Author:
Randy Alexander
Date Of Creation:
4 April 2021
Update Date:
1 July 2024

Content
The two muscles that combine to form the calf are the slipper muscle in a deeper position and the lower abdominal muscle (closer to the skin). These muscles connect the heel to the hamstrings, which act as ankle flexion and knee stretching which is essential for movements such as walking, running, jumping and kicking. Calf injuries usually occur in the middle of the leg and / or in the abdominal muscles. Muscle strains are categorized as Grade I (tearing some muscle fibers), Grade II (with severe muscle fiber damage) or Grade III (complete rupture of the muscle). It's important to diagnose calf strain because it determines the treatment regimen you need to follow.
Steps
Part 1 of 4: Consult a therapist
Make an appointment with your doctor. If your calf pain doesn't go away after a few days, you need to see a general practitioner. Your doctor will examine your leg and calf and ask about your lifestyle and the cause of the injury. Your doctor may also order an X-ray of your lower leg (to rule out fractures of the tibia and fibula). If necessary, your doctor will refer you to a more specialized trained musculoskeletal specialist.
- Other health professionals who can help diagnose and treat musculoskeletal injuries are osteoarthritis doctors, physiotherapists, and massage therapists. However, you should initiate a visit with a general practitioner to rule out other serious causes of pain such as blood clots, damage to blood vessels, bursa cysts, or emergency surgery. like chamber compression syndrome.

See a podiatrist. Calf muscle injuries are usually mild I grade muscle strains, but there are cases that require surgery if the muscle is severely torn. Furthermore, certain medical conditions can cause calf or surrounding pain such as fractures, bone cancer, osteomyelitis, venous insufficiency, sciatica caused by lumbar disc herniation or complications. related to diabetes. As such, you may need medical specialists such as a chiropractor, a neurologist, or a therapist (a muscle and bone specialist) to rule out the most serious causes. calf muscle pain.- X-rays, bone scans, magnetic resonance imaging, CT scans and ultrasound are all tools doctors can use to help diagnose pain in your legs.
- Calf muscle injuries often occur in tennis, basketball, soccer, volleyball and race athletes.

Understand the different treatments. Ask your doctor for a clear explanation of the diagnosis, especially the cause (if possible), and give you many options for treatment. Rest and home remedies (such as ice packs) are suitable for mild to moderate strains of calf muscles.- Search for information on calf muscle injuries on the internet (look for reputable medical websites only) to learn more about the condition and to learn about treatments and outcomes.
- Factors that may put a person at risk for muscle strain include advanced age, previous muscle damage, lack of flexibility, lack of flexibility, and exhaustion.
Part 2 of 4: Treatment of I degree muscle tension
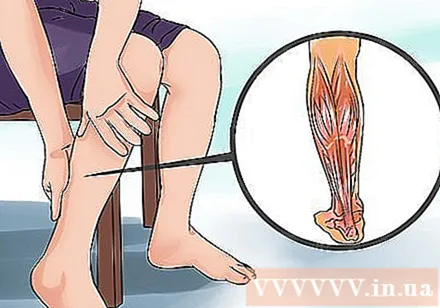
Determine the severity of the injury. Most muscle strains are usually mild and go away on their own within a week. Pain, difficulty with movement, and bruising are all indications of how severe the injury is. A grade I strain is a case of small tears with less than 10% of the muscle fibers being torn. This is characterized by mild pain in the calf, usually from the middle of the calf to near the elbow. Movement is somewhat limited and weak. You are still able to walk, run or play sports, despite the feeling of tension and discomfort.- Muscle tension occurs when the force exerted by the muscle is so strong that the tissue tears, most commonly between joints, where the muscles taper into tendons.
- Most Grade I calf strains will cause discomfort 2 to 5 days after injury, but it can take several weeks to fully recover, depending on the rate of muscle fiber damage and treatment.
Use treatment regimen R.I.C.E.. The most effective treatment regimen for most muscle strains / sprains is R.I.C.E., the first letters of rest, ice, compression and elevation (raise). The first step is rest - temporarily stop all activities to address your injury. Then, cold therapy (ice wrapped in a thin towel or frozen gel bag) is used to apply to the sore area as soon as possible to prevent internal bleeding and reduce inflammation, preferably when the feet are restrained on a chair. or a stack of pillows (also for anti-inflammatory). Apply ice every hour for 10-15 minutes, then reduce the number of compressions once the swelling and pain subsides for a few days. Applying ice to the injury with an elastic bandage or pillow will also help stop bleeding due to torn muscle fibers, and reduce inflammation.
- Do not tie the compression bandage too tightly or leave it on for more than 15 minutes at a time as complete blocked blood circulation can damage your legs.
Take an over-the-counter pain reliever. Your doctor may recommend that you take anti-inflammatory medications like ibuprofen, naproxen or aspirin, or common pain relievers like acetaminophen to fight inflammation and relieve pain associated with calf damage.
- Remember that these medications will be harmful to the stomach, liver and kidneys, so don't take them for more than 2 weeks at a time unless directed by your doctor.
Do leg muscles stretching exercises. Mild muscle strains respond well to light stretching by reducing muscle tension and assisting with blood circulation. After the inflammatory phase of muscle tension, some scar tissue forms; These tissues are not as flexible as muscle fibers. Stretching helps repair scar tissue and makes them more flexible. You can do this exercise by using a towel or bandage around the soles of your feet near your toes, then holding the ends of the towel and pulling in, while slowly stretching your legs and noting the feeling of deep stretch. calf muscles - hold for about 20-30 seconds and slowly relax.Practice 3 to 5 times a week if it doesn't increase calf pain.
Consult with your doctor or therapist before practicing this exercise and be very careful, as exercise can sometimes make the situation worse and prolong the healing time.
- Warming and stretching your calf muscles before doing any sport can help prevent injuries like muscle strains, sprains and cramps.
Part 3 of 4: Treatment of Grade II calf strains
Distinguish between strain legs and sandals. With severe muscle tension, it is important to distinguish which muscle is damaged more: the sandal muscle is in a deeper position or the "head" of the abdominal muscle is in a shallower position. Imaging of magnetic resonance imaging or diagnostic ultrasound is needed for the most accurate diagnosis of the location and extent of the lesion. Level II muscle strains are more severely damaged, and the number of torn muscle fibers can be as high as 90%. These lesions manifest with more severe pain (described as throbbing pain), loss of strength, and a markedly limited range of motion. The swelling is more severe and bruises develop more rapidly due to internal bleeding from torn muscle fibers.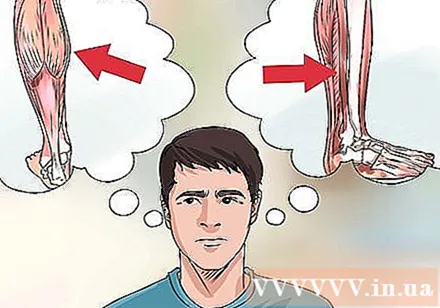
- Type II strains have limited mobility, especially jumping and running, so you'll have to avoid these activities for a while (weeks or more).
- Abdominal muscles are considered to be high risk because it connects 2 joints (knee and ankle) and has a high proportion of rapidly contracting muscle fibers (group 2).
- The middle end of the calf muscles is usually more stretched than the side head.
Apply treatment regimen R.I.C.E.. This regimen is also suitable for the treatment of Grade II strains, but you may need to apply ice to the calf for a little longer (20 minutes at a time) if the damage is mainly to a deeper sandal site. Instead of just applying the R.I.C.E regimen for a few days, such as during a grade I strain, this case requires attention to a week or more.
- Most Grade II calf strains will cause discomfort between 1 and 2 weeks after the injury, depending on the proportion of muscle fibers damaged and the treatment method. This damage takes 1 to 2 months before you can fully return to sports activities.
- In severe and moderate muscle strains, anti-inflammatory drugs should be avoided within the first 24 hours because of the risk of bleeding due to antiplatelet effects (blood thinning).
Use physiotherapy. Grade II muscle strain is a serious damage to skeletal muscles, more likely to form scar tissue, and significantly reduces endurance and range of motion. So, after the swelling, bruising, and pain have subsided significantly, ask your doctor to refer a sports therapist or physiotherapist. They can provide you with endurance exercises, tailor-made stretches, massage techniques, and other treatments such as therapeutic ultrasound (to reduce inflammation and destroy adhesion of scar tissue) and muscle stimulation with electrical impulses (to strengthen muscle fibers and stimulate blood circulation).
- You are allowed to resume all activities once the pain is gone, the range of movement of the legs is back to maximum and the calf muscles are fully restored, which usually takes a few weeks or more.
- Calf strain is most common in men, between the ages of 30 and 50.
Part 4 of 4: Treatment of third degree leg muscle tension
Seek immediate medical attention. Grade III muscle strain is a complete rupture of the muscle or tendon. This is characterized by severe pain (a burning sensation and / or throbbing pain), immediate severe inflammation and bruising, muscle spasm, and sometimes a "pop" sound when the muscle is cut. You may also feel a bulge in your calf, as a large part of the muscle contractes strongly when cut. Inability to walk is characteristic of Grade III calf strains, so someone needs help getting it to the hospital or medical facility. Muscle fibers cannot heal on their own, even with the help of scar tissue, so urgent medical intervention is needed.
- A sudden rupture of a tendon (such as the Achilles tendon) often causes intense pain, like someone slipping from behind or attacking you with a sharp object.
- Severe muscle strains often cause bruises to build up in the feet and turn bluish-black.
Repair surgery. Type III (and some II strains) strains may require surgery to repair and reconnect damaged calf muscles and / or tendons. Time is of the essence, because the longer a muscle is broken and contracted, the more difficult it is to relax and restore normal muscle tone. Furthermore, internal bleeding can cause local necrosis (surrounding tissue death) and potentially (although very rarely) lead to blood loss anemia. In case of fracture between corn will heal faster because of a better blood supply, whereas a tendon rupture will take longer to heal due to not receiving much blood circulation. Apply R.I.C.E. treatment regimen. following surgery.
- In the case of a complete rupture, it takes about 3 months for the calf muscles to heal after surgery and restore mobility.
- After surgery, you may need to use leg braces and crutches for a short time before starting physical therapy exercises.
Take some practice time to rehabilitate. As is the case with grade II muscle tension, physical therapy is an essential method in the recovery of grade III sprains, especially in the presence of surgical intervention. With the guidance of a physiotherapist, isotonic, isometric and then functional exercises will be continually replenished as each exercise is completed without pain. These exercises will strengthen the calf muscles. You can gradually return to sports for 3-4 months, although there is a higher risk of injury again.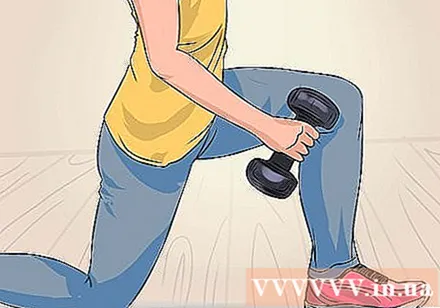
- Poor biomechanics and posture of the foot also contribute to calf muscle damage, so you may need a specially designed foot orthotic after recovery to prevent other problems. could happen.
Advice
- Put the heel pad in the shoe for a few days to elevate the heel and help shorten the injured calf muscles, which can reduce tension and pain somewhat. But don't forget it; Using the foot pads for too long can cause achilles tendon to contract and permanent ankle stiffness.
- Ten days after the injury, the growing scar will stretch similar to the adjacent muscle, and rehabilitation exercises can be initiated under the guidance of a doctor and a physical therapist.