Author:
Monica Porter
Date Of Creation:
22 March 2021
Update Date:
1 July 2024

Content
Lymphedema is an accumulation of fluid in the body's soft tissues due to obstruction or removal of the lymph nodes. Lymphedema is usually caused by lymph node removal after cancer treatment, but it can also be caused by environmental or genetic factors. Most lymphedema develops within 3 years of surgery. Lymphedema can also be caused by an abnormal growth of the lymphatic system at birth and symptoms may appear later. Recognizing symptoms and treating them early is the best way to prevent lymphedema.
Steps
Method 1 of 3: Prevention of lymphedema
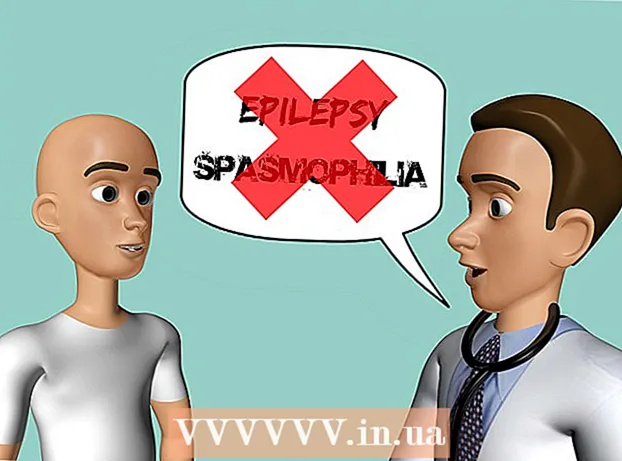
Talk to your doctor as soon as you notice signs of lymphedema. Signs of lymphedema include swelling in the arms, legs, hands, fingers, neck or chest. If you notice any swelling or other signs (listed below), you should see your doctor immediately.
- Recognizing the early signs is the best way to prevent the disease from getting worse.
- There is no cure for lymphedema, but early treatment can help ease symptoms and prevent other symptoms.
- Lymphedema may appear days, weeks, months, or even years after cancer treatment.
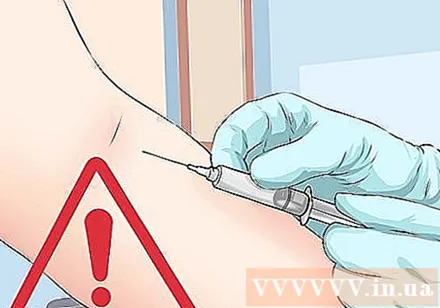
Avoid extracting blood from the arm at risk of lymphedema. Lymphedema usually appears on the surgical site of the body. You should avoid injections or intravenous infusions in the hands that are at risk of lymphedema- When measuring your blood pressure, you should take a hand measurement with less chance of developing lymphedema.
- Consider purchasing a medical alert bracelet to warn others not to take blood, take an intravenous infusion or inject into the arm at risk of developing lymphedema.

Do not take a hot bath for too long. Do not expose the arms or legs that are likely to get lymphedema in contact with hot water, heat or high temperature. If you want to take a hot bath, avoid soaking your hands in the water.- Do not use hot packs or other heat treatments.
- Do not massage too hard in areas at risk of lymphedema.
- The high temperature and massage will push the body's fluids back into the sensitive area, thereby inducing lymphedema.
- Keep your arms out of the sun if possible.

Do not carry heavy objects or carry heavy bags on the shoulder. To recover from surgery or cancer treatment, you should avoid using the affected part of your body to carry heavy loads. You should be careful to avoid putting great pressure on the arm as there is a risk of lymphedema.- When carrying heavy loads, you should raise your arms above your hips.
- After you get better, you can slowly carry heavy objects.
Do not wear tight clothing or jewelry. If watches, rings, bracelets or other jewelry tighten too tight, loosen them or stop wearing them. Also, wear loose clothing that does not obstruct movement.
- Avoid wearing tight-necked tops if there is a risk of head or neck lymphedema.
- Over-wrapping or tightening around the neck, arms, legs, wrists and other body parts can cause fluid to accumulate in that area.
Raise your arms / legs up high. If you are at risk for lymphoedema, raise the part of your arms / legs that are at risk if possible. This will help prevent fluid from accumulating in the hands / feet to prevent swelling.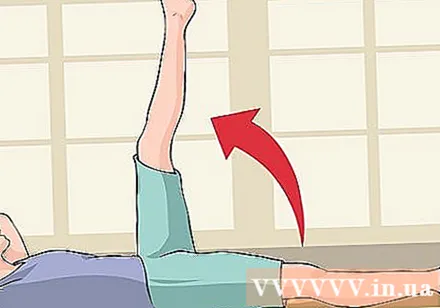
- This preventive measure is most effective in preventing lymphedema from developing in the arm, hand or finger.
- If you sleep on your back, keep your feet higher than your heart. For example, you could put a pillow under your knee or foot.
Change your posture. Do not sit or stand in one place for too long. Instead, change your position often. Do not cross your legs while sitting and should sit with your back on the bed.
- Sitting upright while in bed helps to improve lymph drainage in the body.
- You can set an alarm in your phone or set a clock to remind yourself to move often. Also, make use of natural objects / events to remind yourself to move. For example, when watching TV, you should change position every time you go to an advertisement.
Wear protective clothing. Cuts, sunburns, burns, insect bites, cat scratches can all cause fluid to accumulate on the affected area, increasing the risk of lymphedema. Wearing loose, long clothing can help protect the skin from these damage.
- Should wear loose fitting, not too tight.
- Do not wear protective sleeves (usually for athletes) as the sleeve will squeeze the arm.
Protect hands and feet from injury. Any cuts, open wounds, scratches or burns in an area of an arm or leg that has lymphedema can cause an infection. An infection will prevent the lymph fluid from filtering bacteria and viruses. Signs of infection include: swelling, pain, redness, warmth, and fever. If you have these symptoms, you should immediately go to the nearest hospital for treatment and control of the infection.
- Do not allow sharp objects to puncture the skin.
- Always use a dyke when sewing, wear thick gloves when gardening, and apply insect repellent when going out.
- Keep skin moisturized by applying a gentle moisturizer to prevent dry and chapped skin.
- Take extra care when shaving if using a regular razor.
- If you do a manicure, you should not let the cuticles right or pull off the cuticles. You should have a manicure in a place where a technician knows your health condition for special attention. If the manicurist is new, you should carefully check their health. Do not work on a nail in a location with poor hygiene rating or where a client has had a fungal, bacterial or viral infection.
- Wear gloves when doing household chores or gardening to avoid damaging your hands, fingers or nails.
- Wear comfortable, toe-fitting shoes to reduce the risk of damage to your feet and toes.
Eat a balanced, low-salt diet. Each meal should have 2-3 servings of fruit and 3-5 servings of vegetables. Eat high-fiber foods, including breads, whole grains, whole-grain pasta, rice, and fresh vegetables. It's best to avoid alcohol (up to 1 serving per day).
- Avoid consuming fast foods or junk food that are high in calories, not nutritious.Not only are these foods high in calories and low in nutrients, these foods are also very high in salt.
- Limit your consumption of red meat and processed meat products such as sausages or bacon.
Maintain a healthy weight. Both being overweight or obese contribute to an increased risk of lymphedema. Excess weight puts additional pressure on an area of the body that is already swollen, thereby affecting the drainage of lymphatic fluid.
- A balanced diet, exercise, and obedience are key to maintaining an ideal weight.
- If you need help, you can consult a doctor. Your doctor can give you suggestions based on your medical condition.
Maintain a healthy lifestyle. Achieving and maintaining a healthy weight helps prevent lymphedema from developing. Follow healthy eating habits and exercise regularly to lead a healthy lifestyle.
- Getting enough sleep helps maintain a healthy immune system and reduces the risk of lymphedema.
- Talk to your doctor to develop a healthy exercise program. Intense exercise is not recommended. You should try to exercise every day.
No smoking. Cigarette smoking narrows the capillaries and small blood vessels, making it difficult for fluid to circulate freely in the body. Smoking also removes oxygen and other essential nutrients for a smooth circulation of fluids. Skin elasticity is also damaged by smoking.
- If you need help quitting smoking, you can talk to your doctor about how to quit smoking. There are many resources available to help you quit smoking.
- Quitting smoking also helps to reduce the risk of cancer and other health problems.
Method 2 of 3: Recognize symptoms of disease
Watch for swelling in your arms, legs, breasts, or hands. Swelling of soft tissue in the arm or leg is one of the most common signs of lymphedema. In the early stages, the skin is still soft and the swollen area is concave when pressed down.
- Your doctor may use a tape measure to measure the swelling and monitor where the swelling is.
- In later stages of lymphedema, the swollen area becomes firm and stiff. When pressed, the swollen area will not sink.
Notice how heavy your arms or legs are feeling. Next to the bump or before you see the bump, you may feel the fluid build up, making it hard to move your arm or leg. If you are at risk for lymphatic disease, this could be the early sign of the disease.
- If you have had surgery, radiation therapy, or lymph node removal surgery, you should look in the mirror to detect the swelling (if any).
- Compare the sides of your body to find the differences.
Note if you have difficulty moving the joint. A feeling of stiffness in your fingers, toes, knees, elbows and other joints can be a sign of increased fluid buildup due to lymphedema. Although there are many causes of stiffness, pressure in the joint due to accumulation of body fluids may be a sign of lymphedema.
- Lymphedema symptoms can appear slowly or at the same time.
- Understand yourself for any abnormalities.
Note if your toe or foot feels itchy or burning. That could be a sign of cellulitis - an infection of the skin and not a infection. Since lymphedema affects the immune system, you should see your doctor as soon as you notice symptoms of cellulitis.
- Cellulitis can be caused by an insect bite or scratch.
- The doctor will treat the infection with antibiotics. Do not be subjective when there are signs of infection because the infection can quickly be life-threatening.
Check for signs of thickening (hyperkeratosis). Fluid build-up can cause the skin to thicken. If you notice thicker skin in your arms, hands, legs, feet, or other skin changes such as blisters or warts, it could be a sign of lymphedema.
- Keeping skin clean is an important step for people with hyperkeratosis.
- Use a daily therapeutic moisturizer and avoid lotions that contain lanolin or scented lotions.
Note if the clothes or jewelry does not fit. People with lymphedema often feel uncomfortable wearing a bra, even without gaining weight. In addition, wearing a ring that doesn't fit your hand, and is uncomfortable with a watch and bracelet can also be a sign of lymphedema.
- You may find it difficult to fit one arm into your sleeve.
- Since lymphedema symptoms can develop slowly, you should not feel swelling in your shoulders or arms until you have difficulty getting dressed. If you find that the clothes are one-sided tight or difficult to fit a T-shirt or jacket, you should pay attention to detect signs of lymphedema.
Look for tight, shiny, warm, or red skin. The skin can be "shiny" or "stretched". That could be a sign of cellulitis. If the color or texture of your skin changes, you should see your doctor immediately.
- Affected skin can spread rapidly when observed.
- Other (uncommon) symptoms include fatigue, fever, soreness or cold-like symptoms.
Method 3 of 3: Recognize the head / neck mark
Watch for swelling in the eyes, face, lips, neck, or under the chin. The signs of head and neck lymphedema usually appear 2-6 months after cancer treatment in the head area. Occasionally lymphedema will develop in the larynx and throat (mouth and throat). The disease can also develop beyond the neck and face, or both, depending on the blocked lymph channel.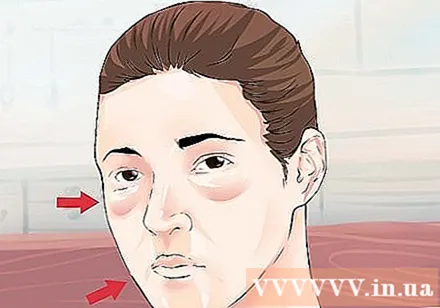
- See your doctor if you have any of these signs of head or neck lymphedema.
- Uncontrolled swelling can lead to inflammation that quickly becomes out of control.
Feel the tension or swelling in the area of the body affected. Since it is difficult to see the swelling of the head and neck, the first symptom of the lymphedema of the head and neck is usually through sensation. You should watch out for any signs of tension in the head and neck area.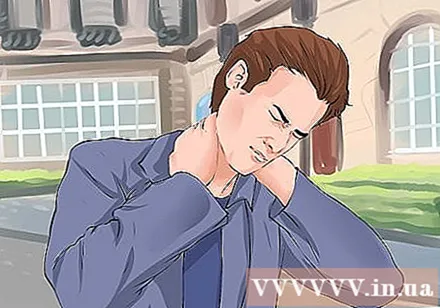
- You may find it difficult to move your head, neck or face. The skin also feels stiff or uncomfortable, though no visible swelling is visible.
- The doctor may perform additional tests to check for lymphedema, including radiuclides-imaging of the lymphatic system or another imaging technique that relies on injections of contrast dye to show abnormal lymphatic circulation.
Be wary if eye swelling affects vision. Blurred or uncontrolled watery eyes, red eyes, and sore eye sockets can all be signs of double eyelash-lymphedema syndrome. This disease is inherited at birth but may not appear until puberty.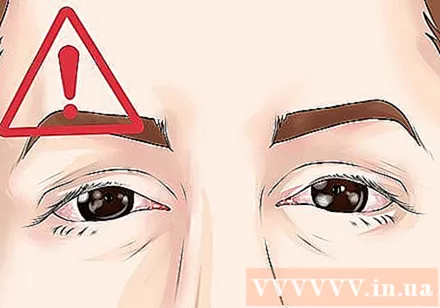
- Growth of extra lashes along the inner lining of the eyelids is also a sign of double eyelash-lymphedema syndrome.
- Other vision problems caused by the disease include abnormally curved corneas and corneal scarring.
Watch for trouble swallowing, speech, or breathing. In more severe cases of lymphedema, swollen tissue in the throat and throat interferes with normal functions. You may salivate or drop food from your mouth.
- The swelling can lead to a stuffy nose or pain in the ear. Swelling can affect the sinus glands and sinus cavities.
- To confirm lymphoedema in the neck and head, your doctor may perform an ultrasound or a magnetic resonance imaging (MRI) scan. These tests show the position of the lymph fluid in the head.
Advice
- Even if you are at risk for lymphedema, you should see your doctor to rule out other causes of lymphedema symptoms.
Warning
- See your doctor right away if you have signs of infection such as fever above 38 ° C, sweating, persistent chills, skin rash, or other skin abnormalities such as pain, redness, or swelling.