Author:
Joan Hall
Date Of Creation:
4 July 2021
Update Date:
1 July 2024

Content
- Steps
- Part 1 of 3: Identifying Features
- Part 2 of 3: Making a diagnosis
- Part 3 of 3: Oral Hygiene
- Tips
- Similar articles
The gums are the basis for the teeth. Like trees with roots in the ground, teeth grow out of the gums. Keeping the gums in good shape is very important for the health of not only the oral cavity, but the entire body. In fact, taking care of your gums is just as important as taking care of your teeth. This article explains how to diagnose gum disease based on your symptoms and determine if you need to visit your dentist or dental surgeon.
Steps
Part 1 of 3: Identifying Features
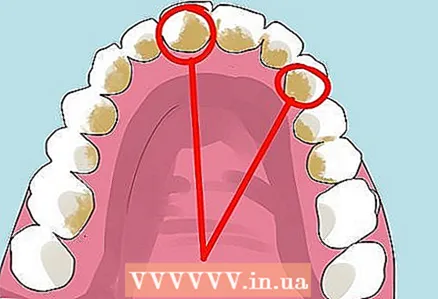 1 Learn about the causes of gum disease. Problems start with a buildup of plaque (a sticky substance) on and around the teeth. Plaque is the environment in which harmful bacteria thrive. These bacteria release acids that not only damage tooth enamel but also affect the gums.
1 Learn about the causes of gum disease. Problems start with a buildup of plaque (a sticky substance) on and around the teeth. Plaque is the environment in which harmful bacteria thrive. These bacteria release acids that not only damage tooth enamel but also affect the gums. - Plaque is a transparent layer, so it is often not visible.
- Flossing regularly helps remove plaque below the gum line.
- Hardened plaque is called tartar and can only be removed by a dentist.
 2 Check out the types of gum disease. Gum disease affects more than just the gums, it can cause damage and even loss of teeth. Gingivitis is an early stage of gum disease, while periodontitis is a more serious condition affecting the jawbone.
2 Check out the types of gum disease. Gum disease affects more than just the gums, it can cause damage and even loss of teeth. Gingivitis is an early stage of gum disease, while periodontitis is a more serious condition affecting the jawbone. - Only a specialist can diagnose gingivitis, since the symptoms of this disease may be mild.
- In case of periodontitis, urgent treatment is necessary, as if delayed, it can lead to the loss of teeth.
 3 See if your gums are bleeding when you brush or floss. You should pay attention to this symptom, since it is the main symptom of periodontitis. The lack of pain with bleeding leads to the fact that many people postpone treatment, which would help to avoid bOmore problems in the future.
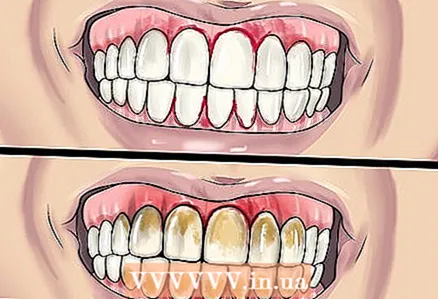
3 See if your gums are bleeding when you brush or floss. You should pay attention to this symptom, since it is the main symptom of periodontitis. The lack of pain with bleeding leads to the fact that many people postpone treatment, which would help to avoid bOmore problems in the future.  4 Examine your gums regularly for abnormal signs. Swollen, loose, red or purple irritated gums indicate illness.
4 Examine your gums regularly for abnormal signs. Swollen, loose, red or purple irritated gums indicate illness. - Healthy gums are pale pink, not dark red or purple.
- If the gums protrude and bulge around the teeth, this may indicate a medical condition.
- Gum disease is also evidenced by the exposure of the roots of the teeth, when the teeth protrude from the gums and appear "longer".
 5 Notice any pain in your teeth, gums, or jaw while eating. The pain is less noticeable in the early stages, but with the development of the disease, as the roots of the teeth become exposed, the sensitivity to temperature changes increases.
5 Notice any pain in your teeth, gums, or jaw while eating. The pain is less noticeable in the early stages, but with the development of the disease, as the roots of the teeth become exposed, the sensitivity to temperature changes increases. - If you feel a change in your bite, it means that your teeth are moving slightly in relation to each other, which may indicate gum disease.
- Pay attention to new spaces between your teeth, which not only affect chewing, but may also indicate gum disease.
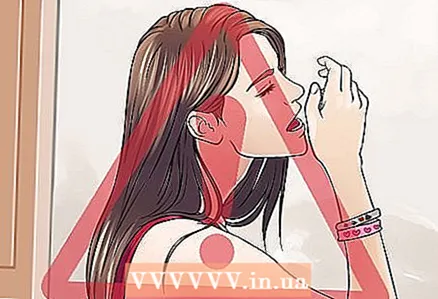 6 Pay attention to your breathing. Halitosis and a persistent bad taste in the mouth can indicate gum disease. If you feel comfortable, ask a friend or relative to sniff your breath; if not, try to assess the bad breath yourself.
6 Pay attention to your breathing. Halitosis and a persistent bad taste in the mouth can indicate gum disease. If you feel comfortable, ask a friend or relative to sniff your breath; if not, try to assess the bad breath yourself.
Part 2 of 3: Making a diagnosis
 1 Make an appointment with your dentist. Only a dentist can tell if you have gingivitis or periodontitis, and the earlier you visit, the more successful the treatment will be.
1 Make an appointment with your dentist. Only a dentist can tell if you have gingivitis or periodontitis, and the earlier you visit, the more successful the treatment will be.  2 Prepare for your doctor's appointment. Your dentist specializes in oral health and will ask you in detail about how you care for your teeth and gums and your lifestyle. Make a list of questions that interest you, do not forget to note the abnormal appearance of the gums and the pain experienced.
2 Prepare for your doctor's appointment. Your dentist specializes in oral health and will ask you in detail about how you care for your teeth and gums and your lifestyle. Make a list of questions that interest you, do not forget to note the abnormal appearance of the gums and the pain experienced. - Prepare a list of questions about gum disease, your symptoms, risk factors, and possible treatments.
- Be prepared to be asked what kind of gum and oral diseases your relatives have.
 3 Relax during your inspection. Your dentist will examine your gums, paying particular attention to their shape and color. The doctor will also check to see if they are bleeding. Your dentist will then use a tiny periodontal probe to check the gaps between your gums and teeth. If they exceed 3-5 mm, this may indicate a disease.
3 Relax during your inspection. Your dentist will examine your gums, paying particular attention to their shape and color. The doctor will also check to see if they are bleeding. Your dentist will then use a tiny periodontal probe to check the gaps between your gums and teeth. If they exceed 3-5 mm, this may indicate a disease. - This procedure is generally painless, although tooth and gum sensitivity may increase due to root exposure.
- The dentist can also check the mobility of the teeth - excessive mobility may indicate insufficient anchorage in the bone.
- You may have an X-ray of your teeth and jaw taken to assess bone loss.
 4 Make a treatment plan. After your dentist diagnoses you with gum disease, you need to work with them to work out the best treatment plan. In the early stages of gingivitis, non-invasive measures are sufficient, while in advanced periodontitis, surgery may be required.
4 Make a treatment plan. After your dentist diagnoses you with gum disease, you need to work with them to work out the best treatment plan. In the early stages of gingivitis, non-invasive measures are sufficient, while in advanced periodontitis, surgery may be required. - In the early stages of the disease, your dentist will recommend removing calculus and cleaning and polishing the tooth root surface. The first procedure involves cleaning the calculus and removing bacteria below the gum line, and the second is smoothing the rough surface of the roots of the teeth so that bacteria do not settle on them.
- For not very advanced stages of gum disease, local or general antibiotics may be recommended.
- Surgery can include flap surgery, gum or bone grafts, and tissue regeneration to heal the disease and prevent it from occurring in the future.
- Another possibility is the derivative of the enamel matrix. In this case, the periodontist applies a special gel to the root of the damaged tooth, which stimulates the growth of bone and other tissues.
 5 Consider alternative treatments. If you are unhappy with the treatment plan, or if you think your dentist is offering you the wrong treatment, try another doctor. Perhaps he will make the same decision, but this way you will once again make sure that he is correct.
5 Consider alternative treatments. If you are unhappy with the treatment plan, or if you think your dentist is offering you the wrong treatment, try another doctor. Perhaps he will make the same decision, but this way you will once again make sure that he is correct.  6 Make an appointment for your next appointment. After your treatment, visit your dentist more often than you did before your illness. To avoid further complications of gum disease, cleanse every three months.
6 Make an appointment for your next appointment. After your treatment, visit your dentist more often than you did before your illness. To avoid further complications of gum disease, cleanse every three months. - Consider restorative treatments (such as coronal lengthening or prosthetics) to improve the appearance of damaged teeth and gums.
- Continue to practice good oral hygiene.
Part 3 of 3: Oral Hygiene
 1 Brush your teeth and gums twice a day. Removing food particles from teeth, gums and tongue reduces the chance of bacteria growing too quickly in the mouth. By multiplying between teeth and gums, bacteria can cause gum disease.
1 Brush your teeth and gums twice a day. Removing food particles from teeth, gums and tongue reduces the chance of bacteria growing too quickly in the mouth. By multiplying between teeth and gums, bacteria can cause gum disease. - Use a soft bristled toothbrush to help you clean your gums without irritating them. Medium to hard bristles can expose teeth below the gum line, allowing bacteria to enter these areas, leading to inflammation.
- Try to brush your teeth after every meal. If this is difficult, rinsing your mouth after eating will reduce bacteria by 30%.
- Change your toothbrush every 1-4 months, as abraded bristles do not remove plaque well and can harbor bacteria.
- Some electric toothbrushes can better clean plaque and calculus from your teeth and gums than conventional toothbrushes.
 2 Use a toothpaste that contains fluoride. Fluoride strengthens teeth and helps to saturate the enamel with minerals, protecting teeth from decay. After a meal, when the mouth is acidic, fluoride inhibits the growth of acid-loving bacteria, thereby protecting the gums.
2 Use a toothpaste that contains fluoride. Fluoride strengthens teeth and helps to saturate the enamel with minerals, protecting teeth from decay. After a meal, when the mouth is acidic, fluoride inhibits the growth of acid-loving bacteria, thereby protecting the gums. - Another common ingredient in toothpastes, triclosan, is antibacterial, reducing the likelihood of gingivitis.
- Metal salts such as zinc and tin can help slightly reduce the appearance of gingivitis.
 3 Floss your teeth daily. Dental floss helps clean up gaps and areas under the gum line where plaque and food debris can collect and cause bacteria to grow. Flossing and then brushing your teeth completely removes harmful bacteria and food particles.
3 Floss your teeth daily. Dental floss helps clean up gaps and areas under the gum line where plaque and food debris can collect and cause bacteria to grow. Flossing and then brushing your teeth completely removes harmful bacteria and food particles. - Thread the floss between your teeth and gently sweep it horizontally to cleanse your gums. Then wrap the floss around each tooth and run it up and down to remove plaque.
- Ordinary wooden or plastic toothpicks are ineffective for cleaning teeth.
 4 Eat a healthy diet. Oral health requires that your diet is nutrient-rich and well-balanced, including fruits and vegetables rich in vitamin C.
4 Eat a healthy diet. Oral health requires that your diet is nutrient-rich and well-balanced, including fruits and vegetables rich in vitamin C. - Drink plenty of water throughout the day. This will flush away plaque and provide enough saliva to fight infection.
- Inadequate nutrition increases the risk of periodontitis.
 5 Quit smoking. Smoking not only increases the risk of gum disease, it also harms overall oral health by causing gum loss and other diseases. The more cigarettes you smoke, the higher your risk of gum disease.
5 Quit smoking. Smoking not only increases the risk of gum disease, it also harms overall oral health by causing gum loss and other diseases. The more cigarettes you smoke, the higher your risk of gum disease. - Smoking a pipe or cigars also increases the likelihood of gum disease.
- Chewing tobacco can cause the gums to recede, allowing bacteria to grow in the vacated areas, leading to periodontitis and tooth loss.
 6 Take care of your health. Gum disease can be associated with many illnesses, especially when oral hygiene is poor. Pay special attention to oral hygiene if you have a chronic medical condition.
6 Take care of your health. Gum disease can be associated with many illnesses, especially when oral hygiene is poor. Pay special attention to oral hygiene if you have a chronic medical condition. - The risk of gum disease is increased with autoimmune diseases such as HIV infection.
- Diabetes mellitus (both type 1 and type 2) significantly increases the risk of gum disease. Diabetes changes blood vessels and increases the content of certain substances that cause inflammation, which increases the risk of periodontitis.
- The risk of gum disease increases with pregnancy and other hormonal changes in the female body, especially if you have diabetes.
 7 Visit your dentist regularly. Early detection of symptoms will help to quickly cope with the disease. In some cases, the symptoms of gum disease are easily recognized, in others they are not. The dentist will be able to spot problems even if they are not so obvious.
7 Visit your dentist regularly. Early detection of symptoms will help to quickly cope with the disease. In some cases, the symptoms of gum disease are easily recognized, in others they are not. The dentist will be able to spot problems even if they are not so obvious. - See your dentist every six months, or more often if you smoke, have diabetes, persistent dry mouth (xerostomia), or are old.
- Go through a periodontologist's examination annually in order to notice a possible deterioration in the condition of the oral cavity in time.
 8 Discuss risk factors with your dentist. Some factors (for example, smoking) can be prevented, while others (genetic predisposition, age) cannot be influenced. After age 35, the risk of gum disease is increased.
8 Discuss risk factors with your dentist. Some factors (for example, smoking) can be prevented, while others (genetic predisposition, age) cannot be influenced. After age 35, the risk of gum disease is increased. - Try to tell your dentist about the cases of oral disease in your family so that he can judge your genetic predisposition to gum disease.
- During psychological stress, the body releases hormones that increase the risk of gum disease.
 9 Check if your fillings and dentures work well for you. Plaque can accumulate in the spaces between them, leading to the multiplication of bacteria. Ask your dentist to check if the fillings and dentures fit well.
9 Check if your fillings and dentures work well for you. Plaque can accumulate in the spaces between them, leading to the multiplication of bacteria. Ask your dentist to check if the fillings and dentures fit well.
Tips
- Diseases of the gums, heart and cardiovascular system share some common risk factors, although more research is needed to identify the link between the two. If you have gum disease, talk to your family doctor.
- Choose a dentist or periodontist you trust. Your teeth are an integral part of your appearance and overall health, so caring for them is extremely important.
Similar articles
- How to cure bleeding gums
- How to treat gum disease with home remedies