Author:
Lewis Jackson
Date Of Creation:
11 May 2021
Update Date:
1 July 2024
Content
Cervical cancer is cancer of the part of the uterus. This disease can occur in women of any age, but usually focuses on women between the ages of 20 and 50. Most women get cancer because they do not go to the gynecological examination regularly and undergo screening. filtering for cervical cancer. Fortunately, cervical cancer can be completely cured if found and treated early. The main symptoms to watch out for are vaginal bleeding and pain.Some symptoms appear only when abnormal cells develop in the surrounding tissue. So you need to see your doctor as soon as you notice any unusual change. Regular screening with cervical smear (PAP smears) and HPV testing can help detect precancerous conditions before it develops into cervical cancer.
Steps
Part 1 of 2: Recognize the symptoms
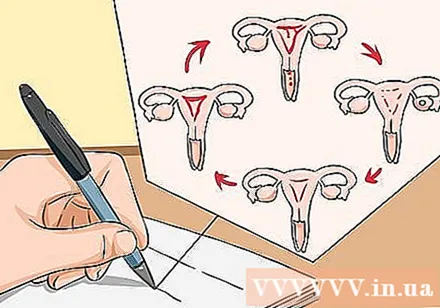
Monitor your menstrual cycle. If you are in perimenopause or near menopause, use a calendar to keep track of when your next menstrual cycle occurs and how long it will last. When you're at menopause, it's important to have a clear understanding of when your last menstrual cycle occurs. The most common symptom of cervical cancer is abnormal vaginal bleeding. You need to know what is normal for you and for any other woman.- The menstrual cycle is still going on steadily while you are in the premenopause. Every woman's body is not the same, however the normal cycle is 28 days late or earlier than 7 days.
- Near menopause, your menstrual cycle will be irregular. This stage usually begins in women between the ages of 40 and 50. This transition occurs when the ovaries begin to produce less estrogen and can last for months to 10 years before reaching menopause. complete experience.
- When it comes to menopause, the menstrual cycle ends. Hormonal levels have reached the point of ceasing to ovulate. Then you will no longer be able to get pregnant.
- If you have had your cervix removed, you will not have a red light time. As the uterus has been removed, the endometrium no longer sloughs off and causes a period. If you still have your ovaries, you're not in menopause yet.
Note that small spots appear during the menstrual cycle. When you notice a small spot, your menstrual production is less and the blood color is different from normal.- During the perimenopause, sometimes the menstrual cycle is irregular and small spots may appear. Factors like illness, stress or heavy exercise also affect the cycle. See your doctor if you notice an irregular menstrual cycle lasting several months.
- Small spot is a normal phenomenon of near menopause. You should be vigilant and watch for other cervical cancer symptoms.

Note that the menstrual cycle is longer and longer than usual. During each menstrual cycle, blood production, color, and consistency may vary. If these factors change markedly, you should contact your doctor.
Contact your doctor in case menstruation suddenly occurs not on a regular basis. Remember that it's not normal for vaginal blood to appear when you are menopausal or when your cervix has been removed.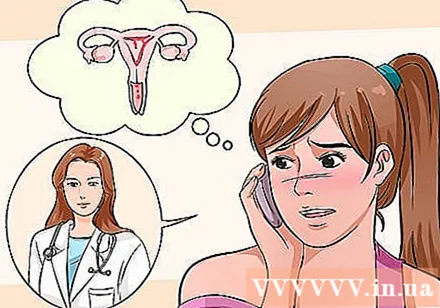
- The process of hysterectomy has not necessarily removed the cervix. When the hysterectomy is complete, the entire uterus and cervix will be removed. A partial cervicectomy is performed in the absence of malignancy. Then the cervix is still in place and you are still at risk for cervical cancer. Ask your gynecologist about hysterectomy surgery.
- If you have not gone through the red light period for 12 consecutive months, you may have entered menopause.
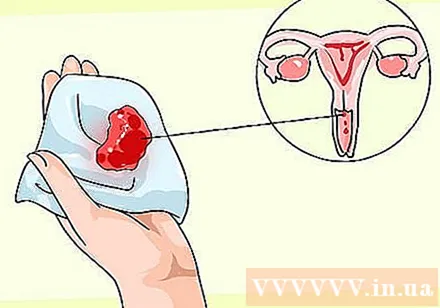
Watch out for vaginal bleeding after normal activity. These activities include intercourse, douching, and even gynecological examination performed by the doctor. Talk to your doctor about the characteristics of blood, small spots with high blood flow.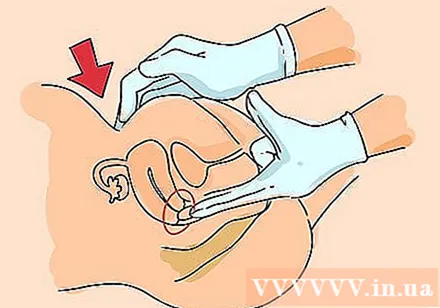
- During the gynecological examination, the doctor inserts a gloved finger into the vagina and presses the lower abdomen with the other hand. The doctor may examine the uterus, including the cervix, and the ovaries for signs of abnormality or illness. This action does not cause excessive bleeding.
Watch for unusual vaginal discharge. The discharge can be bloody and can appear between menstrual cycles as well as have an unpleasant odor.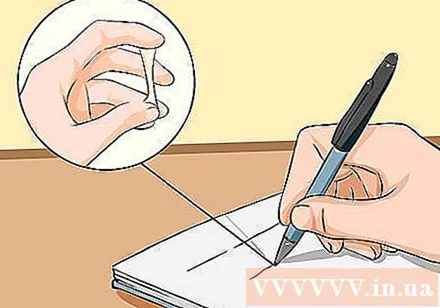
- The cervix secretes mucus with a varying density during the menstrual cycle that can help prevent or encourage pregnancy. There should be no blood between the menstrual periods.
- If menstrual blood builds up in the vagina for 6 to 8 hours, your genital area will smell bad. This is different from a foul smelling discharge.
- Seek medical attention. An unpleasant discharge can be caused by other conditions, such as inflammation that causes pain and bleeding, or from precancer or cancer.
Talk to your doctor about pain after sex or pelvic pain. Pain during sex is normal; 3 out of 4 women experience this condition during sex at some point in time. However, if the pain occurs frequently or worsens, discuss this with a qualified medical professional. Make a distinction between menstrual cramps and pelvic or lower abdominal pain.
- During menopause and perimenopause, the vagina can change due to fluctuations in estrogen levels. The vaginal wall will become thinner, dry, less elastic, and more sensitive to irritation (atrophic vaginitis). Sometimes having sex is painful due to these changes.
- Pain during sex can also occur during skin irritation, or less lubricant secretion.
Part 2 of 2: Seeking medical help
See a doctor as soon as symptoms appear. Delaying the disease can get worse and reduce the chances of an effective treatment.
- Upon admission, the doctor will collect information about your personal and family history as well as your symptoms. In addition, your doctor discussed risk factors such as having multiple sex partners, early sexual activity, sexually transmitted diseases, decreased immunity, and smoking history.
- After knowing your medical history, your doctor will conduct tests to determine your overall health. During the visit, the doctor will perform cervical smear and HPV testing if it has not been done in the past. These are screening tests (for signs of cervical cancer) and have no diagnostic effect (confirm cervical cancer).
- Diagnostic tests are performed only after cervical smear and / or abnormal symptoms associated with cervical cancer. The test involves colposcopy using a vaginal opening reflector to magnify the cervix to help the doctor see the abnormal area on the cervix. If necessary, the doctor will perform a curettage of the endometrium (the inner lining of the cervix) and / or a cone biopsy. The pathologist will use an observational microscope to diagnose precancerous or cancerous changes in cells.
Get regular cervical cancer screening before symptoms appear. There are two types of tests that are done in the clinic for precancerous lesions: cervical smear and HPV.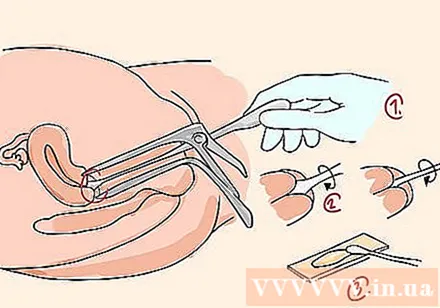
Get regular cervical smear tests. This test identifies precancerous cells at risk of developing cervical cancer if they are not treated early and properly. This test is needed for women between the ages of 21 and 65 and can be done in a doctor's office or hospital.
- During the analysis, the gynecologist inserts a reflector into the vagina to examine the walls of the vagina and cervix, and then collects cells and mucus in the cervix along with and surrounding tissues. These samples will be placed in a slide or bottle containing the liquid and sent to a laboratory for examination under a microscope to determine any abnormality.
- You should get regular cervical smear testing even during sex abstinence and after menopause.
- The cervical smear test can be done in any hospital or clinic, because it is included in the list of services in compulsory health insurance. If you don't have insurance, you can get the test done for free or at a low cost at a community hospital.
Get tested for HPV. This test is done to detect the human papillomavirus, which causes precancerous changes in the cells of the cervix.Most cervical cancers are caused by HPV infection. This virus is passed from person to person during sex. Cells collected during the cervical smear can be analyzed for HPV.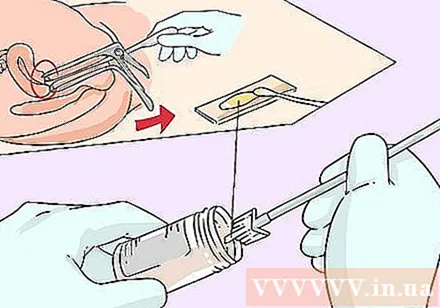
- The cervix has a cylindrical shape below the uterus. The uterus is the site where the doctor checks with a reflex mirror. The endometrium is the tube that passes through the cervix and into the endometrium. Cervical cancer can occur in the transition zone between the endometrium and the uterus. This is the site for sampling cervical cells and mucus.
- Women over 30 years of age should have cervical smear and HPV testing every 5 years.
Talk to your doctor about how often to have cervical smear and HPV tests. The timing of a screening or follow-up test depends on your age, number of sexual partners, as well as history and results of previous cervical smear and HPV smear tests.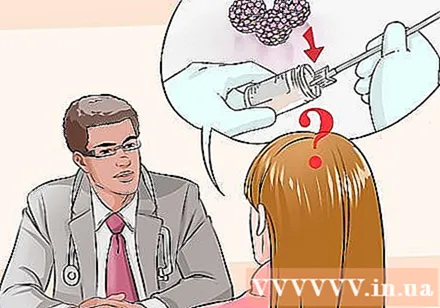
- Women between the ages of 21 and 29 need to have a Pap smear every 3 years. Women aged 30 to 63 years need a smear test every 3 years or in combination with an HPV test every 5 years.
- If you have a poor immune system, are HIV positive, or have an abnormal cervical smear, talk with your doctor about whether to have a smear test more often are not.
- Cervical cancer is one of the most common cancers in women. However, the incidence of this cancer is often lower in developed countries than in other countries due to widespread and frequent use of cervical smear and HPV testing.
- Early diagnosis and treatment. Cervical cells with significant changes carry a huge cancer risk. The transition from normal to anomalous to invasive cells can occur within 10 years, but it can happen sooner.