Author:
Louise Ward
Date Of Creation:
6 February 2021
Update Date:
1 July 2024

Content
Hemorrhoids are enlarged and inflamed veins in the lower rectum and anus. This is a common disease in which about 50% of adults face hemorrhoids at least once before the age of 50. Hemorrhoids are caused by increased pressure in the veins in the lower rectum and anus, cause veins to swell. Visible symptoms include: painless bleeding during bowel movements, rectal / anal pain, anal itching and / or soft lumps near the anus. There are many home remedies and medical treatments for hemorrhoids and hemorrhoids pain.
Steps
Method 1 of 3: Treat hemorrhoids at home
Determine the type of hemorrhoids. Hemorrhoids can be internal or external hemorrhoids. Pain symptoms are usually caused by external hemorrhoids. However, it's best to see your doctor for an accurate diagnosis.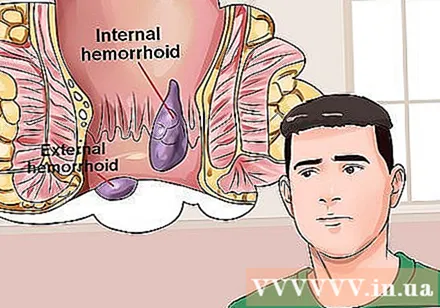
- Internal hemorrhoids develop in the lower rectum, usually not causing pain because the body does not have pain receptors in the rectum. You may not know you have internal hemorrhoids until you see blood in your stool or see the hemorrhoids come out (sticking out of your anus).
- Painful symptoms with hemorrhoids are usually a sign of external hemorrhoids, which develop under the skin around the anus. If a blood clot forms in a hemorrhoid, it is called an "embolism hemorrhoids", the pain is described as very intense and sudden. The patient can see or feel the lump around the anus. The blood clot usually dissolves gradually, leaving excess skin protruding in the anus.
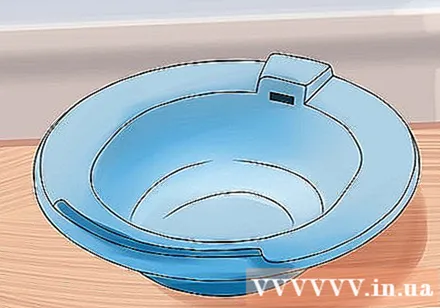
Bathing Sitz. Sitz bath therapy (or sitz bath) can provide immediate relief from the pain and itching associated with hemorrhoids. Soak the anal area in warm water for 10-20 minutes, 2-3 times daily and after defecating. In pharmacies, small plastic containers are often sold to fit the toilet. Or you can fill the tub with warm water so it reaches your hips.- Gently use a towel to dry the anus or use a hair dryer to dry it after a sitz bath.
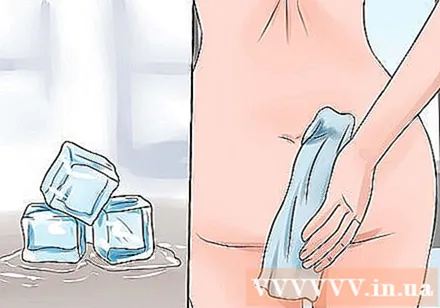
Apply a cold compress to the anus. A cold compress can help reduce swelling and pain from hemorrhoids. You can apply a water-filled and frozen condom or an ice pack wrapped in a soft cloth over the anal area for 5-10 minutes, 3-4 times a day.- Gently dry the anus with a towel or use a hair dryer to dry it after applying the cold compress.
Try over-the-counter topical medications. There are specialized over-the-counter medications available at pharmacies to help relieve the pain and discomfort associated with hemorrhoids. Some products you can buy:- Apply the Tucks cold pad to the affected area from hemorrhoids up to 6 times a day to relieve pain and itching. The cold pad contains witch hazel with natural soothing and anti-inflammatory properties.
- Preparation H cream is a local anesthetic, which helps constrict blood vessels and protect the skin effectively in the treatment of hemorrhoids. Preparation H cream blocks pain signals from nerve endings in the anus, while also helping to shrink swollen, inflamed tissue.
- Over-the-counter creams or suppositories containing the steroid hydrocortisone may help with hemorrhoids. Hydrocortisone is a powerful anti-inflammatory that can help soothe the pain and itchiness of hemorrhoids. Topical steroid medications such as hydrocortisone should be used for no more than 7 days as this can lead to atrophy of the skin of the anus.
- Pramoxine, available in both prescription and over-the-counter medications, is another local anesthetic used to treat hemorrhoids.
Take a pain reliever. Over-the-counter pain relievers such as acetaminophen (Tylenol), ibuprofen (Advil), or aspirin can be used to relieve the discomfort of hemorrhoids.
- Acetaminophen can be taken at a dose of 650-1000 mg every 4-6 hours, not to exceed 4 g for 24 hours.
- Ibuprofen can be taken in 800 mg, up to 4 times daily.
- Aspirin can be taken at a dose of 325-650 mg every 4 hours if needed, not to exceed 4 g in 24 hours.
Take a stool softener. Stool softeners can be helpful if you have constipation due to hemorrhoids. An over-the-counter stool softener like docusate (Colace) can be used to keep your stools soft, relieve constipation, and tighten the anal area. 100-300 mg of docusate can be taken per day for up to 7 days. advertisement
Method 2 of 3: Get medical treatment
See a doctor. Sometimes hemorrhoids get better with home treatment and don't need medical treatment. However, you should consult your doctor if your hemorrhoids symptoms do not improve after a week of home treatment. Your doctor can talk to you about more powerful prescription medications or recommend surgery.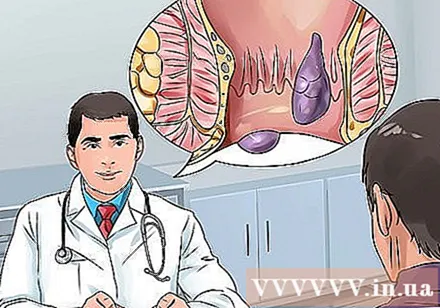
- See a doctor right away if hemorrhoids are painful.
- Your doctor may advise you to make changes in your diet and lifestyle before trying medications or surgery. These changes can include increased fiber and exercise.
Ask your doctor about a stronger prescription anesthetic. If you think that surgery isn't necessary, your doctor may prescribe a stronger anesthetic like lidocaine (Xylocaine) to help ease the pain, itching, and discomfort associated with hemorrhoids.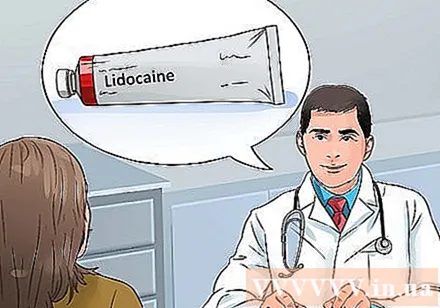
Talk to your doctor about how to use a rubber ring with hemorrhoids. This is the most common procedure for treating hemorrhoids. Your doctor will tie a small elastic ring around the center of the internal hemorrhoids to block circulation to the hemorrhoids. When there is no blood flow, the hemorrhoids shrink and dry within a week.
Talk to your doctor about intravenous fiber injection. Your doctor will inject a chemical solution into the hemorrhoids to scar and shrink the tissue. This method is not effective by tying hemorrhoids with a rubber ring.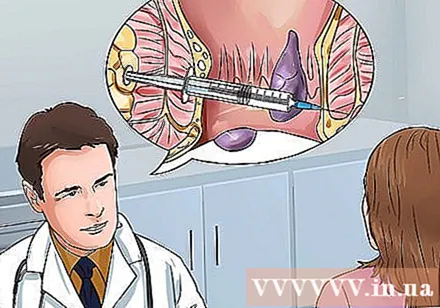
- The method of intravenous fibrosis is not recommended by some doctors because studies show that this method is only effective for a short time and hemorrhoids will recur in most patients.
Research on blood clotting methods. Coagulation technique uses laser beam, infrared light or heat. This procedure stops bleeding in the small hemorrhoids and causes them to shrink. Compared with the method of constricting hemorrhoids with rubber rings, the technique of coagulation has a higher rate of hemorrhoids recurrence.
- This technique is often applied to small hemorrhoids (rubber ring ligation is not applicable) or in combination with rubber area hemorrhoids, providing a success rate of 97%.
- The patient only takes a short time (1-2 weeks) to recover from surgery.
Research the removal of hemorrhoids. This procedure is called hemorrhoidectomy. Internal or external hemorrhoids will be removed surgically. This is the most effective treatment for severe or recurrent hemorrhoids, curing 95% of patients and the rate of complications is low.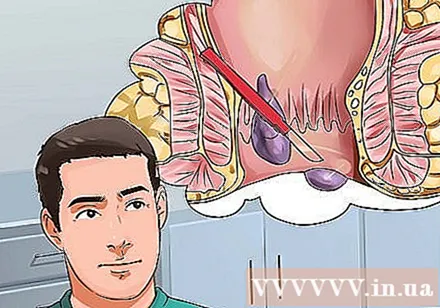
- The removal of hemorrhoids is usually done in cases of internal embolism, internal hemorrhoids combined with external hemorrhoids, or rectal problems requiring surgery. Surgery to remove hemorrhoids will be more painful and recovery time will also be longer.
- Recovery time from hemorrhoidectomy is usually 2-3 weeks with one follow-up visit.
Consider cutting out hemorrhoids with a forceps. In clamp removal, your doctor will use a clamping device to clamp the hemorrhagic or prolapsed hemorrhoid and fix it in its normal position. The procedure of cutting hemorrhoids with forceps prevents the blood flow to hemorrhoids, helping to shrink hemorrhoids.
- Compared with hemorrhoids, forceps cut hemorrhoids with a higher risk of recurrence and prolapse of the rectum (rectum protruding from the anus). However, compared with conventional hemorrhoidectomy, cutting hemorrhoids with forceps significantly reduces the pain after surgery.
Method 3 of 3: Prevent hemorrhoids
Increase fiber in your diet. Increasing fiber consumption can prevent constipation - the main cause of hemorrhoids. Fiber is found in fruits, vegetables and whole grains. Fiber helps to soften stools, reducing anal tension in the first place - the main cause of hemorrhoids.
- The recommended dose of fiber supplements is about 20-35 g per day, depending on age and gender. Women under 51 need 25 grams of fiber daily, while women over 51 need 21 grams per day. Men under 51 need 38 grams of fiber daily, while men over 51 need 30 grams.
- Alternatively, you can get more fiber from over-the-counter fiber sources like psyllium husk (Metamucil, Citrucel).
- Increase fiber in your diet slowly to avoid bloating.
- If increasing fiber intake still doesn't help relieve constipation, incorporate a stool softener like Colace in the short term.
Drink a lot of water. Getting enough water helps prevent constipation. You should drink 6-8 glasses of water, each 8 oz, per day. Water softens stools and helps bowel movements go smoother. This step is especially important for people who are consuming fiber, as not drinking enough water while increasing fiber intake can cause constipation or worsen constipation.
Exercise regularly. Regular exercise helps to increase bowel movements to prevent constipation. In addition, exercise also helps to lose weight, which in turn reduces pressure on the lower rectum and anus to prevent hemorrhoids.
- It is recommended to exercise for 30 minutes, at least 5 times per week. You can split it into several shorter training sessions. For example, exercise for 15 minutes, 2 times a day, or 10 minutes, 2 times a day if you feel that way.
- Do something that you enjoy to increase your motivation. You can walk after a meal, cycle to work, or take aerobic classes a few times a week.
Go to the toilet as soon as you need it. Stopping defecation can worsen constipation and trigger hemorrhoids. You should stay close to the toilet when it's time to defecate so you can go as soon as you feel the need.
- If, after sitting on the toilet for 5 minutes, you are still unable to defecate, get up and come back later. Sitting on the toilet for too long can make hemorrhoids worse.
Avoid sitting for too long. Sitting for long increases the pressure on the lower rectal veins and the anus, contributing to hemorrhoids. If your work involves sitting a lot, get up and walk around even for a few minutes while you have a break. advertisement
Warning
- This article provides information regarding hemorrhoids but is not medical advice. You should always consult your doctor for the best treatment.
- People with anal-rectal bleeding when taking blood thinners (anticoagulants) such as warfarin (Coumadin), clopidogrel (Plavix), enoxaparin (Lovenox), rivaroxaban (Xarelto), dabigatran (Pradaxa) or apixaban (Eliquis) ) need urgent medical evaluation.
- Hemorrhoids do not cause abdominal pain, so the anal-rectal bleeding accompanied by abdominal pain requires immediate medical attention.
- Anorectal bleeding accompanied by dizziness, mild headache or fainting should also be examined urgently. The above symptoms may indicate significant blood loss and require blood transfusion.
- In cases of internal hemorrhoids that cannot be pushed back into the anus, urgent medical attention is required.
- Thrombolytic hemorrhoids cause severe pain that should be examined urgently and require dissolution of a blood clot if indicated.