Author:
Gregory Harris
Date Of Creation:
10 August 2021
Update Date:
1 July 2024

Content
- Steps
- Part 1 of 4: Be Confident in Your Sexual Partner
- Part 2 of 4: Protected Sex
- Part 3 of 4: Preventive Treatment
- Part 4 of 4: Get tested regularly
- Warnings
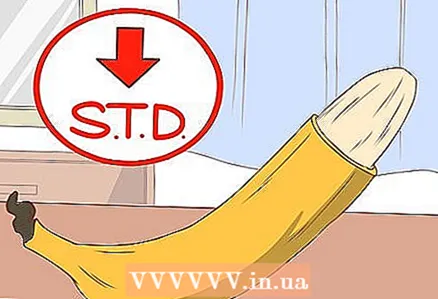
STIs are sexually transmitted infections (also known as STDs (Sexually Transmitted Diseases)). These infections are spread from person to person through various body fluids, including those exchanged between partners during sexual intercourse. Common sexually transmitted infections are herpes, chlamydia, gonorrhea, hepatitis, and human immunodeficiency virus (HIV). These are very unpleasant diseases that can negatively affect human health, and some of these diseases can be fatal. But there are several ways to reduce your risk of contracting an STI.
Steps
Part 1 of 4: Be Confident in Your Sexual Partner
 1 Consider abstinence. The surest way to protect yourself from STIs is not to have sexual intercourse. This applies to vaginal, oral and anal sex.
1 Consider abstinence. The surest way to protect yourself from STIs is not to have sexual intercourse. This applies to vaginal, oral and anal sex. - Abstinence is a great choice for some people, but for most it remains unrealistic and undesirable. If abstinence is not for you, there are other ways to reduce your risk of contracting these infections.
- Remember that abstaining from sexual intercourse alone is usually less effective than just proper sexual behavior. If you are planning to abstain from sexual intercourse for a while, it is important to learn more information about safer sex to help you choose the one that suits you best.
 2 Think about monogamy. The most reliable form of sexual contact is sexual contact with only one partner, if this partner also prefers monogamy. Before having sex with your partner, you both need to get tested for any sexually transmitted infections. If neither of you has these infections, if you both prefer monogamy, your risk of contracting an STI is very low.
2 Think about monogamy. The most reliable form of sexual contact is sexual contact with only one partner, if this partner also prefers monogamy. Before having sex with your partner, you both need to get tested for any sexually transmitted infections. If neither of you has these infections, if you both prefer monogamy, your risk of contracting an STI is very low. 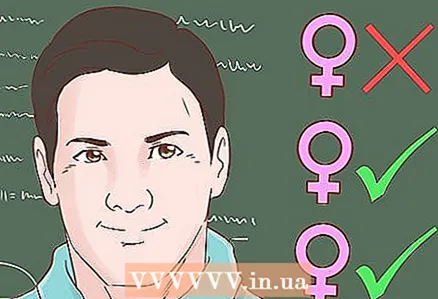 3 Consider reducing the number of sex partners. The fewer sex partners you have, the lower your risk of contracting sexually transmitted infections. You should also ask how many sex partners each of those you sleep with had. The fewer sexual partners they have, the lower the risk of contracting an STI.
3 Consider reducing the number of sex partners. The fewer sex partners you have, the lower your risk of contracting sexually transmitted infections. You should also ask how many sex partners each of those you sleep with had. The fewer sexual partners they have, the lower the risk of contracting an STI.  4 Sleep only with trusted partners. Before you sleep with a person, you need to make sure that he was tested and that he has not been diagnosed with an STI. Most STIs can be detected with tests, and most of these infections can be cured. If your partner tests positive for an STI, refrain from sexual intercourse with him until the end of his treatment. You can be intimate with your partner again as soon as your doctor tells you to.
4 Sleep only with trusted partners. Before you sleep with a person, you need to make sure that he was tested and that he has not been diagnosed with an STI. Most STIs can be detected with tests, and most of these infections can be cured. If your partner tests positive for an STI, refrain from sexual intercourse with him until the end of his treatment. You can be intimate with your partner again as soon as your doctor tells you to. - If your partner claims to have been tested for STIs, ask to identify which diseases.Often people are only tested for gonorrhea and chlamydia, but not tested for HIV, hepatitis, and herpes.
- Keep in mind that the human papilloma virus is not detected in men.
 5 Inquire about your partner's sexual health. Communication is the key to protecting yourself from STIs. Be open about your past and your sexual health, and make sure your partner listens to you respectfully. Refuse sexual contact with a person who does not want to share information about their sex life with you, who reacts aggressively to such conversations: safe sex requires the consent of both partners.
5 Inquire about your partner's sexual health. Communication is the key to protecting yourself from STIs. Be open about your past and your sexual health, and make sure your partner listens to you respectfully. Refuse sexual contact with a person who does not want to share information about their sex life with you, who reacts aggressively to such conversations: safe sex requires the consent of both partners.  6 Be careful during sexual intercourse. Alcoholic drinks dull attention. This can negatively affect your decision-making ability: for example, after drinking alcohol, you may decide to give up contraception, which you would not do when sober. Alcohol and drugs also interfere with the correct use of condoms, so there is a risk that you simply will not be able to put them on correctly. Make sure you are sober enough to make the right decisions during sex.
6 Be careful during sexual intercourse. Alcoholic drinks dull attention. This can negatively affect your decision-making ability: for example, after drinking alcohol, you may decide to give up contraception, which you would not do when sober. Alcohol and drugs also interfere with the correct use of condoms, so there is a risk that you simply will not be able to put them on correctly. Make sure you are sober enough to make the right decisions during sex.  7 Give up drugs. Drugs, like alcohol, negatively affect your vigilance, they can provoke you to make the wrong decisions, and also make it difficult to use a condom. In addition, it is important to know that STIs can also be spread through injections, because during the injection there is an exchange between body fluids.
7 Give up drugs. Drugs, like alcohol, negatively affect your vigilance, they can provoke you to make the wrong decisions, and also make it difficult to use a condom. In addition, it is important to know that STIs can also be spread through injections, because during the injection there is an exchange between body fluids. - It is known that AIDS and hepatitis can be spread through a needle - that is, by injection.
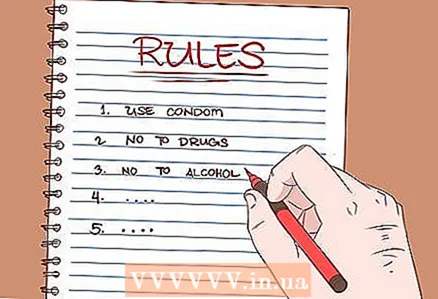 8 Follow safe sex practices with your partner. Before having sexual intercourse, make sure that you and your partner agree on the rules for safe sex. If you decide to have sex only with a condom, explain this to your partner. Support each other in your desires to make your sexual relationship more comfortable and healthy.
8 Follow safe sex practices with your partner. Before having sexual intercourse, make sure that you and your partner agree on the rules for safe sex. If you decide to have sex only with a condom, explain this to your partner. Support each other in your desires to make your sexual relationship more comfortable and healthy.  9 Do not have sexual contact with someone who is showing STI symptoms. Some STIs, such as genital herpes, have severe symptoms. If your potential sex partner has open sores, rashes, or other injuries, the person may have an STI that could be passed on to you. If you notice anything suspicious, postpone sexual intercourse with this person until they are examined by a doctor.
9 Do not have sexual contact with someone who is showing STI symptoms. Some STIs, such as genital herpes, have severe symptoms. If your potential sex partner has open sores, rashes, or other injuries, the person may have an STI that could be passed on to you. If you notice anything suspicious, postpone sexual intercourse with this person until they are examined by a doctor.
Part 2 of 4: Protected Sex
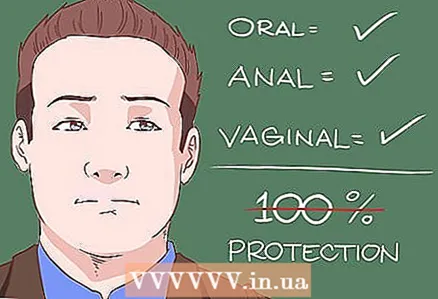 1 Keep in mind that you can get STIs through all forms of sex. Oral, anal and vaginal sex are all ways STIs can spread. Through oral sex using a condom, the risk of infection is quite low, but still there is no 100% "safe" sex. However, you can protect yourself by reducing your risk of contracting an STI.
1 Keep in mind that you can get STIs through all forms of sex. Oral, anal and vaginal sex are all ways STIs can spread. Through oral sex using a condom, the risk of infection is quite low, but still there is no 100% "safe" sex. However, you can protect yourself by reducing your risk of contracting an STI.  2 Recognize that forms of protection against STIs are not completely reliable prevention methods. Male and female condoms and rubber dams significantly reduce the risk of contracting an STI, but there is still a risk of transmitting an STI. Talk to your doctor if you have questions about the effectiveness of safer sex products.
2 Recognize that forms of protection against STIs are not completely reliable prevention methods. Male and female condoms and rubber dams significantly reduce the risk of contracting an STI, but there is still a risk of transmitting an STI. Talk to your doctor if you have questions about the effectiveness of safer sex products. 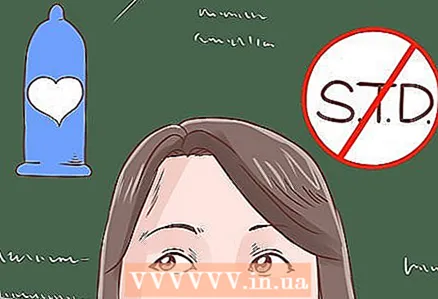 3 Understand that there is a difference between birth control and STI protection. Some of the methods that prevent you from getting an STI also prevent you from getting an unintended pregnancy (for example, male condoms), but there are many other methods of contraception that do not prevent you from getting an STI. Remember that any non-barrier method of contraception (for example, oral contraceptives, intrauterine hormonal systems, spermicides) does not protect you from contracting STIs!
3 Understand that there is a difference between birth control and STI protection. Some of the methods that prevent you from getting an STI also prevent you from getting an unintended pregnancy (for example, male condoms), but there are many other methods of contraception that do not prevent you from getting an STI. Remember that any non-barrier method of contraception (for example, oral contraceptives, intrauterine hormonal systems, spermicides) does not protect you from contracting STIs!  4 Look for latex condoms that say "disease protection" on the packaging. Most condoms are made from latex and are effective in preventing STIs, but there are some condoms (often labeled "natural" on the packaging) that are made from other materials. These condoms can prevent unwanted pregnancies, but they are not effective at protecting against STIs. To be sure to protect yourself from STIs, you need to use condoms that are labeled to protect against STIs.
4 Look for latex condoms that say "disease protection" on the packaging. Most condoms are made from latex and are effective in preventing STIs, but there are some condoms (often labeled "natural" on the packaging) that are made from other materials. These condoms can prevent unwanted pregnancies, but they are not effective at protecting against STIs. To be sure to protect yourself from STIs, you need to use condoms that are labeled to protect against STIs.  5 Condom use must be correct and consistent. Condoms are very effective and reliable when used correctly. They can be bought at all pharmacies, most department stores, sex shops, and are sometimes given out for free at some clinics and hospitals. Use a condom every time you have sex, because they only protect with constant use.
5 Condom use must be correct and consistent. Condoms are very effective and reliable when used correctly. They can be bought at all pharmacies, most department stores, sex shops, and are sometimes given out for free at some clinics and hospitals. Use a condom every time you have sex, because they only protect with constant use. - Male condoms are placed on the penis before sex. They are applied before vaginal, anal and oral sex. Gently open the package (not with your teeth or scissors), then take out the condom and position it with the curled edges away from the penis, then bring it to the glans of the penis and gently pull the condom down by rolling it down. Inspect the condom for holes or cracks, and if you feel the condom is damaged, remove it immediately. You can use a lubricant to prevent friction damage to the condom. After intercourse is complete, remove the condom before you lose your erection and discard it carefully. Never reuse a condom!
- Female condoms will also work. Female condoms are used by women before sex and must be immersed in the vagina just below the cervix. Inserting the female condom is somewhat similar to inserting a tampon. They are more difficult to find, but can usually be obtained from clinics and hospitals. Female condoms are made from latex or polyurethane material. Female condoms are especially useful for women who want to take control of their own ability to prevent unwanted pregnancies and STIs. Polyurethane female condoms can be used by women who are allergic to latex as well as women who prefer an oil-based lubricant.
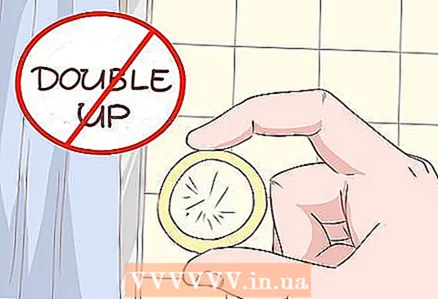 6 Use only one condom at a time. Never wear two condoms at once. In other words, men should not wear multiple condoms before intercourse, and they should not mix the use of male and female condoms at the same time. The use of several condoms at once greatly increases the risk of damage to the condom and the occurrence of various breaks and cracks, which makes using multiple condoms less effective than using one correctly.
6 Use only one condom at a time. Never wear two condoms at once. In other words, men should not wear multiple condoms before intercourse, and they should not mix the use of male and female condoms at the same time. The use of several condoms at once greatly increases the risk of damage to the condom and the occurrence of various breaks and cracks, which makes using multiple condoms less effective than using one correctly. 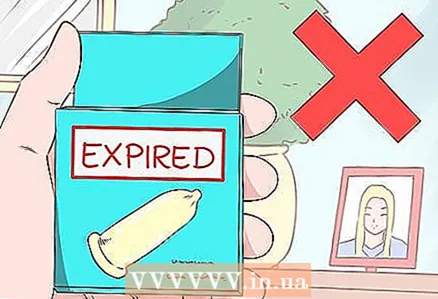 7 Make sure the condom has not expired. Check the expiration date of the condoms on the packaging. Use only condoms that have not expired, otherwise there is a high risk that the condom will simply break during sex.
7 Make sure the condom has not expired. Check the expiration date of the condoms on the packaging. Use only condoms that have not expired, otherwise there is a high risk that the condom will simply break during sex.  8 Do not store condoms in a hot or sunny place. The risk of a condom breaking is much lower when stored in a cool, dry place (such as a closet). If condoms are stored in a hot or sunny place, such as in a car or in a wallet, they need to be moved urgently to minimize the risk of the condom breaking during use.
8 Do not store condoms in a hot or sunny place. The risk of a condom breaking is much lower when stored in a cool, dry place (such as a closet). If condoms are stored in a hot or sunny place, such as in a car or in a wallet, they need to be moved urgently to minimize the risk of the condom breaking during use.  9 Try using a rubber dam. A rubber dam is a latex sheet that is used to prevent getting an STI (such as herpes) during oral sex (used for the vulva, penis, and anus). This will help protect vulnerable tissues in the mouth from infection. Cofferdams are available from the same place as condoms. As a last resort, you can use a plastic wrap or an opened condom.
9 Try using a rubber dam. A rubber dam is a latex sheet that is used to prevent getting an STI (such as herpes) during oral sex (used for the vulva, penis, and anus). This will help protect vulnerable tissues in the mouth from infection. Cofferdams are available from the same place as condoms. As a last resort, you can use a plastic wrap or an opened condom.  10 Use medical gloves. Medical gloves can be used to manually stimulate the erogenous zones. This will protect you and your partner, especially if you have any cuts or injuries on your hands that you are not aware of, because cuts can also catch an STI. In addition, the gloves can be used as a makeshift rubber dam.
10 Use medical gloves. Medical gloves can be used to manually stimulate the erogenous zones. This will protect you and your partner, especially if you have any cuts or injuries on your hands that you are not aware of, because cuts can also catch an STI. In addition, the gloves can be used as a makeshift rubber dam.  11 It is worth protecting yourself when using any intimate devices and sex toys that are used not only by you (for example, dildos or anal balls). These sex toys must be washed and disinfected after every use. You can put a condom on the dildo and vibrator. Use a new condom every time, especially with a new partner. Most sex toys come with instructions on how to clean and disinfect these toys after use.
11 It is worth protecting yourself when using any intimate devices and sex toys that are used not only by you (for example, dildos or anal balls). These sex toys must be washed and disinfected after every use. You can put a condom on the dildo and vibrator. Use a new condom every time, especially with a new partner. Most sex toys come with instructions on how to clean and disinfect these toys after use.  12 Do not use oil based lubricants if using latex products. Oil-based lubricants (such as mineral oil or petroleum jelly) can damage and rupture latex condoms and rubber dams. Use only water-based lubricant. Lubricant packaging usually indicates whether it is suitable for use with latex condoms or rubber dams.
12 Do not use oil based lubricants if using latex products. Oil-based lubricants (such as mineral oil or petroleum jelly) can damage and rupture latex condoms and rubber dams. Use only water-based lubricant. Lubricant packaging usually indicates whether it is suitable for use with latex condoms or rubber dams. - Many condoms already have a certain amount of lubricant on them.
Part 3 of 4: Preventive Treatment
 1 Get vaccinated. Currently, vaccines have been created for some STIs. For example, you can get vaccinated against hepatitis A and B, as well as against the human papilloma virus (HPV). Talk to your doctor about the possibility of vaccinating you or your child at the recommended age to take care of your health.
1 Get vaccinated. Currently, vaccines have been created for some STIs. For example, you can get vaccinated against hepatitis A and B, as well as against the human papilloma virus (HPV). Talk to your doctor about the possibility of vaccinating you or your child at the recommended age to take care of your health. - It is recommended to be vaccinated against hepatitis A and B in infancy, and children 11–12 years old are recommended to be vaccinated against HPV. However, adults who have not been vaccinated can also talk with their doctor about getting vaccinated. The HPV vaccine should not be given to people over the age of 26.
 2 Consider circumcision. Some studies have shown that men who choose circumcision are at a lower risk of developing STIs (including HIV) relative to other men. If you are at increased risk of contracting an STI, consider using circumcision to lower your risk of infection.
2 Consider circumcision. Some studies have shown that men who choose circumcision are at a lower risk of developing STIs (including HIV) relative to other men. If you are at increased risk of contracting an STI, consider using circumcision to lower your risk of infection.  3 Take Truvada if you are at high risk of contracting HIV. Truvada is a new drug that reduces the likelihood of exposure to HIV. If you are in a high-risk group, talk to your doctor about taking Truvada. For example, if you have an HIV positive partner, if you work in the sex industry, Truvada will help protect your health.
3 Take Truvada if you are at high risk of contracting HIV. Truvada is a new drug that reduces the likelihood of exposure to HIV. If you are in a high-risk group, talk to your doctor about taking Truvada. For example, if you have an HIV positive partner, if you work in the sex industry, Truvada will help protect your health. - Keep in mind that Truvada alone cannot prevent HIV infection. You must use a condom when having sex with your HIV-positive partner, even if you are taking Truvada.
 4 Don't douch. Douching (or using chemicals and soap to flush out the vaginal lining) removes beneficial bacteria from the lining that help prevent STIs from spreading. Bacteria living on mucous membranes are a protective factor against the spread of STIs, therefore it is necessary to maintain a beneficial microflora of the vagina to maintain health.
4 Don't douch. Douching (or using chemicals and soap to flush out the vaginal lining) removes beneficial bacteria from the lining that help prevent STIs from spreading. Bacteria living on mucous membranes are a protective factor against the spread of STIs, therefore it is necessary to maintain a beneficial microflora of the vagina to maintain health.
Part 4 of 4: Get tested regularly
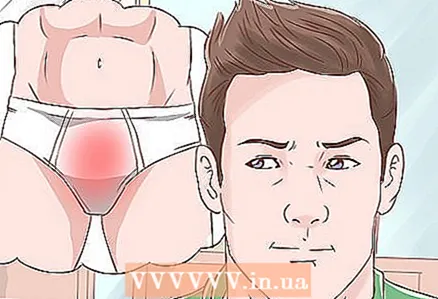 1 Recognize the most common symptoms of STIs. Not all STDs are symptomatic. However, there are some signs that you or your partner may notice and you should see your doctor right away. The most common symptoms include the following:
1 Recognize the most common symptoms of STIs. Not all STDs are symptomatic. However, there are some signs that you or your partner may notice and you should see your doctor right away. The most common symptoms include the following: - sores and rashes around the vaginal area, penis, or anus;
- pain when urinating;
- pain during sex;
- unusual discharge with a strange foul odor from the vagina or glans;
- unusual vaginal bleeding.
 2 Understand the fact that many STDs are curable. Do not neglect visiting your doctor if you are worried about STIs.Many STIs are curable and can be completely eliminated from the body if the correct treatment is followed. Be honest and open with your doctor and adhere to treatment recommendations.
2 Understand the fact that many STDs are curable. Do not neglect visiting your doctor if you are worried about STIs.Many STIs are curable and can be completely eliminated from the body if the correct treatment is followed. Be honest and open with your doctor and adhere to treatment recommendations.  3 Determine if you are at risk. Everyone should get tested regularly, but there are several demographic groups that should be tested more often than others. This category of people includes:
3 Determine if you are at risk. Everyone should get tested regularly, but there are several demographic groups that should be tested more often than others. This category of people includes: - Pregnant women or women trying to get pregnant.
- People with HIV-positive status - they are more prone to contracting STIs.
- People who regularly sleep with HIV-positive partners.
- Homosexual men.
- Women under 25 who are sexually active - they are advised to be tested more often for chlamydia.
- Women over 21 - they should get tested more often for HIV.
- People born in 1945-1965 - they have an increased risk of hepatitis C.
- People who have many sexual partners, who have only one sexual partner but sleeps with several partners, if you provide intimate services, if you take certain drugs, have unprotected sex, if you have had an STD before, or someone from your parents had an STD, if you were born while your mother had an STD, you have an increased risk of contracting an STD.
 4 Get tested regularly. You need to be checked every 3-6 months, especially if you are in a high-risk group. In fact, everyone who is sexually active is at risk. Therefore, even if you are in a monogamous relationship, it is a good idea to get tested for STIs every few years. To protect yourself and prevent further spread of infection, it is necessary to reduce the risk of contracting STIs in the population. In other words, you are protecting others by taking care of your health. Tests can be taken in a doctor's office, in a private clinic or in a laboratory, for example, in "Invitro".
4 Get tested regularly. You need to be checked every 3-6 months, especially if you are in a high-risk group. In fact, everyone who is sexually active is at risk. Therefore, even if you are in a monogamous relationship, it is a good idea to get tested for STIs every few years. To protect yourself and prevent further spread of infection, it is necessary to reduce the risk of contracting STIs in the population. In other words, you are protecting others by taking care of your health. Tests can be taken in a doctor's office, in a private clinic or in a laboratory, for example, in "Invitro". - Regular testing is essential if you have multiple sex partners.
- Today it is possible to identify HIV, syphilis, herpes, trichomoniasis, chlamydia, gonorrhea, hepatitis B.
 5 Collect blood, urine, or other body fluid samples. The doctor usually determines the status after the examination, examination and delivery of blood and urine tests. If you have any genital lesions that ooze fluid, you can also take it for analysis.
5 Collect blood, urine, or other body fluid samples. The doctor usually determines the status after the examination, examination and delivery of blood and urine tests. If you have any genital lesions that ooze fluid, you can also take it for analysis.  6 Have your partner get tested too. Encourage him to take the STI test with you. Reassure him that this is the best solution for both of you to keep you healthy. This does not mean that you do not trust your partner or are insincere yourself. It's just the smartest decision.
6 Have your partner get tested too. Encourage him to take the STI test with you. Reassure him that this is the best solution for both of you to keep you healthy. This does not mean that you do not trust your partner or are insincere yourself. It's just the smartest decision.  7 If you want, you can use the free services. If you can't afford expensive tests or don't have health insurance, look for a free STI screening test, especially if you are at risk of contracting these infections. There are many organizations that provide free screening of patients, for example, these organizations include:
7 If you want, you can use the free services. If you can't afford expensive tests or don't have health insurance, look for a free STI screening test, especially if you are at risk of contracting these infections. There are many organizations that provide free screening of patients, for example, these organizations include: - health department;
- family planning center;
- school or clinic at a higher educational institution;
- city polyclinics;
- Internet resources;
- city clinical hospitals.
 8 Do not be shy. There is no shame in getting tested for STIs. You have made a smart decision that will protect your health and the health of those around you. If each of us regularly undergoes tests and examinations, STDs will become much less common. You should be proud to take part in protecting the health of your people.
8 Do not be shy. There is no shame in getting tested for STIs. You have made a smart decision that will protect your health and the health of those around you. If each of us regularly undergoes tests and examinations, STDs will become much less common. You should be proud to take part in protecting the health of your people.  9 Understand the fact that not all STDs can be diagnosed with testing. For example, in men, HPV is not diagnosed. Therefore, even if your doctor gave you a negative test result, it is still recommended to use condoms during sex.
9 Understand the fact that not all STDs can be diagnosed with testing. For example, in men, HPV is not diagnosed. Therefore, even if your doctor gave you a negative test result, it is still recommended to use condoms during sex.  10 Follow your doctor's recommendations. If the doctor said that it is still dangerous for you to have sex, try to still listen to his words. For example, people with genital herpes should not have sex during a flare-up. Only have sexual intercourse when your doctor has confirmed that it is safe for your health.
10 Follow your doctor's recommendations. If the doctor said that it is still dangerous for you to have sex, try to still listen to his words. For example, people with genital herpes should not have sex during a flare-up. Only have sexual intercourse when your doctor has confirmed that it is safe for your health. - Don't have sexual intercourse until you and your partner are completely healed of any STDs.
 11 Tell your sexual partner (s) about your diagnosis. If the test tests positive for an STI, tell your sex partner (and ex-partner) so they can get tested too. If you do not want to discuss this topic in person, you can send your partner an anonymous letter - this is necessary to notify the person that he may be infected with an STI.
11 Tell your sexual partner (s) about your diagnosis. If the test tests positive for an STI, tell your sex partner (and ex-partner) so they can get tested too. If you do not want to discuss this topic in person, you can send your partner an anonymous letter - this is necessary to notify the person that he may be infected with an STI.
Warnings
- It is very difficult to prevent HIV infection even with the use of barrier methods of protection. Get vaccinated if you are susceptible to getting HIV.
- Even if you always use protective equipment and contraception correctly, there is still a (albeit small) risk of contracting an STI.
- Non-barrier contraceptives (such as hormonal contraceptives or intrauterine devices) do not protect against STIs. If you are at risk for STDs and unwanted pregnancies, use condoms or other methods of protection (besides normal contraceptives).
- Some people are allergic to latex. Therefore, before using latex condoms, it is necessary to make an allergic test for the presence of an allergic reaction to this material, especially if you have not used latex condoms before. If you or your partner is allergic to latex, it is worth considering other methods of protection, such as female condoms. In addition, today there are protective equipment made from other materials. In the event that you have not found such remedies, it is worth postponing sexual contacts until you find an alternative solution - remember that this is fraught with STI infection.
- Remember that not all STDs are symptomatic. You and your sexual partner may not even be aware of an STD infection. Talk to your doctor if you suspect you may have contracted an STI (even if you are feeling well).