Author:
Robert Simon
Date Of Creation:
20 June 2021
Update Date:
24 June 2024

Content
Gestational diabetes occurs in about 9% of pregnant women and usually develops by 24 weeks of pregnancy. Most do not cause noticeable symptoms, but your doctor will likely recommend screening for gestational diabetes as part of the routine prenatal check-up. Glucose is a type of sugar. It is difficult for the cells of women with gestational diabetes to absorb sugar, so it remains in the blood. Increased blood glucose (sugar) causes many health problems for both mother and fetus.
Steps
Method 1 of 4: Follow a diet that controls your weight and blood sugar
Consume recommended calories per day. Women with a normal pre-pregnancy weight should consume around 30 calories / kg / day, based on weight during pregnancy. Women who were obese before pregnancy could reduce their caloric intake by 33%, or about 25 calories / kg / day, based on weight during pregnancy. Remember this is a general guide only. You should talk to your doctor specifically for the best calorie recommendation.
- Buy a food scale to weigh food. This will help you figure out how much a serving is. By reading food labels, you can estimate the amount of calories and macronutrients contained in each serving.
- Track your calorie intake by keeping a food diary. You can use a small notebook as a food diary. Record foods eaten and look up their calories on the internet or guidebook. There are also smartphone apps for easy calorie tracking, such as www.myfitnesspal.com.
- Combine a food diary with regular weight gain to determine whether you are gaining or losing weight.
- If you have not gained enough weight, you should increase your caloric intake to 200-500 calories per day. Continue monitoring to see if your weight has gained correctly.

Keep track of your carbohydrate intake. Carbohydrates are one of the three essential macronutrients besides protein and fat. There are three main types of carbohydrates: sugars, starches and fibers. Sugar is the simplest form of carbohydrates. Sugar includes fructose, glucose, sucrose and several other molecules. Starches are also known as complex carbohydrates and are made up of many types of sugars that link together in chains. Fiber is a type of carbohydrate that the human body cannot break down. When you eat sugar or starches, they are broken down and converted to glucose. Sugar (glucose is a type of sugar) is converted to glucose faster than complex carbohydrates. Fiber is not converted to glucose because it cannot be digested.- There is no definite number of carbohydrates needed by a pregnant woman. Therefore, you should discuss this with your doctor. Monitor your carbohydrate intake along with your blood glucose. If your blood glucose levels are consistently high, you should reduce your sugar and complex carbohydrates intake and increase your fiber intake.
- There is no need to limit fiber. The recommended intake is 20-30 g of fiber per day.
- Keep a food diary to keep track of your carbohydrate intake. Smartphone apps can make it easy to keep track of your carbohydrate and sugar intake.
- Reduce sugar consumption.

Eat carbs in moderate amounts. Even if you consume low-glycemic starches such as barley, oatmeal and quinoa, you should still consume in moderation. Starch is converted to glucose in cells. A good rule of thumb is to consume about one cup of carbs at each meal.
Eat fruit in moderation. Even if you consume fruits with a low glycemic index, you should only consume 1-3 servings of fruit per day. Besides, consume only a portion of the fruit at a time.- Avoid fruits with a high glycemic index like watermelon.
- Avoid consuming canned fruits, soaked in sweet syrups.
- Avoid fruit juices with added sugars.
- Combine fruit with other fatty foods like nuts, peanut butter or cheese to reduce the impact on blood sugar.
Balance your portion sizes throughout the day. Eating too much at a time can raise blood sugar. It is best to divide into 3 main meals, 2-3 snacks throughout the day.
- Bring snacks such as chopped nuts or vegetables to a snack.
- Eat a variety of nutritious foods that contain healthy fats and proteins like avocados, coconut oil, lean meats and nuts.
Method 2 of 4: Exercise to control weight
Exercise in moderation. Exercise not only helps to lower blood glucose, but also changes the cell's response to insulin. Cells become insulin sensitive, meaning the body doesn't have to make too much insulin to help the cells absorb glucose. Cells absorb glucose from the blood which helps to lower blood glucose. Experts recommend 30 minutes of exercise a day for pregnant women.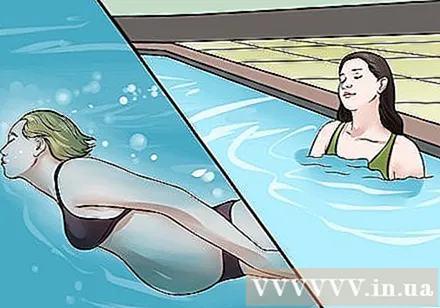
- Talk to your doctor about the type of exercise that's best for you.
- If you haven't been exercising regularly for a long time, start slowly. Start exercising for 10 minutes a few days a week, then gradually increase it to 30 minutes each day.
- Swimming. Swimming is a great exercise for pregnant women. Moving in the water helps to reduce stress in the joints and back.
Move more. You don't have to exercise in the gym. Simple actions like sending the car away from the supermarket / market, taking the stairs or taking the dog for a regular walk are also helpful.
Avoid activities that are potentially dangerous to pregnant women. In addition to most exercises that pregnant women can do, you should avoid certain exercises like crunches or high leg exercises that cause you to lie on your back. These exercises should be avoided during the first 3 months of pregnancy. In addition, you should avoid or limit participation in sports requiring strong exposure that harms pregnant women and their baby, such as martial arts, soccer and basketball. Also avoid sports with a high risk of falling. advertisement
Method 3 of 4: Blood glucose monitoring
Monitor blood sugar (glucose) as recommended by your doctor. Experts recommend daily blood glucose meters to avoid hypoglycemia. This will also help you determine your ideal insulin needs. Learning how to use a blood glucose meter is very important. You should buy a gauge with an easy-to-get test tape. Initially, you will likely have to test your blood sugar 3-4 times a day or even in the evening.
Understand the benefits of insulin therapy. Controlling insulin levels improves carbohydrate metabolism and lowers blood sugar.Insulin therapy is used individually for each case, based on weight, lifestyle, age, family and career support. It's best to follow your doctor's instructions when administering insulin.
Know when to start insulin therapy. If you need medication, your doctor may recommend that you start taking blood sugar control medications such as Metformin or Glyburide. When drug treatment is ineffective, you will be advised to traditional treatment of moderate-acting insulin injections (such as NPH) in the morning and evening, and short-acting insulin injections over a few or all meals . The dose for injection depends on your weight, what is the pregnancy in the third trimester and how much blood sugar is increased. advertisement
Method 4 of 4: Equip yourself with knowledge
Know how much weight to gain. The National Institute of Child Health and Human Development (USA) has a guideline on how much weight should be increased (overall and weekly) for pregnant women based on height, pre-pregnancy weight. pregnancy and fetal number.
- In general, if you are underweight, you can safely gain weight at 16-18 kg.
- If your weight is normal, you can safely gain weight 13-16 kg.
- If you are overweight, you can safely gain weight 10-12 kg.
- If obese, you can safely gain weight 7-9 kg.
- Pregnant women with multiple pregnancies can safely gain weight from 16 to 20 kg.
Know what your blood glucose level needs to be. The American Diabetes Association gives the following guidelines for blood sugar levels to reach in women with gestational diabetes. Remember that each person's blood sugar needs will vary from person to person, so it's important to talk to your doctor first to set appropriate goals.
- Before meals, blood glucose levels should be 95 mg / dL or less.
- One hour after a meal, blood sugar should be 140 mg / dL or less.
- Two hours after a meal, your blood sugar should be 120 mg / dL or less.
Talk to your doctor if you plan to become pregnant. If you plan to become pregnant, you should have an overall health check, including talking to your doctor about the risk of diabetes during pregnancy. Preventive measures that help reduce the risk of diabetes during pregnancy include a healthy diet, staying active, and maintaining a healthy weight before pregnancy. Your doctor can help you come up with a wellness plan when you want to get pregnant.
Recognize the symptoms of high blood sugar. Gestational diabetes causes no symptoms in most pregnant women, but high blood sugar does. If your blood sugar is at 130 mg / dL or higher, you may experience symptoms:
- More thirsty
- Headache
- Blurred vision
- Tired
- Urinate often
- Seek medical attention immediately if you have the above symptoms or high blood sugar reading.
Know the symptoms of hypoglycemia. If you have gestational diabetes and are taking insulin and have the following symptoms, you will need to check your blood sugar. If your measurements are low, you should eat a lozenge or drink some juice. 15 minutes later, continue to measure blood glucose concentration.
- Sweat
- Feeling weak
- Dizziness
- Shivering
- Confusion
- Pale skin
Advice
- You should stay hydrated by drinking at least 8 glasses of water a day.
Warning
- Talk to your doctor if you experience a significant change in weight or not gaining enough weight.
- Untreated gestational diabetes can increase the risk of the fetus being too large, the risk of a cesarean section, problems with infant blood sugar and pre-eclampsia.



