek medical attention as soon as possible. Although there is no specific cure for dengue fever, medical attention is needed given the risk of developing bleeding problems from the disease.
- Most patients will feel better in about 2 weeks with general care.
Follow the treatment regimen. The usual regimen of dengue fever is the practice of healing the body.
- Lie down a lot in bed.
- Drink plenty of fluids.
- Take medication to control your condition.
- Acetaminophen is recommended for reducing fever and reducing the discomfort of dengue fever.
Avoid aspirin. Due to the risk of bleeding, aspirin is not used to relieve pain and fever in dengue fever.
- Ask your doctor about over-the-counter anti-inflammatory drugs. Medicines such as ibuprofen and naproxe can reduce fever and unpleasant symptoms.
- In some cases, ibuprofen or naproxen may not be appropriate if you are taking similar medicines, or you are prone to gastrointestinal bleeding.
- Follow the directions on the label you are taking. Do not exceed the recommended dosage.
- Check with your doctor if you are taking pain relievers or blood thinners before taking over-the-counter medications.
Wait weeks to recover. Most patients recover from dengue within two weeks.
- Many patients, especially adults, continue to feel tired and somewhat depressed for many weeks to months after being infected with dengue.
Find an ambulance. If symptoms persist or appear signs of bleeding, contact your doctor immediately or call an ambulance. Some of the alarming symptoms that indicate your body is having trouble keeping the vascular system working include:
- Persistent nausea and vomiting.
- Vomiting of blood or substance like coffee powder.
- There is blood in the urine.
- Stomachache.
- Shortness of breath.
- Nosebleeds or root bleeding.
- Easy to bruise.
- You are more likely to be hospitalized after an emergency. While in hospital you will be treated with supportive care measures that can save your life.
- Some care measures may include fluid supply and electrolyte replacement, treatment or prevention of shock.
Part 4 of 5: Keep track of possible complications
Continue treatment regimen. Stay in contact with your doctor and report any changes in treatment if any, or if symptoms recur or worsen.
- Your doctor will know how to intervene if your condition worsens dengue fever or dengue shock syndrome.
Watch for persistent symptoms closely. If symptoms persist for more than seven days, including problems such as persistent vomiting, bloody vomiting, severe abdominal pain, difficulty breathing, bruising on the skin, constant nosebleeds and bleeding root, you should look for immediate emergency.
- Your illness can progress to dengue, a very serious and life-threatening condition.
- If the above symptoms progress, you are in the 24 -48 hour window period, when the capillaries, the tiny blood vessels in the body, become more permeable or leak.
- Leaking capillaries cause fluid to seep through blood vessels, accumulating in the chest and abdominal cavities, causing conditions called ascites and pleural effusions.
- You may experience circulatory disorders, leading to shock. If not treated in time, the patient can die.
Seek emergency help. If you have any of the signs of dengue fever or hemorrhagic shock syndrome, you'll need immediate hospitalization for care. This is a life-threatening situation.
- Call an ambulance on 115 or get medical help as quickly as possible. This is an emergency.
- Dengue shock syndrome can be identified by early symptoms including loss of appetite, non-stop fever, persistent vomiting and symptoms related to persistent dengue. The greatest risk of shock is on the third or seventh day of the illness.
- If left untreated, internal bleeding will continue. Symptoms of hemorrhage include bleeding under the skin, persistent bruising or reddish purple rash, worsening symptoms, unusual bleeding, cold and damp hands and feet, sweating.
- The above symptoms indicate that the patient is or is about to fall into a state of shock.
- Hemorrhagic shock syndrome can be fatal. If passed, the patient may develop encephalopathy, loss of brain function, liver damage or seizures.
- Treatment for hemorrhagic shock syndrome includes limiting blood loss, rehydrating fluid, restoring normal blood pressure, providing oxygen, and possibly getting a blood transfusion to restore platelets and bring healthy blood. to important organs in the body.
Part 5 of 5: Prevent dengue fever
Avoid mosquitoes. Mosquitoes carry the dengue germs that bite during the daytime, usually early in the morning or late afternoon.
- Stay indoors during these times, turn on the air conditioner, and close the windows and doors.
- Walk outside during a time when mosquitoes are inactive.
Cover skin. Wear long clothes that cover the whole body. Even if it's hot, try to wear long pants, a long-sleeved shirt, wear socks and shoes, and even wear work gloves when you need to be outdoors during mosquitoes.
- Sleep mosquito nets.
Use mosquito repellent. DEET-containing mosquito repellent products have been found to be effective.
- Other insect repellants that may be helpful include those that contain picaridine, lemon or eucalyptus essential oil, or IR3535.
Check around the house. Mosquitoes that carry dengue diseases often live near home.
- They like to breed in standing water in artificial containers such as drums, flower pots, pet water bowls, or old tires.
- Eliminate any unnecessary condensation.
- Check for potential standing water sources. Clogged drains and gutters, wells, manholes, and septic tanks can all be pools of water. Clean these areas up or fix them so they don't stand still.
- Remove containers with standing water outside around or near the home. Wash the vase, bird bath, fountains and pet water dish at least once a week to get rid of the larvae.
- Maintain pools and release mosquito-eating fish into small tanks.
- Make sure windows and doors are screened, snug and tightly closed.