Author:
Lewis Jackson
Date Of Creation:
8 May 2021
Update Date:
1 July 2024

Content
Arthritis is swelling and damage in one or more cavities in the knee joint. Arthritis can be divided into several different forms depending on the cause; Osteoarthritis is a progressive abrasion of the cartilage covering the top of the bone, rheumatoid arthritis is a chronic autoimmune disorder in the lining of the joint. Other types of arthritis may be caused by an infection, an underlying health problem (for example, systemic lupus erythematosus) or from a buildup of uric acid crystals. If you want to know if you have knee arthritis, you need to learn to recognize the signs and symptoms commonly associated with the condition.
Steps
Method 1 of 3: Recognize the signs of knee arthritis
Assess your risk factors. Depending on the type of arthritis, there are many factors that can increase the risk of mass arthritis. Some of these factors are non-modifiable, but there are others you can change to reduce your risk of knee arthritis.
- Genetic. Genetic factors may make you more susceptible to certain types of arthritis (for example, rheumatoid arthritis or systemic lupus erythematosus). If you have a family history of arthritis, you may be at a higher risk of arthritis of the knee.
- Sex. Men are susceptible to gout - a form of arthritis caused by high levels of uric acid in the blood, while women are more susceptible to rheumatoid arthritis.
- Age. The older you get, the higher your risk of arthritis.
- Fat. Being overweight adds pressure to the knee joint and can increase the risk of arthritis.
- History of joint injury. Damage to the knee joint can partly lead to osteoarthritis.
- Infection. Bacteria can infect joints and can make different types of arthritis worse.
- Job. Certain jobs that require you to constantly flex and / or slack your knees can increase your risk of osteoarthritis.
- If you carry one or more of the risk factors for arthritis, you should consult your doctor about the preventive steps to take (or see prevention below).

Know the symptoms of knee arthritis. The most common symptoms of knee arthritis are joint pain and stiffness in the knee. However, depending on the type of arthritis (such as rheumatoid arthritis or osteoarthritis), you may experience other symptoms. To recognize the symptoms of arthritis, be alert if you notice any of the following:- Pain that worsens with activity.
- Reduce or limit the range of motion.
- Stretch your knees.
- Swelling and pain in the knee joint.
- The feeling of a "lack of strength" joint.
- Fatigue and discomfort (often occurring during periods of rheumatoid arthritis flare-ups)
- Mild fever and chills (often present during periods of rheumatoid arthritis flare-ups).
- Joint deformations (knuckles or ankles) are often a more severe symptom of untreated arthritis.

Watch for pain. Knee pain is not always a sign of arthritis. Pain caused by arthritis is usually the inside of the knee, and in some cases the front or back of the knee.- Activities that put pressure on the knee joint like hiking, climbing stairs or standing for long periods of time can make knee arthritis pain worse.
- In severe cases of knee arthritis, pain may appear when you sit or lie down.

Evaluate your range of motion and feeling of tension. Besides pain, arthritis also reduces the range of motion in the knee. Over time, as the sliding surface of the bones decreases, you may feel your knees stiffen and your movement is limited.- As the cartilage on one side of the knee wears off, you may find that the knee is bent inward or the wall of the foot is arched.
Watch for swelling or creaking. Swelling is another sign of inflammation (in addition to pain, warmth, and redness) and is a common symptom of knee arthritis. In addition, a person with knee arthritis may actually feel or hear a creak or creak inside the knee joint.
Note if symptoms change or worsen. Symptoms of arthritis can come on gradually and often progress as the disease gets worse. Learning to recognize the progression of arthritis symptoms can help distinguish arthritis from other pain in the knee.
- People with rheumatoid arthritis often experience worsening episodes of symptoms called "flare-ups". During these stages, symptoms worsen, peak, and then subside.
Seek medical advice. If you experience one or more of these symptoms, ask your doctor if you have arthritis of the knee.
- Your doctor will check for swelling, redness, and warmth in your knee and evaluate the range of motion. If your doctor suspects you have arthritis, your doctor may recommend some of the following tests to confirm the diagnosis:
- Tests to analyze traces of arthritis in the blood, urine and / or joint fluid. Joint fluid is collected by inserting a needle into the space in the joint and suctioning it.
- Ultrasound images of the soft tissues, cartilage and fluid-bearing structures in the knee. Ultrasound can also be used to guide needle insertion during joint aspiration.
- X-rays show cartilage loss, bone damage and / or spikes.
- Computerized tomography (CT) scan to visualize the bones in the knee. CT images are taken from many different angles of the joint and then combined together to create cross sections of the internal structure.
- Magnetic resonance imaging (MRI) can be used to produce more detailed cross-sectional images of the surrounding tissue such as cartilage, tendons and ligaments of the knee.
- Your doctor will check for swelling, redness, and warmth in your knee and evaluate the range of motion. If your doctor suspects you have arthritis, your doctor may recommend some of the following tests to confirm the diagnosis:
Method 2 of 3: Prevent knee arthritis
Weight loss. Although many people find it difficult, losing weight is probably one of the most important steps in treating arthritis. Reducing the weight the knee will bear, reducing pressure and damage to the joint can help reduce the risk of osteoarthritis.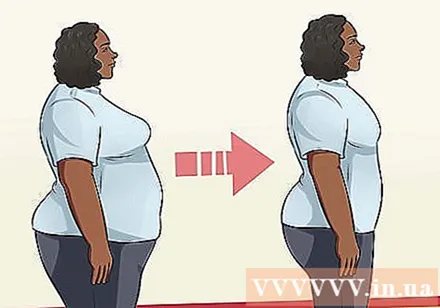
Adjust activities. You may need to limit some activities and learn new methods of exercise to prevent or reduce joint damage.
- Water exercise is a great option for those suffering from joint problems.
- Using a crutch or a cane on the side of your leg opposite the inflamed knee will help reduce pressure on the joint.
Drink joint supplements. Many joint supplements contain molecules that are naturally produced in the body, such as glucosamine and chondroitin sulfate, which are important for maintaining healthy knee cartilage.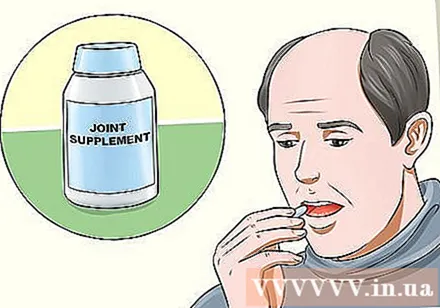
- While it can be controlled pain, joint supplements do not help regenerate cartilage. The reliable studies show that the supplement is no better than a placebo, but the risk is the lowest (but the price is higher). So, most orthopedic experts advise to try it.
- Some doctors recommend taking joint supplements for 3 months to see if they help.
- Over-the-counter joint supplements are generally not regulated by the US Food and Drug Administration (FDA). Therefore, you should consult your doctor before taking it.
Method 3 of 3: Treatment of knee arthritis
Physiotherapeutic treatment. Strengthening the muscles around the knee joint can help reduce pressure on the knee. Preventing muscle atrophy is an important part of maintaining proper knee function and reducing further damage to the joint.
Take anti-inflammatory medication. Prescription and over-the-counter anti-inflammatory pain relievers (such as nonsteroidal anti-inflammatory drugs or NSAIDs) are medications that help treat pain and inflammation in the joints.
- Always consult your doctor before trying to treat arthritis with over-the-counter medications, especially if you are taking other arthritis medications.
- Absolutely do not exceed the recommended dose, including over-the-counter anti-inflammatory drugs. An overdose of NSAIDs can be life-threatening.
Get a hyaluronic acid injection into the knee. Hyaluronic acid helps lubricate the joint and is naturally present in the fluid of the knee joint. If you have arthritis, the hyaluronic acid in the knee becomes thinner and less effective.
- Your doctor may recommend injecting hyaluronic acid (also called artificial joint fluid or injectable slime) into the knee joint.
- While not always effective, injections of hyaluronic acid can help relieve symptoms within 3-6 months.
Ask your doctor if you should take corticosteroids or a slow acting anti-rheumatic drug. There are a number of prescription medications used to treat arthritis. Consult with your doctor if you can take these medications to treat arthritis.
- Slow acting anti-rheumatic drugs (such as Methotrexate or Hydroxychloroquine) slow or prevent the immune system from attacking the joints.
- Probiotics (eg Etanercept and Infliximab) attack many protein molecules involved in the immune response leading to arthritis.
- Corticosteroid medications (eg, Prednisone and Cortisone) reduce inflammation and suppress the immune system. It can be taken by mouth or injected directly into the painful joint.
Ask your doctor if surgery is needed. If traditional treatments don't relieve joint pain or aren't enough to prevent further damage, you may need surgery, such as a joint alignment or replacement.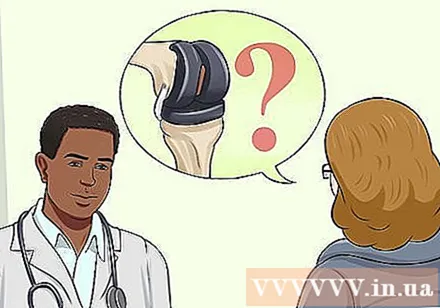
- During osteoarthritis, the doctor removes the ends of the two bones in the joint, and then locks the ends together until they heal into a hard bone.
- During joint replacement surgery, your doctor will remove the damaged joint and replace it with an artificial joint.
Advice
- If you suspect that you are having early signs of arthritis, you should see your doctor right away. Early treatment can change the progression of some types of arthritis.
- The treatment of knee arthritis should start with the most basic steps and then move on to more complex steps, which may include surgery.
- Not every treatment is suitable for every patient, so talk with your doctor to determine which treatment is right.