Content
- Steps
- Part 1 of 3: Know Your GFR
- Part 2 of 3: Diet and lifestyle changes
- Part 3 of 3: Drug Therapy and Other Therapies
Glomerular filtration rate (GFR) is a measure of how much blood passes through the kidneys in one minute. If the glomerular filtration rate is significantly lower than normal, this indicates a malfunction of the kidneys, leading to the accumulation of toxic metabolic products in the body. In some cases, a person can increase the glomerular filtration rate if they change their diet and lifestyle. However, it must be remembered that a significant decrease in GFR indicates serious health problems - in this case, it is necessary to contact a nephrologist who will prescribe drug therapy and other necessary treatment methods.
Attention:the information in this article is for informational purposes only. Talk to your healthcare professional before using any home remedies or medications.
Steps
Part 1 of 3: Know Your GFR
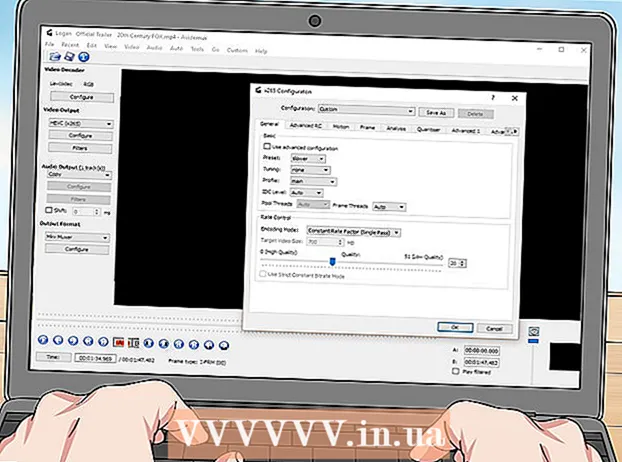
 1 Pass the necessary tests. To determine your glomerular filtration rate, your doctor will order a blood creatinine test. Creatinine is a metabolic end product found in the blood. If the content of creatinine in the analyzed blood sample is significantly higher than the norm, it means that the excretory function of the kidneys is significantly reduced.
1 Pass the necessary tests. To determine your glomerular filtration rate, your doctor will order a blood creatinine test. Creatinine is a metabolic end product found in the blood. If the content of creatinine in the analyzed blood sample is significantly higher than the norm, it means that the excretory function of the kidneys is significantly reduced. - In most cases, therapists prescribe an analysis that allows you to determine the GFR by the clearance (purification factor) of endogenous creatinine, during which the creatinine content in the patient's blood and urine is determined.
 2 Find out what the test results show. The values measured in the creatinine clearance assay are just one of several factors that can be used to assess the glomerular filtration rate. Your doctor will also take into account parameters such as your age, race, gender, and physique to interpret the test results correctly.
2 Find out what the test results show. The values measured in the creatinine clearance assay are just one of several factors that can be used to assess the glomerular filtration rate. Your doctor will also take into account parameters such as your age, race, gender, and physique to interpret the test results correctly. - If the GFR is 90 ml / min / 1.73 m or higher, your kidneys are healthy.
- A GFR between 60 and 89 ml / min / 1.73 m is characteristic of stage II chronic kidney disease (CKD). If the value of this indicator varies from 30 to 59 ml / min / 1.73 m, this indicates the third stage of CKD, a decrease in GFR to 15-29 ml / min / 1.73 m indicates the fourth stage of CKD.
- If the glomerular filtration rate is less than 15 ml / min / 1.73 m, we are talking about end-stage chronic kidney disease (stage 5), that is, the kidneys are unable to perform their functions.
 3 Discuss the situation with your doctor. The doctor will be able to explain in more detail what your test results mean and how it affects your life. If the indicators are significantly below the physiological norm, the therapist will refer you to a nephrologist - a doctor who specializes in kidney disease. After an additional examination, the nephrologist will determine the causes and characteristics of your condition and recommend an individual treatment plan.
3 Discuss the situation with your doctor. The doctor will be able to explain in more detail what your test results mean and how it affects your life. If the indicators are significantly below the physiological norm, the therapist will refer you to a nephrologist - a doctor who specializes in kidney disease. After an additional examination, the nephrologist will determine the causes and characteristics of your condition and recommend an individual treatment plan. - You will need to make some changes in your diet and lifestyle in general, depending on your stage of chronic kidney disease. When it comes to the early stages of the disease, in many cases it is enough to change the lifestyle according to the doctor's recommendations in order to improve the glomerular filtration rate, especially if the patient has not had kidney problems before.
- For advanced stages of CKD, your nephrologist will most likely prescribe medication for you. It should be understood that taking medication alone is unlikely to help solve the problem - treatment should be accompanied by appropriate lifestyle changes.
- If chronic kidney disease has reached the terminal stage, the patient needs regular hemodialysis, and in some cases, kidney transplantation.
Part 2 of 3: Diet and lifestyle changes
 1 Eat more vegetables and less meat. An increase in creatinine and a decrease in GFR usually go hand in hand, and there is an inverse relationship between these parameters. Animal products contain creatine and creatinine, so you will need to reduce your animal protein intake.
1 Eat more vegetables and less meat. An increase in creatinine and a decrease in GFR usually go hand in hand, and there is an inverse relationship between these parameters. Animal products contain creatine and creatinine, so you will need to reduce your animal protein intake. - Plant-based protein contains neither creatine nor creatinine. Eating a predominantly vegetarian diet will also help reduce other risk factors associated with GFR, including diabetes and high blood pressure.
 2 Stop smoking. Smoking increases the amount of toxic substances in the human body, and all these harmful substances pass through the kidney tissue. If you defeat this bad habit, then reduce the load on the kidneys, as a result of which they will become better at eliminating the end products of metabolism.
2 Stop smoking. Smoking increases the amount of toxic substances in the human body, and all these harmful substances pass through the kidney tissue. If you defeat this bad habit, then reduce the load on the kidneys, as a result of which they will become better at eliminating the end products of metabolism. - In addition, smoking causes an increase in blood pressure, which, in turn, has a negative effect on kidney function. To increase GFR, blood pressure needs to be maintained at a normal level.
 3 Try to reduce the amount of salt in your diet. When kidney function is impaired, sodium filtration deteriorates, so a diet high in salt leads to further development of the disease and a decrease in GFR.
3 Try to reduce the amount of salt in your diet. When kidney function is impaired, sodium filtration deteriorates, so a diet high in salt leads to further development of the disease and a decrease in GFR. - Remove salty foods from your diet and, if possible, choose salt substitutes that are low in sodium ions. You can use a variety of spices and herbs as a seasoning for food, not limited to table salt alone.
- Try increasing the amount of homemade, organic foods in your diet and eating fewer processed foods and processed foods. Dishes made with natural products tend to contain less salt, as salt is added to convenience foods during the manufacturing process to increase shelf life.
 4 Reduce the amount of potassium and phosphorus in your diet. Phosphorus and potassium are two other elements whose elimination from the body requires intensive kidney function, which is difficult if the kidney function is already impaired or weakened. Avoid foods rich in these elements; If you are taking any dietary supplements, make sure they are free of phosphorus and potassium.
4 Reduce the amount of potassium and phosphorus in your diet. Phosphorus and potassium are two other elements whose elimination from the body requires intensive kidney function, which is difficult if the kidney function is already impaired or weakened. Avoid foods rich in these elements; If you are taking any dietary supplements, make sure they are free of phosphorus and potassium. - Foods high in potassium: winter squash, sweet potatoes, potatoes, white beans, yogurt, halibut, orange juice, broccoli, cantaloupe melon, bananas, pork, lentils, milk, salmon, pistachios, raisins, chicken, tuna.
- Foods that are high in phosphorus include milk, yogurt, hard cheeses, cottage cheese, ice cream, whole grains, lentils, peas, beans, nuts, seeds, sardines, pollock, cola, and fruit water.
 5 Drink nettle leaf tea. Drinking 250-500 ml (one to two cups) of nettle leaf tea daily will help reduce the amount of creatinine in your body, which in turn will help increase GFR.
5 Drink nettle leaf tea. Drinking 250-500 ml (one to two cups) of nettle leaf tea daily will help reduce the amount of creatinine in your body, which in turn will help increase GFR. - Check with your healthcare professional to see if your health condition allows you to drink nettle leaf tea.
- To make tea from nettle leaves, take two fresh nettle leaves, pour at least 250 ml of boiling water and heat in a water bath for 10-20 minutes. Remove the nettle leaves and drink the cooked broth hot.
 6 Exercise regularly. In particular, cardiovascular exercise improves blood circulation.
6 Exercise regularly. In particular, cardiovascular exercise improves blood circulation. - Note that excessive exercise increases the conversion of creatine to creatinine, which puts additional stress on the kidneys and further decreases GFR.
- The optimal solution would be regular sports loads of medium intensity. For example, you can ride a bike or walk at a brisk pace for half an hour, three to five days a week.
 7 Maintain a healthy weight. More often than not, eating a balanced diet and exercising regularly will be enough to maintain a healthy weight. At the same time, you should not overly limit yourself in food or adhere to a very strict diet, except in cases where the diet is prescribed by the attending physician or nutritionist.
7 Maintain a healthy weight. More often than not, eating a balanced diet and exercising regularly will be enough to maintain a healthy weight. At the same time, you should not overly limit yourself in food or adhere to a very strict diet, except in cases where the diet is prescribed by the attending physician or nutritionist. - Losing excess weight can help improve circulation and blood pressure. In addition, increased blood circulation in the body improves renal blood flow and filtration of toxic substances and fluid in the kidneys. All this has a positive effect on the glomerular filtration rate.
Part 3 of 3: Drug Therapy and Other Therapies
 1 Discuss your treatment plan with your nephrologist. If your nephrologist has diagnosed you with a serious kidney disease, they will put together a special therapeutic diet to follow. In some cases, the doctor recommends that the patient seek additional advice from a dietitian.
1 Discuss your treatment plan with your nephrologist. If your nephrologist has diagnosed you with a serious kidney disease, they will put together a special therapeutic diet to follow. In some cases, the doctor recommends that the patient seek additional advice from a dietitian. - Diet for kidney disease is aimed at reducing the load on the excretory system and allows you to maintain an optimal balance of fluid and minerals in the human body.
- When a doctor draws up a special meal plan for a patient, he takes as a basis the Pevsner diet system, developed for the treatment of various diseases. A diet for a certain group of diseases is called a table and has its own number. Thus, in case of kidney disease, the doctor draws up a diet based on table number 7 (as well as 7a and 7b). Many components of this diet are consistent with the recommendations of this article, in particular, patients are advised to reduce their intake of sodium, potassium, phosphorus and protein.
 2 Determine the underlying cause of your condition. In most cases, chronic kidney disease and a concomitant decrease in GFR are caused by or closely related to other diseases. In this case, it is necessary to diagnose these diseases and take appropriate measures - this will help to increase GFR.
2 Determine the underlying cause of your condition. In most cases, chronic kidney disease and a concomitant decrease in GFR are caused by or closely related to other diseases. In this case, it is necessary to diagnose these diseases and take appropriate measures - this will help to increase GFR. - In most cases, the decrease in GFR is due to high blood pressure or diabetes (and sometimes both).
- If the doctor could not immediately determine the cause of the decrease in GFR, he prescribes additional tests and examinations. Urinalysis, ultrasound, and computed tomography are usually done to diagnose kidney disease. In some cases, the doctor considers it appropriate to order a biopsy of the kidney tissue, when a small tissue sample is taken for detailed microscopic examination.
 3 Drug therapy for kidney disease. When the impaired renal function is caused by another disease, or vice versa, renal disease adversely affects other body systems, the doctor prescribes drug treatment aimed at a comprehensive solution to the problem.
3 Drug therapy for kidney disease. When the impaired renal function is caused by another disease, or vice versa, renal disease adversely affects other body systems, the doctor prescribes drug treatment aimed at a comprehensive solution to the problem. - High blood pressure often leads to decreased GFR. In this case, the patient is prescribed drugs to lower blood pressure: an ACE inhibitor (capoten, captopril, enalapril and other drugs in this group) or angiotensin II receptor blockers (losartan, valsartan and others). These drugs help lower blood pressure and reduce urine protein, thereby helping to reduce the burden on the kidneys.
- In the later stages of CKD, the kidney disrupts the synthesis of erythropoietin, an important hormone of the human body. In this case, the doctor prescribes special drugs aimed at solving this problem.
- In addition, the doctor may prescribe vitamin D or other drugs that control phosphorus levels, since kidney disease prevents the elimination of this element from the body.
 4 Talk to your doctor about other medicines. Any medicine or products of its metabolism are excreted from the body by the kidneys. If you have a decreased GFR, be sure to ask your doctor how any medications you are taking or plan to take in the near future are affecting your kidneys. This applies to both prescription drugs and over-the-counter drugs.
4 Talk to your doctor about other medicines. Any medicine or products of its metabolism are excreted from the body by the kidneys. If you have a decreased GFR, be sure to ask your doctor how any medications you are taking or plan to take in the near future are affecting your kidneys. This applies to both prescription drugs and over-the-counter drugs. - Your doctor will probably tell you not to take non-steroidal anti-inflammatory drugs, including coxibs (Celebrex) and propionic acid derivatives (ibuprofen, naproxen). It has been found that taking these drugs increases the risk of onset and worsening of kidney disease.
- Talk to your doctor before taking any alternative medicine. Natural does not always mean safe, especially for people with kidney disease, so some folk remedies can cause GFR to decline further.
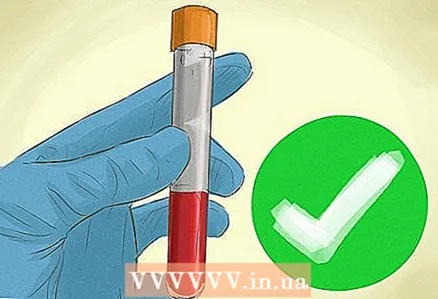 5 Check your GFR regularly. Even if you have managed to restore your GFR to normal, you should periodically get tested and check your GFR throughout your life. This is especially important if your GFR was below normal or if you are at risk for kidney disease.
5 Check your GFR regularly. Even if you have managed to restore your GFR to normal, you should periodically get tested and check your GFR throughout your life. This is especially important if your GFR was below normal or if you are at risk for kidney disease. - With age, kidney function weaken, and the glomerular filtration rate decreases, so the nephrologist will recommend that you undergo regular examinations to observe the dynamics of the process. Depending on the results of the next examination, the attending physician will adjust the drug therapy and dietary recommendations.
 6 Learn about the dialysis procedure. If GFR drops to a minimum and a person develops kidney failure, the patient needs dialysis to remove toxic metabolic products and excess fluid from the body.
6 Learn about the dialysis procedure. If GFR drops to a minimum and a person develops kidney failure, the patient needs dialysis to remove toxic metabolic products and excess fluid from the body. - In hemodialysis, blood is purified through an artificial membrane using an artificial kidney apparatus.
- During peritoneal dialysis, the patient's peritoneum acts as a filtering membrane, and the filtered toxic substances are removed from the abdominal cavity together with special solutions.
 7 Learn about kidney transplant. Kidney transplantation is a surgical procedure performed in patients with end-stage chronic renal disease with extremely low GFR. When a kidney is transplanted, it is necessary that the donor's kidney be compatible in several ways with the recipient's body (the patient to whom the kidney is being transplanted). Quite often, the donor of the kidney is a relative of the patient; in other cases, the donor kidney is taken from a person who is not related to the patient.
7 Learn about kidney transplant. Kidney transplantation is a surgical procedure performed in patients with end-stage chronic renal disease with extremely low GFR. When a kidney is transplanted, it is necessary that the donor's kidney be compatible in several ways with the recipient's body (the patient to whom the kidney is being transplanted). Quite often, the donor of the kidney is a relative of the patient; in other cases, the donor kidney is taken from a person who is not related to the patient. - Sometimes it is not possible for a patient to receive a kidney transplant, even if he is in end-stage renal disease. When doctors decide whether an operation is necessary and appropriate, they take into account many factors, including the patient's age, various physiological parameters, and the presence of other diseases.
- After a kidney transplant, the patient must follow all medical prescriptions, follow a diet and take care of the health of the excretory system in every possible way in order to avoid a repeated decrease in GFR.