Author:
Lewis Jackson
Date Of Creation:
13 May 2021
Update Date:
1 July 2024

Content
Root bone resorption is a condition in which the bones supporting the teeth are shrinking, causing the teeth to become loose in the alveoli. Without treatment, you may lose your teeth because the remaining bone is not enough to support the teeth. Root osteoporosis is most commonly associated with the following conditions: severe gum problems (periodontal disease), osteoporosis and type 2 diabetes. Although surgery is often necessary in correcting bone resorption Root root is serious, but you can prevent this by maintaining good oral hygiene and early detection of signs and symptoms of root osteoporosis.
Steps
Method 1 of 3: Corrected with medical methods
Use a bone transplant to fix bone resorption. It is very difficult to restore lost root bones. Right now, a bone transplant is the only way to completely restore the root bone. With bone graft surgery, the wound usually heals within 2 weeks.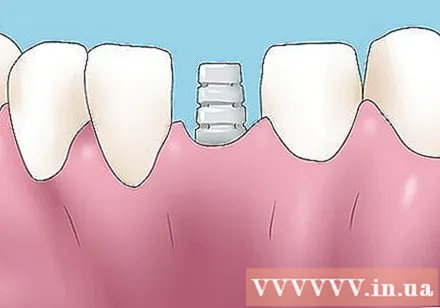
- It may take 3-6 months to see the results of the bone transplant procedure.
- Bone graft surgery to overcome root bone resorption can be divided into the following three main types.
Bone-building implants to stimulate bone regeneration. During this surgery, the bone is removed from a source (jaw area, lower jaw, etc.) and transferred to the area of the root bone that is missing. The newly transplanted bone cells will begin to multiply and build new bones to replace the missing bone.- The gold standard in bone transplant surgery is taking bone from a location in a patient's body and transplanting it into the site of the missing bone.
- This technique allows the body to more easily accept new bone cells because it is recognized as its own cells.
- Bone marrow transplant surgery is often used in osteoporosis.

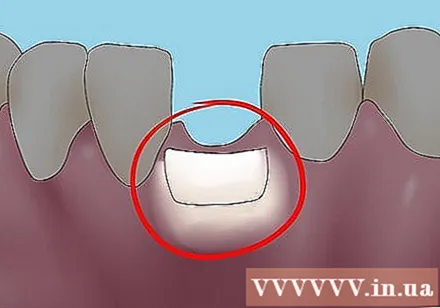
Consider osteoporosis surgery to provide a framework for bone formation. During this process, a piece of bone is inserted into the site of the missing bone. Grafted bone fragments make the framework for bone-forming (osteoblasts) cells to grow and multiply.- Biomedical glass is an example of a framing material.
- Along with the bone graft, biomedical glass is grafted into the missing bone to rebuild the root bone.
- The biomedical glass will provide the framework for the bone graft to grow and build bones. They also induce growth factors to support more effective bone formation.
Using bone conduction to stimulate stem cell growth. In this technique, grafted bone fragments, such as demineralized bone (DBM) taken from the bone bank, are inserted into the site of the missing root bone. The DBM fragments stimulate stem cells to grow where bone is lost, and these stem cells will convert into osteoblasts (bone-forming cells). These osteoblasts will repair bone defects and create new root bones.- The use of DBM pieces from the dead is legal and safe. The transplants will be thoroughly disinfected before transplanting.
- Once it is determined that the transplant is safe, tests are done to make sure the piece is suitable for the recipient.
- This is an important factor in ensuring that the graft is not rejected by the body.
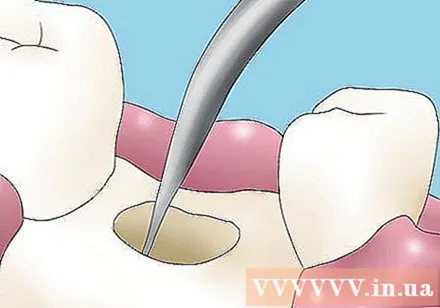
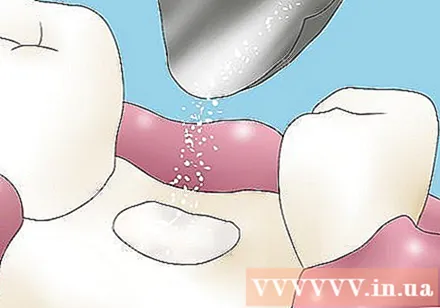
Shave tartar under your gums to treat infections that cause bone loss. Under-gum tartar scraping or root cleaning is a deep cleaning technique that diabetics often need. With this procedure, the root area will be thoroughly cleaned to remove infected root parts caused by bacteria that cause bone loss. After shaving tartar under the gums, gum disease will be controlled and root bone resorption also ceases.- If you have diabetes, your recovery may be impaired and you must take precautions like antibiotics and antibacterial mouthwashes.
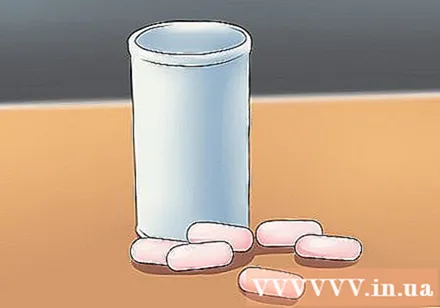
- You may be prescribed doxycycline 100mg / day for 14 days to make up for a poor immune system.
- Chlorhexidine mouthwash may also be prescribed by a doctor to kill bacteria that cause serious gum disease. You will rinse your mouth with 10 ml of 0.2% chlorhexidine (Orahex®) for 30 seconds for 14 days.
Use estrogen supplement therapy to prevent osteoporosis. Estrogen can help prevent osteoporosis and maintain bone mineral levels by slowing bone loss. Hormone replacement therapy may also reduce your risk of heart disease and fractures. There are several ways to take estrogen supplements, the most common being:- Estrace: 1-2 mg daily for 3 weeks
- Premarin: 0.3 mg per day for 25 days
- The estrogen patches listed below are used in estrogen supplement therapy. These patches are placed on the abdomen, below the waist:
- Alora
- Climara
- Estraderm
- Vivelle-Dot
Method 2 of 3: Prevent root bone resorption
Prevent root bone resorption by keeping good oral hygiene. To avoid costly bone grafting surgery, you need to prevent root bone resorption. This is pretty easy, as long as you take the necessary steps correctly. All you need to do is keep good oral hygiene and follow some simple steps:
- Brush your teeth thoroughly after every meal - brush your teeth at least 2 times a day to prevent gum disease. Brushing is a way to remove plaque that causes gum disease and root bone resorption.
- Floss after brushing your teeth. Flossing can remove the plaque that remains after brushing. Flossing is imperative after brushing, as plaque may remain in areas where the bristles cannot reach.
Visit the dental clinic periodically to clean your teeth. Tooth decay is one of the leading causes of root bone resorption. You can prevent tooth decay by visiting your dentist periodically for a thorough cleaning and thorough dental care.
- To preserve root bones, you need to keep all your teeth healthy.
- Visit your dentist every 6 months for a periodic cleaning of your teeth, a must for maintaining good oral hygiene.
- Talk to your dentist regularly so they can help you monitor your oral health and prevent gum problems.
- You may also have x-rays to identify areas with bone resorption.
- If you skip the routine dental exams, it is possible that root bone resorption is only detected when it is in the irreversible stage.
Brush your teeth with fluoride toothpaste. Fluorine toothpaste can protect teeth and gums from root bone loss by providing essential minerals to bones and enamel.
- The use of extra fluoride in addition to toothpaste is not recommended, as this can lead to other health problems.
- Use fluoride toothpaste once a day, other times regular toothpaste can be used.
- Do not let children under 10 years old use fluoride toothpaste.
Increase your calcium intake to support tooth health. Calcium is an essential nutrient for bones, including teeth. Calcium-rich foods and calcium supplements will help your body get the calcium it needs to build and strengthen bones and teeth, increase bone density and reduce the risk of root bone resorption and fractures. bone.
- Foods such as low-fat milk, yogurt, cheese, spinach and soy milk are rich in calcium and play an important role in maintaining the strength of teeth and bones.
- Calcium is also available as a dietary supplement.
- Take 1 capsule (Caltrate 600+) after breakfast and 1 capsule after dinner. If you miss a dose, take it as soon as you remember.
Get enough vitamin D for good calcium absorption. You can take vitamin D supplements or sunbathe to ensure proper vitamin D levels are maintained in your body. Vitamin D helps increase bone density by assisting the body to absorb and retain calcium.
- To determine if you have a vitamin D deficiency, ask your doctor about a blood test to measure the amount of vitamin D in your blood.
- Results below 40ng / ml indicate a deficiency of vitamin D in the blood.
- The normal vitamin D level should be in the blood at 50 ng / ml.
- Take vitamin D foods each day with a dose of 5,000 IU.
- To determine if you have a vitamin D deficiency, ask your doctor about a blood test to measure the amount of vitamin D in your blood.
Method 3 of 3: Understand risk factors and detect symptoms early
Recognize the signs and symptoms of root root condition for effective treatment. Root bone disease in the early stage is difficult to determine if only observing teeth. Dentists often have to do x-rays or computed tomography to determine if the bones are atrophy. If you haven't seen your teeth in a while, chances are you will only know you have root bone resorption when the disease is advanced.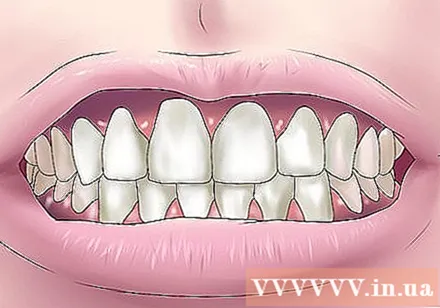
- You may notice some changes with root bone resorption. These changes occur because the bones shrink and the ability to support the teeth becomes ineffective. Note that these changes only evolve over time:
- Dislocation of bites
- Creates spaces between teeth
- The tooth feels loose and may be loose.
- Teeth crooked
- Spindle teeth
- The feeling of biting is different than before
Understand that gum disease is the leading cause of root bone resorption. Periodontal disease or serious gum disease caused by bacteria living on the plaque leads to root bone resorption. Bacteria present in the plaque will reside in the gums and secrete toxins that cause the root bones to shrink.
- In addition, the immune system also contributes to the destruction of root bones in the process of killing bacteria. This is because immune cells secrete substances (such as matrix metalloproteinases, IL-1 beta, prostaglandin E2, TNF-alpha) that can speed up bone loss.
Know that diabetes contributes to an increased risk of bone loss. Diabetes is a disease that lacks the ability to produce insulin (type 1) and is resistant to insulin (type 2). Both types of diabetes lead to serious gum problems and can lead to root bone resorption.
- Diabetic patients have high blood sugar, which facilitates the growth of bacteria that cause root bone resorption.
- People with diabetes lack defense because weak white blood cells make them more susceptible to infection.
Understand that osteoporosis contributes to weak bones and overall bone loss. Osteoporosis is a disease that commonly occurs in women over the age of 60, when bone density decreases. This drop is due to an imbalance of calcium - phosphate, which helps maintain bone mineral levels, associated with decreased estrogen levels.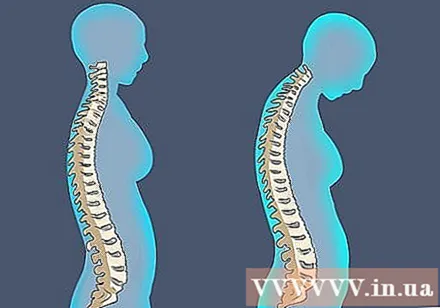
- The decrease in overall bone density also affects the teeth bones, leading to the risk of root bone resorption.
Remember that extraction can lead to root bone resorption. Root bones often shrink as soon as the tooth is lost. After the tooth is pulled, a blood clot forms and white blood cells move to where the tooth was extracted to clean bacteria and damaged tissue. A few weeks later, new cells will arrive to resume the cleaning process. These cells (osteoblasts) can stimulate bone formation.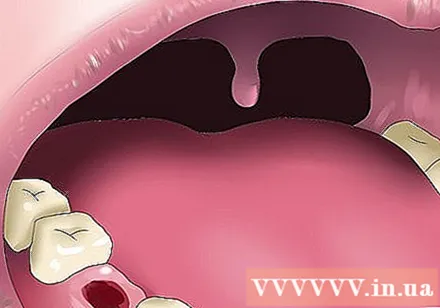
- However, these cells will only work if the teeth are still present, as they require supporting bone. If the teeth are lost, bone function is lost and the cells cannot build new bone.