Author:
Gregory Harris
Date Of Creation:
11 August 2021
Update Date:
1 July 2024

Content
- Steps
- Method 1 of 3: Symptoms
- Method 2 of 3: At the doctor's office
- Method 3 of 3: Planning a Pregnancy
A miscarriage is the spontaneous termination of a pregnancy before the 20th week. In most cases, this happens when the woman does not yet realize that she is pregnant, so it is impossible to establish the actual number of miscarriages. According to statistics, 10 to 20 percent of pregnancies end in miscarriage. These numbers refer to women who are aware of their pregnancy. If you experience symptoms of a miscarriage, seek immediate medical attention.
Steps
Method 1 of 3: Symptoms
 1 Contact your obstetrician-gynecologist or call an ambulance if you have bleeding. It can be all sorts of discharge: blood clots, bleeding and discharge mixed with rejected tissue. Such discharge can be a symptom of a miscarriage. Depending on the intensity of the bleeding and where you are, your doctor may recommend that you call an ambulance or come to your appointment at the appointed time.
1 Contact your obstetrician-gynecologist or call an ambulance if you have bleeding. It can be all sorts of discharge: blood clots, bleeding and discharge mixed with rejected tissue. Such discharge can be a symptom of a miscarriage. Depending on the intensity of the bleeding and where you are, your doctor may recommend that you call an ambulance or come to your appointment at the appointed time. - If there is a discharge of tissue from the vagina, and you think it is fetal tissue, collect it in a clean, sealed container and take it with you to your doctor.
- It may seem strange to you, but thanks to these actions, the doctor will be able to conduct the necessary research to confirm or refute your fears.
 2 Note that the risk of miscarriage is greatly increased if spotting or bleeding from the vagina is present. Many women bleed, but this does not mean that a miscarriage has occurred. However, it is best to consult an obstetrician-gynecologist who will tell you what to do in your situation.
2 Note that the risk of miscarriage is greatly increased if spotting or bleeding from the vagina is present. Many women bleed, but this does not mean that a miscarriage has occurred. However, it is best to consult an obstetrician-gynecologist who will tell you what to do in your situation. - If you experience muscle cramps, we recommend that you see your doctor immediately.
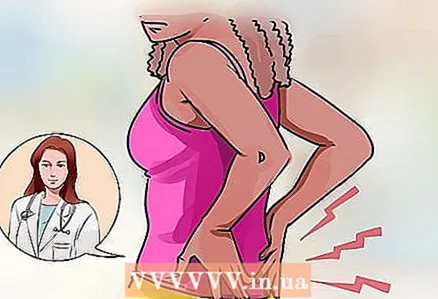 3 Pay attention to severe lower back pain. Back pain, abdominal discomfort, cramps can be symptoms of a miscarriage, even if you are not bleeding.
3 Pay attention to severe lower back pain. Back pain, abdominal discomfort, cramps can be symptoms of a miscarriage, even if you are not bleeding. - Check with your doctor before taking any pain relievers.
 4 Learn about the symptoms of a septic miscarriage. Septic miscarriage occurs when the contents of the uterus become infected. This condition is dangerous for a woman's health and requires immediate medical attention. Symptoms of a septic miscarriage include:
4 Learn about the symptoms of a septic miscarriage. Septic miscarriage occurs when the contents of the uterus become infected. This condition is dangerous for a woman's health and requires immediate medical attention. Symptoms of a septic miscarriage include: - foul-smelling vaginal discharge;
- vaginal bleeding;
- fever and chills;
- abdominal cramps and pains.
Method 2 of 3: At the doctor's office
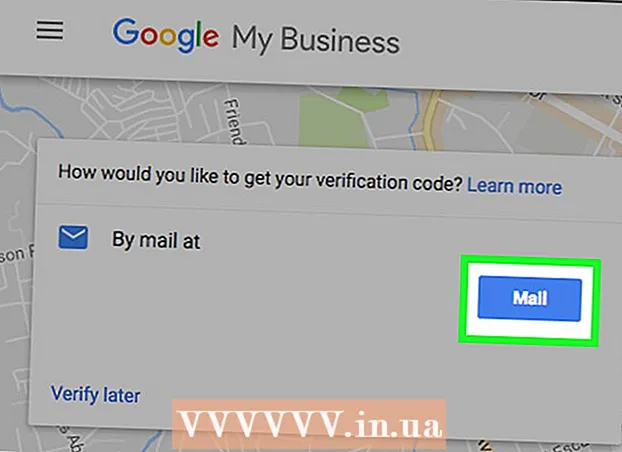
 1 Get the necessary examination with an obstetrician-gynecologist. Your doctor will do a test to help him determine if you have a miscarriage or if you are still pregnant.
1 Get the necessary examination with an obstetrician-gynecologist. Your doctor will do a test to help him determine if you have a miscarriage or if you are still pregnant. - The doctor will most likely do an ultrasound scan so that the presence of the fetus in the uterus can be seen. If you are pregnant, the ultrasound will also allow your doctor to see if the fetus is developing properly. In addition, for longer periods, the doctor can check the fetal heartbeat.
- The obstetrician-gynecologist will examine the vagina so that he can see if the cervix has opened.
- The blood test results will allow the doctor to assess your hormonal levels.
- If you have brought tissue with you in an airtight container that you believe may be fetal tissue, your doctor will do the necessary tests to confirm or refute your concerns.
 2 Find out about the possible diagnoses your doctor might give you. These include:
2 Find out about the possible diagnoses your doctor might give you. These include: - Risk of miscarriage.This diagnosis can be made if symptoms of a possible miscarriage are present. But do not worry ahead of time, because the threat of a miscarriage does not always lead directly to a miscarriage. If you are having seizures or bleeding but your cervix is closed, your doctor may diagnose you at risk of miscarriage.
- If it is impossible to prevent a miscarriage, then, unfortunately, the doctor will diagnose you with a miscarriage. The doctor will make this diagnosis if the uterus contracts and the cervix has opened. In this case, a miscarriage is inevitable.
- A complete miscarriage is characterized by the complete release of all tissues of the fetus and ovum from the uterus.
- An incomplete miscarriage occurs when the tissue has come out, but some parts of the fetus or placenta have not yet exited the vagina.
- A frozen pregnancy occurs when the fetus dies for any reason.
 3 Follow your doctor's recommendations if you have been diagnosed with threatened miscarriage. The threat of miscarriage does not always lead directly to miscarriage. However, in some situations, a miscarriage is inevitable. Often, however, your doctor may recommend the following to prevent miscarriage:
3 Follow your doctor's recommendations if you have been diagnosed with threatened miscarriage. The threat of miscarriage does not always lead directly to miscarriage. However, in some situations, a miscarriage is inevitable. Often, however, your doctor may recommend the following to prevent miscarriage: - rest until symptoms have subsided;
- do not exercise;
- refrain from intimacy;
- refuse to travel to places where you will not be able to provide fast and high-quality medical care, if necessary.
 4 If a miscarriage has occurred, but not all tissues of the ovum have come out, follow the recommendations of the obstetrician-gynecologist. However, your doctor will take your opinion into account when prescribing treatment.
4 If a miscarriage has occurred, but not all tissues of the ovum have come out, follow the recommendations of the obstetrician-gynecologist. However, your doctor will take your opinion into account when prescribing treatment. - You can wait for the remaining tissue to be torn away. In this case, it will take about one month.
- You may be taking medications that will reject any remaining tissue. This usually happens during the day. The drugs can be taken orally or used as suppositories inserted into the vagina.
- If you show signs of infection, the doctor will remove the remaining tissue.
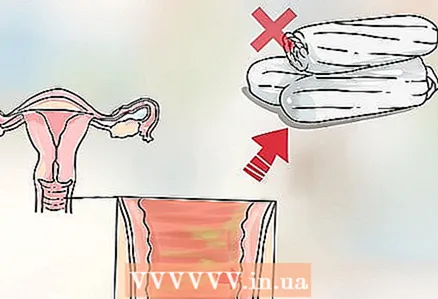 5 Take enough time to physically recover from your miscarriage. It will most likely only take you a few days to feel healthy again.
5 Take enough time to physically recover from your miscarriage. It will most likely only take you a few days to feel healthy again. - Be prepared for your period to resume as early as next month. This means you can get pregnant again. If you don't want to, use contraception.
- For two weeks, do not have sex or use tampons, as this can interfere with the repair of tissue in the vaginal walls.
 6 Take time to restore your mental health. Research shows that a woman can experience intense sadness no matter how long she has lost her baby. So don't beat yourself up for your feelings, but rather surround yourself with people who can help you cope with your grief.
6 Take time to restore your mental health. Research shows that a woman can experience intense sadness no matter how long she has lost her baby. So don't beat yourself up for your feelings, but rather surround yourself with people who can help you cope with your grief. - Get the support of trusted friends and family members.
- Find a support group.
- Most women who have miscarried in the past have been able to bear and give birth to a healthy baby. A miscarriage does not mean that you will not be able to have a baby in the future.
Method 3 of 3: Planning a Pregnancy
 1 Learn about the causes of the miscarriage. A miscarriage early in pregnancy often occurs because the fetus is not developing properly. This can happen for many reasons, including genetic disorders of the fetus and poor maternal health.
1 Learn about the causes of the miscarriage. A miscarriage early in pregnancy often occurs because the fetus is not developing properly. This can happen for many reasons, including genetic disorders of the fetus and poor maternal health. - Genetic abnormalities of the fetus. Among the causes of abnormal development of the fetus, there are both hereditary factors and disorders that occur in a particular egg and sperm.
- Diabetes in the mother.
- Infection.
- Hormonal disorders in the mother's body.
- Thyroid disease.
- Diseases of the uterus or cervix.
 2 Reduce the risk of future miscarriage as much as possible. While miscarriage is not always preventable, there are a few things you can do to reduce your risk of miscarriage. The risk of miscarriage is increased by:
2 Reduce the risk of future miscarriage as much as possible. While miscarriage is not always preventable, there are a few things you can do to reduce your risk of miscarriage. The risk of miscarriage is increased by: - Smoking.
- Alcohol.Alcohol can cause irreparable harm to your baby, even if it does not miscarry.
- Drugs. Stop using drugs if you are pregnant or trying to get pregnant. Do not take medicines, even over-the-counter or herbal medications, without talking to your doctor.
- Diabetes.
- Overweight or underweight.
- Diseases of the reproductive organs, in particular the uterus or cervix.
- Environmental toxins.
- Infections.
- Immune system disorders.
- Hormonal imbalance.
- Invasive diagnostic methods such as amniocentesis or chorionic biopsy.
- The woman is over 35 years old.
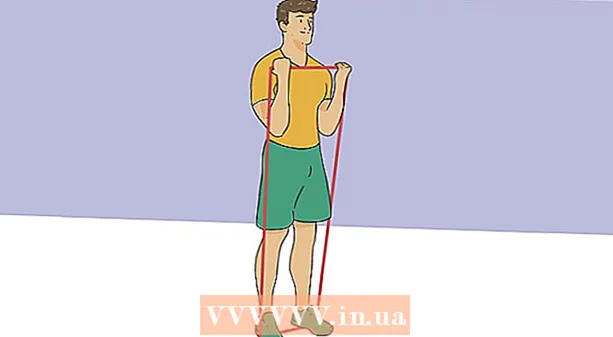
 3 Learn about activities that may not cause a miscarriage. The following activities, which are mentioned below, may not cause a miscarriage. However, if your doctor makes recommendations other than these, then follow the recommendations of the obstetrician-gynecologist.
3 Learn about activities that may not cause a miscarriage. The following activities, which are mentioned below, may not cause a miscarriage. However, if your doctor makes recommendations other than these, then follow the recommendations of the obstetrician-gynecologist. - Moderate exercise.
- Safe sex. Protect yourself from infections.
- Work that does not expose you to environmental toxins, infectious agents, chemicals, or radiation.