Author:
Marcus Baldwin
Date Of Creation:
14 June 2021
Update Date:
24 June 2024

Content
- Steps
- Part 1 of 3: Identifying Vaginismus
- Part 2 of 3: Understanding the Causes of Vaginismus
- Part 3 of 3: Treating Vaginismus
- Tips
Vaginismus is a type of female sexual dysfunction in which the muscles in the vagina contract involuntarily, usually during attempted intercourse, causing discomfort or pain. Vaginismus not only interferes with a normal sex life, but also prevents women from inserting tampons or undergoing gynecological examinations. The causes of vaginismus can be different and need to be identified for treatment. While this condition can be frustrating, awkward, and tense, it is completely treatable.
Steps
Part 1 of 3: Identifying Vaginismus
 1 Take painful sex seriously. The first and most disturbing symptom of vaginismus is pain during attempted intercourse. Feelings may differ from woman to woman - it can be a burning sensation, tingling sensation, tension, tearing, or as if the partner is "hitting an obstacle." Often, the pain and involuntary muscle contractions are so severe that you have to stop intercourse.
1 Take painful sex seriously. The first and most disturbing symptom of vaginismus is pain during attempted intercourse. Feelings may differ from woman to woman - it can be a burning sensation, tingling sensation, tension, tearing, or as if the partner is "hitting an obstacle." Often, the pain and involuntary muscle contractions are so severe that you have to stop intercourse. - Many women find this problem the first time they try to have sex. This is called primary vaginismus.
- Other women develop vaginismus during their lifetime - this is called secondary vaginismus.Therefore, you should not ignore this important symptom just because you have had a pain-free sexual relationship in the past.
 2 Look for other vaginal penetration problems. In addition to pain during intercourse, women with vaginismus may have problems with other types of penetration, including tampon insertion and gynecological examinations. Other signs also include:
2 Look for other vaginal penetration problems. In addition to pain during intercourse, women with vaginismus may have problems with other types of penetration, including tampon insertion and gynecological examinations. Other signs also include: - non-consumable marriage;
- persistent sexual discomfort after childbirth, candidiasis, urinary tract infections, STDs, interstitial cystitis, hysterectomy, cancer and surgery, rape or menopause;
- pain during intercourse of unknown origin;
- stopping breathing during an attempt to perform intercourse;
 3 Look for other muscle cramps.Vaginal muscle contractions and spasms are a hallmark of vaginismus, but some women also experience cramps in the legs or lower back. These spasms occur most often during attempted intercourse.
3 Look for other muscle cramps.Vaginal muscle contractions and spasms are a hallmark of vaginismus, but some women also experience cramps in the legs or lower back. These spasms occur most often during attempted intercourse.  4 Consider if you are avoiding sex. Many women with vaginismus avoid situations that can lead to sex. If you are avoiding sexual activity or romance because you are afraid of pain and uncomfortable with your symptoms, then it is worth seeking medical attention.
4 Consider if you are avoiding sex. Many women with vaginismus avoid situations that can lead to sex. If you are avoiding sexual activity or romance because you are afraid of pain and uncomfortable with your symptoms, then it is worth seeking medical attention. - Remember that you are avoiding sex through no fault of your own, but because your body involuntarily associates sex with pain.
 5 See your doctor. Make an appointment with your doctor or gynecologist to discuss vaginismus. Be clear about the extent and severity of your symptoms.
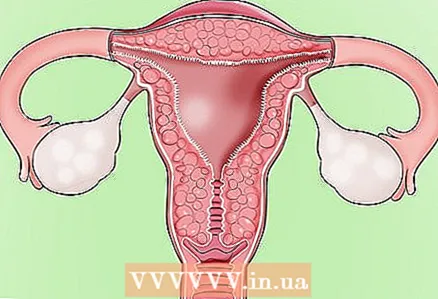
5 See your doctor. Make an appointment with your doctor or gynecologist to discuss vaginismus. Be clear about the extent and severity of your symptoms.  6 Eliminate other possible violations. Your doctor should perform a pelvic exam and pay attention to any discomfort or vaginal contractions that may occur. In addition, he or she will likely recommend additional tests to rule out other possible causes of your symptoms.
6 Eliminate other possible violations. Your doctor should perform a pelvic exam and pay attention to any discomfort or vaginal contractions that may occur. In addition, he or she will likely recommend additional tests to rule out other possible causes of your symptoms. - Vaginismus can be caused by obvious physical causes, such as infections, trauma, or oversensitive nerves in the vaginal area (provoked vulvodynia).
 7 It is imperative that the correct diagnosis be made. If all other possible causes of your symptoms have been ruled out, your doctor may diagnose you with either primary vaginismus or secondary vaginismus. In addition, the clinician may describe the disorder as general if symptoms appear in all administration situations, or as situational if symptoms appear only in certain situations (for example, during attempted sex).
7 It is imperative that the correct diagnosis be made. If all other possible causes of your symptoms have been ruled out, your doctor may diagnose you with either primary vaginismus or secondary vaginismus. In addition, the clinician may describe the disorder as general if symptoms appear in all administration situations, or as situational if symptoms appear only in certain situations (for example, during attempted sex). - Unfortunately, female sexuality and sexual dysfunction are not fully understood. You may run into nursing staff who will ignore your symptoms or be unable to help you. In this case, you may need to be persistent to get diagnosed and treated. If your doctor does not help you, see another doctor, preferably one with experience in treating vaginismus and other forms of female sexual dysfunction.
- Other possible diagnoses include apareunia, a general term for an inability to have intercourse (in particular, vaginismus is one of the types) and dyspareunia, pain during intercourse.
- These diagnoses will help propel treatment forward by making it possible to see the right specialists.
Part 2 of 3: Understanding the Causes of Vaginismus
 1 Be aware that anxiety is often associated with vaginismus. Many women with vaginismus may notice that their symptoms are associated with stress, anxiety, and fear. These causes may have deep roots, or they may simply be related to your current standard of living, such as lack of sleep and the stress associated with overworking at work.
1 Be aware that anxiety is often associated with vaginismus. Many women with vaginismus may notice that their symptoms are associated with stress, anxiety, and fear. These causes may have deep roots, or they may simply be related to your current standard of living, such as lack of sleep and the stress associated with overworking at work.  2 Identify underlying beliefs about sex and sexuality. Women with vaginismus are more likely to think negatively about sex and sexuality.These feelings may be rooted in childhood, or they may be associated with a traumatic event.
2 Identify underlying beliefs about sex and sexuality. Women with vaginismus are more likely to think negatively about sex and sexuality.These feelings may be rooted in childhood, or they may be associated with a traumatic event. - If latent negative beliefs about sex come from early childhood, then another potential component of vaginismus may be lack of proper sex education.
 3 Become aware of the role of past experiences. It was found that women with vaginismus were twice as likely to experience a traumatic sexual event in childhood. These could be injuries of varying severity, which include:
3 Become aware of the role of past experiences. It was found that women with vaginismus were twice as likely to experience a traumatic sexual event in childhood. These could be injuries of varying severity, which include: - sexual harassment by a friend;
- sexual abuse;
- pelvic injury;
- violence in family;
- extremely negative early sexual experience with a consensual partner.
 4 Be aware that relationship difficulties may have contributed. If you have secondary and situational vaginismus, then problems with a sexual or romantic partner may be the cause. These problems can include: lack of trust, fear of commitment, fear of becoming too vulnerable or open to pain and frustration.
4 Be aware that relationship difficulties may have contributed. If you have secondary and situational vaginismus, then problems with a sexual or romantic partner may be the cause. These problems can include: lack of trust, fear of commitment, fear of becoming too vulnerable or open to pain and frustration. 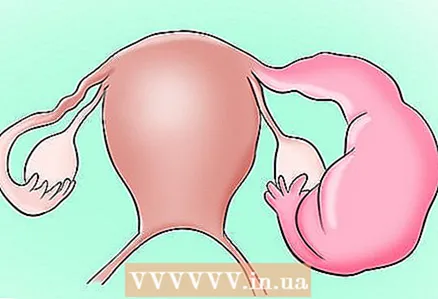 5 Understand that medical disorders can play a role. A variety of disorders can provoke or worsen the symptoms of vaginismus. This is more likely if vaginismus appears after a period of normal sexual functioning. Potential medical conditions that can contribute to vaginismus:
5 Understand that medical disorders can play a role. A variety of disorders can provoke or worsen the symptoms of vaginismus. This is more likely if vaginismus appears after a period of normal sexual functioning. Potential medical conditions that can contribute to vaginismus: - urinary tract infections and other urinary problems;
- sexually transmitted infections;
- cancer of the genital or reproductive organs;
- endometriosis;
- inflammatory diseases of the pelvic organs;
- vulvodynia or vestibulodynia.
- Medical procedures involving the female reproductive organs, such as removing the uterus, can also lead to vaginismus.
 6 Be aware of the potential role of the reproductive periods. For many women, the onset of secondary vaginismus is associated with childbirth. This is especially true if the childbirth was difficult or if genital injuries appeared as a result of childbirth. In some women, vaginismus has developed due to hormonal changes and vaginal dryness, usually occurring during menopause.
6 Be aware of the potential role of the reproductive periods. For many women, the onset of secondary vaginismus is associated with childbirth. This is especially true if the childbirth was difficult or if genital injuries appeared as a result of childbirth. In some women, vaginismus has developed due to hormonal changes and vaginal dryness, usually occurring during menopause. - Secondary vaginismus can also occur as a result of fear of having children or having to go through labor.
 7 Accept the possibility that there are no apparent reasons. Some women will never know why they got vaginismus. They do not have any visible or hidden causes of vaginismus.
7 Accept the possibility that there are no apparent reasons. Some women will never know why they got vaginismus. They do not have any visible or hidden causes of vaginismus. - Some studies even suggest that the symptoms of vaginismus are part of general defense mechanisms that are triggered in threatening situations. This suggests that it does not always need to be viewed as primarily sexual dysfunction.
Part 3 of 3: Treating Vaginismus
 1 Try counseling. Whether your vaginismus is due to emotional or psychological problems, a therapist can help you. This is because awareness of the condition itself often generates fear and anxiety before intercourse, forming a vicious circle that only aggravates the symptoms. Depression, feelings of isolation and low self-esteem are also common signs of sexual dysfunction.
1 Try counseling. Whether your vaginismus is due to emotional or psychological problems, a therapist can help you. This is because awareness of the condition itself often generates fear and anxiety before intercourse, forming a vicious circle that only aggravates the symptoms. Depression, feelings of isolation and low self-esteem are also common signs of sexual dysfunction. - Treatment outcomes are much more positive when the woman and her sexual partner are motivated, act in concert and determined to reduce relationship conflicts. Thus, a psychological assessment of the couple is an excellent starting point for treatment.
- If vaginismus is associated with an anxiety disorder or sexual trauma in the past, a therapist can help you deal with these issues so you can move on.
- One type of psychotherapy, cognitive behavioral therapy, may be especially helpful for some women.This type of psychotherapy focuses on the relationship between thoughts and behavior, and a cognitive-behavioral therapist can help change your thoughts and behaviors about avoiding sex. ...
 2 Ask about exposure therapy. One type of treatment for vaginismus is called exposure therapy, or "immersion," which involves gradually desensitizing penetration. The therapist's assistance in penetration is effective treatment, even if the woman has lived with vaginismus her entire life. Impact techniques are usually associated with vaginal penetration exercises using dilators.
2 Ask about exposure therapy. One type of treatment for vaginismus is called exposure therapy, or "immersion," which involves gradually desensitizing penetration. The therapist's assistance in penetration is effective treatment, even if the woman has lived with vaginismus her entire life. Impact techniques are usually associated with vaginal penetration exercises using dilators. - The same method is used for self-healing with the help of a consultant who would help move on without losing confidence in success.
 3 Find a physical therapist. Ask your doctor to refer you to a physical therapist who has experience with vaginismus and other forms of female sexual dysfunction. Since the pelvic floor muscles play an important role in the onset of vaginismus symptoms, physical therapy is one of the best treatments. A physical therapist can:
3 Find a physical therapist. Ask your doctor to refer you to a physical therapist who has experience with vaginismus and other forms of female sexual dysfunction. Since the pelvic floor muscles play an important role in the onset of vaginismus symptoms, physical therapy is one of the best treatments. A physical therapist can: - teach you breathing and relaxation techniques
- help you with the contraction of the pelvic floor muscles by teaching them to control
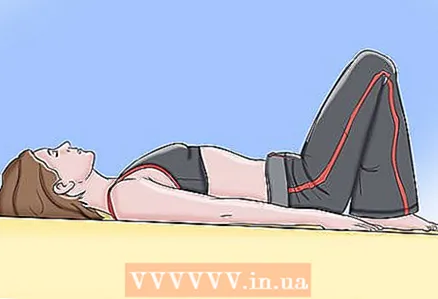 4 Do Kegel exercises. The Kegel Exercise is designed to help control your pelvic floor muscles. To do the Kegel exercise, squeeze the muscles you are using to stop the flow of urine, hold them for a few seconds, and then relax. Try to do about 20 contractions at a time, as often throughout the day as you can.
4 Do Kegel exercises. The Kegel Exercise is designed to help control your pelvic floor muscles. To do the Kegel exercise, squeeze the muscles you are using to stop the flow of urine, hold them for a few seconds, and then relax. Try to do about 20 contractions at a time, as often throughout the day as you can. - Some doctors recommend doing the Kegel exercise with a finger inserted into the vagina (up to three fingers can be used). The finger allows you to feel the contracting muscles for better control.
 5 Consider using vaginal dilators. Your doctor may recommend using vaginal dilators at home. These are tapered instruments that are placed in the vagina. They gradually enlarge, allowing the vaginal muscles to stretch and get used to penetration.
5 Consider using vaginal dilators. Your doctor may recommend using vaginal dilators at home. These are tapered instruments that are placed in the vagina. They gradually enlarge, allowing the vaginal muscles to stretch and get used to penetration. - To begin with, push as if you were having a bowel movement. It helps to enlarge the vagina. Then insert your fingers (without a dilator yet) into the vagina while continuing to push or push.
- When you start using the extenders, leave them on for 10-15 minutes. The vaginal muscles will get used to the pressure.
- If you have a spouse or partner, you can ask them to help you insert dilators.
 6 Begin sexual intercourse gradually. Women with vaginismus need to be patient and try different treatment options before having sex. If you try to immediately become sexually active, you may experience pain or discomfort, thereby attuning to pain and anxiety and exacerbating vaginismus. It is very important that your partner is supportive.
6 Begin sexual intercourse gradually. Women with vaginismus need to be patient and try different treatment options before having sex. If you try to immediately become sexually active, you may experience pain or discomfort, thereby attuning to pain and anxiety and exacerbating vaginismus. It is very important that your partner is supportive. - When you try to have sex, start very slowly, using a lot of lubricant, and experiment to find the most comfortable positions.
- Doctors generally advise women, when they stop using vaginal dilators, to hold the penetrating object by placing some or all of it in the vagina. This applies equally to penises, dildos and vibrators.
Tips
- Some women are so embarrassed and ashamed of their condition that they do not seek medical help. If you are experiencing these feelings, then remember that vaginismus is not your fault and that this disorder is treatable. Find a sympathetic therapist and a good therapist who can help you find a normal sex life.
- Some doctors and websites may recommend medications, including local anesthetics, to treat vaginismus.Overall, however, this is not a good idea: local anesthetics reduce pain, but they will not solve the problem itself, and it may be even more difficult for you to deal with the condition.