Author:
Louise Ward
Date Of Creation:
12 February 2021
Update Date:
1 July 2024

Content
Asthma is the most common chronic school-age illness, affecting approximately 7 million children in the United States. This is an inflammation that narrows the airways and people find it hard to breathe. They often experience periodic "asthma attacks" with worsening symptoms. If not treated properly, an asthma attack can progress and lead to serious injury or death. So you have to detect asthma attacks in children quickly and accurately.
Steps
Part 1 of 4: Listen to young children
Watch for agents from the environment. Most children with asthma usually begin to show signs at the age of 5, when they begin to react negatively to the asthma triggers. An asthma trigger is anything that causes a symptom to flare. The triggers are not the same for every baby, so be aware of what might trigger a flare-up, especially if you suspect an asthma attack is coming. Some agents (like dust mites and fur) can be eliminated, but others (such as air pollution) need to be carefully monitored. The most common agents are: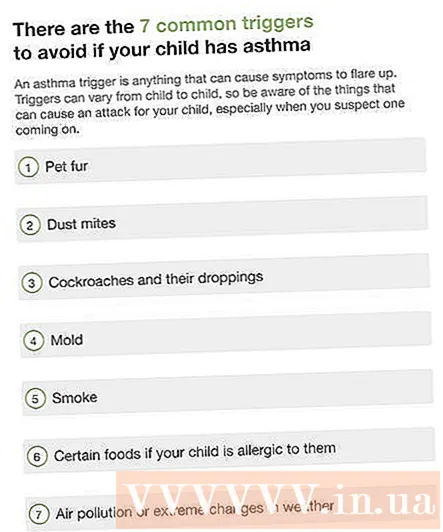
- Fur: vacuum or mop regularly to remove hair.
- Dust mites: Use upholstery and pillowcases to protect your baby from dust mites, wash bedding often, avoid stuffed animals in your baby's room and do not use pillows or down blankets.
- Cockroaches: cockroaches and their droppings are a common asthma trigger. To keep cockroaches away from your home, cover all food and water sources. Wipe away spilled food after eating and clean the house regularly. Refer to purchasing insect control equipment.
- Mold: mold is caused by moisture, so you can use a meter to check moisture indoors. Use a dehumidifier in the air to avoid mold.
- Smoke: Regardless of tobacco smoke or wood smoke, it can trigger an asthma attack. Even if you go out to smoke, the remaining smoke on your clothes and hair will put your child in danger.
- Some foods: Eggs, milk, peanuts, soy products, flour, fish, shellfish, salads, and fresh fruit are all foods that can trigger an asthma flare-up if your child is allergic. corresponding to them.
- Air pollution and extreme weather changes.

Observe the child's behavior. Keeping a clean environment free of triggers may not be enough. When a child has strong emotions like sad, happy, fearful, and so on, the risk of an asthma attack is also higher. Similarly, too much exercise causes children to run out of breath and must breathe quickly and deeply, easily leading to an asthma attack.
Treat respiratory tract infections properly. Viral or bacterial infections in the upper respiratory tract or the lower respiratory tract can both trigger an asthma attack. Children must be examined in pediatrics if they show signs of respiratory infections. Your baby may have to take medicine to control the infection or to get the disease over faster.- Remember that antibiotics only cure bacterial infections. Respiratory viral infections need to be approached from a control rather than a therapeutic perspective.
Part 2 of 4: Assessing the child's breathing

Watch for signs of rapid breathing. Usually adult breathing is no faster than 20 breaths per minute. Depending on age, children may experience faster resting respiratory rates. It's best to watch for any signs that your baby is breathing abnormally fast.- Children 6-12 years old usually breathe 18-30 beats per minute.
- Children 12-18 years old usually breathe 12-20 breaths per minute.
Notice if your baby is trying to breathe. When breathing normally, young children mainly use the diaphragm for breathing. However, with children with asthma they have to use other muscles to help get more air. Look for signs that your baby's neck, chest, and abdominal muscles are working harder than usual.
- A child trying to breathe will usually bend over with his hands on his knees or desks. If you see this position, chances are your baby is having an asthma attack.
Listen for wheezing sounds. Children with asthma, when breathing, often make a small, vibrating hissing sound, particularly when they exhale because the air is forced through narrow channels.
- You can hear wheezing in both inhalation and exhalation, and note that when a child has a mild asthma attack or at the onset of a severe asthma attack you can only hear wheezing when the child exhales.
Watch for coughs. Asthma is the most common cause of chronic cough in children. Coughing causes the pressure in the airways to increase and force the passage to expand, temporarily allowing better air flow. So even though babies breathe easier when they cough, it's a symptom of a bigger problem. Children often cough when their bodies are trying to push environmental factors out, which is the cause of an asthma attack.
- However, a cough is also a sign of a respiratory infection, which can trigger an asthma attack.
- A nagging nighttime cough is a common symptom that a child has mild to moderate asthma, but if the cough continues for long periods of time, then the baby is likely to have an asthma attack.
Look for signs of contraction. Contraction is a "in" phenomenon seen in the middle or just below the ribs or collarbone while the child is breathing. This happens when the muscles have to work harder to pull air in, but the air can't fill the space in time because the airways are blocked.
- If there is slight contraction between the ribs, you should see your baby as soon as possible. If the condition is moderate to severe, your baby should be taken to the emergency room immediately.
Look for signs of enlargement of your nostrils. When your baby is trying to breathe, you often notice that her nostrils are enlarged. This is a helpful sign of an asthma attack happening in infants and very young children.At this age, the child may not be able to show symptoms or display a crouch position as in an older child.
Watch for signs of "standing still chest". If your child seems to be showing discomfort but you can't hear wheezing, a "standing chest" phenomenon may be happening. This is a sign in severe cases when the airways are so blocked that there is not enough air to make a wheezing noise. You must take your baby to the emergency room immediately. Children can be exhausted after trying to breathe and no longer have enough force to push the carbon dioxide gas out, which also means not getting enough oxygen for the body.
- Another sign that the baby is not getting enough oxygen and needs immediate medical attention is when the baby is unable to complete sentences.
Use a peak flow meter to determine the severity of your asthma attack. A peak flow meter is a simple device used to measure the "peak expiratory flow" (PEFR). You should measure this flow daily to find out your child's normal PEFR. Abnormal readings will be an early warning sign that will help you predict asthma attacks. The normal range for PEFR depends on the child's age and height; You should ask your doctor about the values of each "zone" and what to do if your child is in the red or yellow zone. As a general rule:
- The PEFR index is 80-100% of the PEFR scale required for an individual meaning that health is in a "green zone" (low risk of asthma).
- A PEFR of 50-80% of the PEFR scale required for an individual means that health is in the "yellow zone" (average risk, follow up and care for the child as directed by the doctor).
- Less than 50% of the PEFR scale required for an individual means there is a high risk of an asthma attack. Give your baby immediate treatment and go to the hospital afterwards.
Part 3 of 4: Evaluate the child's appearance
Consider the overall appearance. Children with asthma attacks often have to try to breathe, so you can notice it from the outside. If you notice that your baby is trying to breathe or “something is wrong,” trust your intuition. Have your baby use inhalers or other immediate treatment prescribed by the doctor and go to the hospital as soon as possible.
Watch for pale, cold, and damp skin. During an asthma attack, a child's body has to work harder just to breathe, so the skin is often sweaty or wet. Instead of having a red or pink color caused by an exercise, your skin looks pale or white during an asthma attack. Blood is red when it comes into contact with oxygen, so if a child doesn't get enough oxygen you won't see the pink color of the blood.
Pay attention to the green color of the skin. If you notice blue skin or blue lips and nails, your baby is having a very bad asthma attack. It is a sign that the baby is severely lacking in oxygen and must be treated immediately. advertisement
Part 4 of 4: Taking care of your child during an asthma attack
Provide asthma medicine. If your child has had asthma in the past, he or she may have asthma medicine prescribed at home, usually in the form of a spray. If so, you need to let your baby inhale the medicine as soon as the asthma attack happens. How to use the spray is quite simple, but the effectiveness will decrease if you use it incorrectly. Use the inhaler properly as follows:
- Remove the cap and shake the tube vigorously.
- Spray the air a little if needed. If it is new or has not been used for a long time, you should spray a small amount of medication out before using it.
- Ask your baby to exhale completely, then inhale as you inhale the pill.
- Continue asking your baby to inhale slowly and deeply for 10 seconds.
- Always use a spacer to let the medication get into the lungs instead of the back of the throat when using a baby inhaler. Ask your doctor about how to use the inhaler with a cushion chamber.
Check the label on the medicine tube before you give the second dose, to see if you have to wait a while. If you take a thuốc2-agonist like albuterol, wait a full minute before giving your baby another dose. But if it is not a β2-agonist then you may not have to wait.
Observe if the medicine is working. Usually the medicine will work a few minutes after spraying, otherwise you should give your child more medicine. Follow the dosage recommendations on the medication label or follow your doctor's advice as they may recommend more sprays right away. If symptoms persist you should bring your baby to the hospital.
Contact your doctor if you experience mild but persistent symptoms. Mild symptoms may include coughing, wheezing or breathless exertion. Contact your pediatrician if an asthma attack is mild but symptoms do not improve after taking medication. There are cases where the doctor needs to directly treat the child in the clinic or give you more specific instructions.
Go to the emergency room for very severe and persistent symptoms. A "standing still chest" or blue lips and nails indicate that a child is not getting enough oxygen. When you experience these symptoms, you need immediate treatment to avoid the risk of brain damage or death.
- If asthma medication is available you should give it to your baby on the way to the emergency room, and never delay taking him to the emergency.
- Delayed treatment during a severe asthma attack can cause permanent brain damage or even death.
- Call the emergency number if your child turns pale that does not go away after taking the medicine, or if the signs of pale pale spread out from the lips or fingernails.
- Call 911 if your child is unconscious or difficult to wake.
Get emergency medical help for asthma attacks that occur due to an allergic reaction. If a child's asthma attack is triggered by a food allergy, insect bite or medication use, seek immediate medical attention. These types of allergies can progress quickly and lead to airway obstruction.
What will they do in the emergency room? The doctor first confirmed the signs and symptoms of asthma. After going to the emergency room, the health staff will give the child oxygen if needed and give more medicine, but if the asthma attack is too severe they may need to inject corticosteroids into the vein. Most patients recover with the care of a specialist and you can bring your baby home early. However, they should stay in hospital overnight if the condition doesn't improve after several hours.
- Your doctor may order a chest x-ray, a pulse measurement or a blood sample.
Advice
- Recognize situations that can trigger or worsen an asthma attack, such as allergens exposure, prolonged physical activity, passive smoking, respiratory infections and extreme emotions .
Warning
- Asthma is a dangerous and potentially fatal disease. Always seek immediate treatment for a child with severe symptoms, including difficulty breathing, pale paleness, rapid pulse, heavy sweating, sudden feeling of restlessness or lethargy.