Author:
Robert Simon
Date Of Creation:
24 June 2021
Update Date:
1 July 2024

Content
- To step
- Part 1 of 4: Identifying common symptoms
- Part 2 of 4: Estimating possible risk factors
- Part 3 of 4: Go to the doctor
- Part 4 of 4: Treating the disease
- Tips
- Warnings
If you have painful or sensitive testicles, it makes sense to worry a bit. Epididymitis, or epididymis, can be the cause of this. Epididymitis is usually caused by a sexually transmitted infection (STI), and it is often treatable with a course of antibiotics. Always see a doctor if you have painful, tender or swollen testicles.
To step
Part 1 of 4: Identifying common symptoms
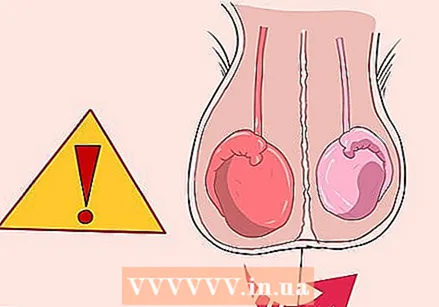 Watch for testicular pain starting on one side. In epididymitis, the pain often starts on one side, and not on both sides at the same time. Over time, the pain can spread to both sides. You usually get pain at the bottom of your testicle at first, but later it spreads to the entire testicle.
Watch for testicular pain starting on one side. In epididymitis, the pain often starts on one side, and not on both sides at the same time. Over time, the pain can spread to both sides. You usually get pain at the bottom of your testicle at first, but later it spreads to the entire testicle. - What kind of pain it is depends on how long the epididymis has been inflamed; it can be a sharp or burning pain.
- If the pain comes on very suddenly in both testicles at the same time, it is usually not an epididymitis. In any case, go to the doctor as soon as possible.
 See if the testicle is red or swollen. The swelling or redness can be on one side or spread to both sides over time. Your testicle may also feel warm, and sitting may hurt from the swelling.
See if the testicle is red or swollen. The swelling or redness can be on one side or spread to both sides over time. Your testicle may also feel warm, and sitting may hurt from the swelling. - The testicle may be red because more blood is flowing to the area, and the swelling may be caused by more fluid leaking to the affected area.
- You may also feel a fluid-filled bump on your testicle.
 Watch for urination problems. Maybe urinating hurts when you have this condition. You may also have to urinate more often than usual, or you may find it difficult to hold it down.
Watch for urination problems. Maybe urinating hurts when you have this condition. You may also have to urinate more often than usual, or you may find it difficult to hold it down. - There may also be blood in your urine.
- Epididymitis is often caused by an infection that starts in the urethra and then spreads to the testicle. Inflammation of the urinary tract can irritate the bladder, causing it to hurt.
 Watch for urethral discharge. Sometimes a transparent, white or yellowish discharge comes out of your penis due to the inflammation of the urinary tract. This symptom usually means the infection was caused by an STI.
Watch for urethral discharge. Sometimes a transparent, white or yellowish discharge comes out of your penis due to the inflammation of the urinary tract. This symptom usually means the infection was caused by an STI. - Do not worry. Even if it is caused by an STI, you can usually treat it properly.
 Measure your body temperature to see if you have a fever. If an infection spreads through the body, you can develop a fever as a defense mechanism. You can also get chills.
Measure your body temperature to see if you have a fever. If an infection spreads through the body, you can develop a fever as a defense mechanism. You can also get chills. - Fever is the body's way of fighting infection. If you have a very high fever, you should call your doctor.
 Keep a record of how long you have been bothered by the symptoms. Acute epididymitis is characterized by symptoms lasting less than 6 weeks. Symptoms that last longer indicate chronic epididymitis. Let your doctor know how long you have been experiencing symptoms as this is important for treatment.
Keep a record of how long you have been bothered by the symptoms. Acute epididymitis is characterized by symptoms lasting less than 6 weeks. Symptoms that last longer indicate chronic epididymitis. Let your doctor know how long you have been experiencing symptoms as this is important for treatment.
Part 2 of 4: Estimating possible risk factors
 Consider if you have had unsafe sex recently. This infection can be the result of a sexually transmitted disease, so unsafe sex, especially with alternate partners, puts you more at risk for epididymitis. If you have recently had unsafe sex and are experiencing symptoms, you may have this condition.
Consider if you have had unsafe sex recently. This infection can be the result of a sexually transmitted disease, so unsafe sex, especially with alternate partners, puts you more at risk for epididymitis. If you have recently had unsafe sex and are experiencing symptoms, you may have this condition. - Always use a condom during intercourse, even if you are not having vaginal sex. You must protect yourself whether you are having oral, anal or vaginal sex.
- Epididymitis is often caused by STIs such as chlamydia, gonorrhea and certain bacteria that can be passed on during sex.
 View your recent medical history, such as surgeries and catheters. The frequent use of catheters can lead to urinary tract infections and epididymitis. Recent surgery near the groin can also cause this condition, so see your doctor if you think this may be the case for you.
View your recent medical history, such as surgeries and catheters. The frequent use of catheters can lead to urinary tract infections and epididymitis. Recent surgery near the groin can also cause this condition, so see your doctor if you think this may be the case for you. - An enlarged prostate, a fungal infection and the use of the drug amiodarone (for atrial fibrillation) can also cause this condition.
- Chronic epididymitis is often associated with granulomatous diseases such as tuberculosis.
 Consider if you recently injured your groin. Although it is not very common, an injury to the groin, for example due to a kick or knee in the testicles, can lead to this condition. If you've recently injured that area and are experiencing symptoms, you may have epididymitis.
Consider if you recently injured your groin. Although it is not very common, an injury to the groin, for example due to a kick or knee in the testicles, can lead to this condition. If you've recently injured that area and are experiencing symptoms, you may have epididymitis.  Know that a cause is not always found. While there may be other rare causes such as TB or mumps, the doctor may also find no cause at all. Sometimes the disease develops for no apparent cause.
Know that a cause is not always found. While there may be other rare causes such as TB or mumps, the doctor may also find no cause at all. Sometimes the disease develops for no apparent cause. - Whether or not a cause is found for the problem, it is not up to your doctor to judge you. He or she just wants to make you better.
Part 3 of 4: Go to the doctor
 If you are experiencing symptoms, see a doctor. Whether or not you have epididymitis, you will still need to see your doctor if you have painful, swollen, tender or red testicles, or if you have trouble urinating.
If you are experiencing symptoms, see a doctor. Whether or not you have epididymitis, you will still need to see your doctor if you have painful, swollen, tender or red testicles, or if you have trouble urinating. - If you experience symptoms, make an appointment with your doctor as soon as possible.
- Be prepared to talk about your recent medical history, as well as your sexual history.
 Be prepared for a physical exam. The doctor will want to look at your genitals and feel the affected testicles. This can be a bit uncomfortable, but it is necessary for the correct diagnosis. If you're a little scared, know that you're really not alone, as most people feel uncomfortable in situations like this.
Be prepared for a physical exam. The doctor will want to look at your genitals and feel the affected testicles. This can be a bit uncomfortable, but it is necessary for the correct diagnosis. If you're a little scared, know that you're really not alone, as most people feel uncomfortable in situations like this. - Your doctor will look for pain in your lower back and see if you have kidney or bladder infections that could be contributing to the epididymitis. He / she can also take a urine sample to check if you have a urinary tract infection.
- Your doctor may want to do a rectal exam to check your prostate.
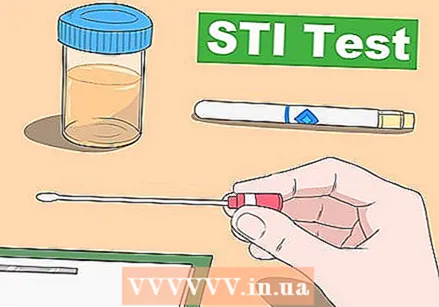 Get tested for STDs. Since this infection can be caused by an STI, your doctor may want to test you for it as well. Usually you will have to give some urine, and sometimes the doctor will take a smear from the inside of your penis.
Get tested for STDs. Since this infection can be caused by an STI, your doctor may want to test you for it as well. Usually you will have to give some urine, and sometimes the doctor will take a smear from the inside of your penis. - While this test won't be very pleasant, it usually doesn't hurt.
 Prepare for blood tests. Your doctor will likely want you to have blood drawn and tested for C-reactive protein or BSE (sedimentation) to find out which abnormalities are causing this infection. He / she can also identify certain strains of bacteria in your blood with a blood test.
Prepare for blood tests. Your doctor will likely want you to have blood drawn and tested for C-reactive protein or BSE (sedimentation) to find out which abnormalities are causing this infection. He / she can also identify certain strains of bacteria in your blood with a blood test. 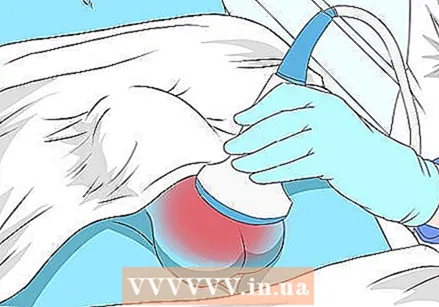 Ask for an ultrasound. With an ultrasound, the doctor can determine whether you have epididymitis or a twisted testicle. This distinction can sometimes be difficult to make in younger men, but an ultrasound can provide more clarity.
Ask for an ultrasound. With an ultrasound, the doctor can determine whether you have epididymitis or a twisted testicle. This distinction can sometimes be difficult to make in younger men, but an ultrasound can provide more clarity. - The doctor uses a kind of handle over your groin to make an ultrasound. If blood flow to the area is limited, it could indicate a twisted testicle. If the blood flow is very high, this can indicate epididymitis.
Part 4 of 4: Treating the disease
 Expect antibiotics to be prescribed. The treatment for epididymitis depends on the cause. Usually the condition is caused by an infection, for which the doctor will prescribe antibiotics. The type of antibiotics depend on whether the infection was caused by an STI or not. If you have epididymitis caused by an STI, your partner may also need to take antibiotics.
Expect antibiotics to be prescribed. The treatment for epididymitis depends on the cause. Usually the condition is caused by an infection, for which the doctor will prescribe antibiotics. The type of antibiotics depend on whether the infection was caused by an STI or not. If you have epididymitis caused by an STI, your partner may also need to take antibiotics. - For gonorrhea and chlamydia, the doctor will usually prescribe a single dose of ceftriaxone given as an injection, followed by a 10-day course of 100 mg doxycycline twice a day.
- In some cases, the doxycycline is replaced with 500 mg levofloxacin or 300 mg ofloxacin once daily for ten days.
- If you were infected with an STI, you should refrain from sexual intercourse until you and your partner have completed the entire course of antibiotics.
- If the infection wasn't caused by an STI, you'll likely get levofloxacin or ofloxacin, without ceftriaxone.
 Take anti-inflammatory pain relievers such as ibuprofen. These agents can reduce pain and inflammation. They are easy to obtain, and you probably already have them in the closet, and they are relatively effective. However, never take painkillers for more than 10 consecutive days; see your doctor if you are still in pain after 10 days.
Take anti-inflammatory pain relievers such as ibuprofen. These agents can reduce pain and inflammation. They are easy to obtain, and you probably already have them in the closet, and they are relatively effective. However, never take painkillers for more than 10 consecutive days; see your doctor if you are still in pain after 10 days. - You can take 200 mg of ibuprofen every 4-6 hours for pain and inflammation. You can increase the dose to 400 mg if needed.
 Lie down and raise your hips slightly. It may be wise to rest in bed for a few days to ease some of the pain associated with the condition. Raise your hips to reduce symptoms.
Lie down and raise your hips slightly. It may be wise to rest in bed for a few days to ease some of the pain associated with the condition. Raise your hips to reduce symptoms. - When lying down or sitting, place a towel or a rolled up T-shirt under your crotch to ease the discomfort.
 Apply a cold compress to the sore spot. Putting a cold compress on your scrotum can reduce inflammation by restricting blood flow. Wrap an ice pack in a towel and place it on your scrotum. Don't leave it on for more than 30 minutes or you could damage your skin.
Apply a cold compress to the sore spot. Putting a cold compress on your scrotum can reduce inflammation by restricting blood flow. Wrap an ice pack in a towel and place it on your scrotum. Don't leave it on for more than 30 minutes or you could damage your skin. - Never put ice directly on the skin. Then you damage your skin, especially in such a sensitive place.
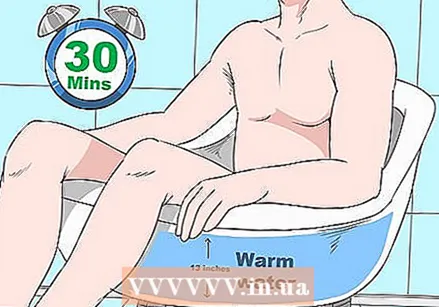 Take a sitz bath to relieve the pain. Fill a tub or bath with about 12 inches of warm water and sit in it for 30 minutes. The warm water stimulates blood flow, which helps the body to fight the infection better. Do this as often as necessary.
Take a sitz bath to relieve the pain. Fill a tub or bath with about 12 inches of warm water and sit in it for 30 minutes. The warm water stimulates blood flow, which helps the body to fight the infection better. Do this as often as necessary. - This treatment is especially effective in chronic epididymitis.
Tips
- Get good support. A tok can provide support in the crotch, so that the pain is less. Boxer shorts are usually less supportive than regular briefs.
Warnings
- Not for quite a while. Avoid intercourse while you are experiencing symptoms. When you have sex, there is more pressure on the area, which can cause pain. In addition, you are still contagious for at least a week after you start treatment if you have an STI.