Author:
Louise Ward
Date Of Creation:
8 February 2021
Update Date:
2 July 2024

Content
Eczema is a general term used to refer to a number of skin conditions. The three most common types of eczema are atopic eczema (atopic dermatitis), contact eczema (contact dermatitis) and eczema. How to control a flare-up will depend on the type of illness. People tend to go through a period of eczema: when the skin is normal, with its first signs and symptoms, and a strong eczema flare-up.
Steps
Method 1 of 4: Understand different types of eczema
Determine what triggers atopic eczema. Atopic eczema is essentially a chronic allergic reaction. It is most common in babies and young children. However, adults can also develop atopic eczema. Flare-ups can be caused by irritants, allergens, stress, fabrics and dry skin. If you have a food allergy, you are at higher risk of developing atopic eczema.
- Atopic eczema is often passed from generation to generation and people who are prone to atopic eczema are also more likely to have fever or asthma.
- Atopic eczema in a newborn usually starts in a baby's head, cheeks, or scalp and can spread to other areas. The eczema shows up as small, itchy red bumps or a scaly rash. When it spreads, the eczema usually appears in the elbows or knees and can spread throughout the body, especially in babies. Atopic eczema is not contagious.

Determine what triggers eczema contact. Contact eczema (contact dermatitis) is also an allergic but not as chronic as atopic eczema. Contact dermatitis occurs only when the skin comes in contact with a specific irritant. The most common irritants are certain metals, poison ivy, soaps and even perfumes or makeup. Contact eczema is also not contagious.- Contact eczema also manifests itself as small, itchy red blisters. The blisters can drain and turn into a scaly area of the skin.
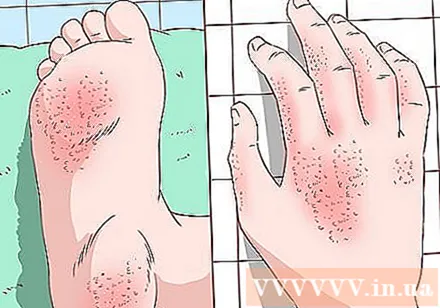
Determine the risk of leukoplakia. Eczema is less common than atopic eczema. The disease usually appears only on the hands and feet. An eczema flare-up can be caused by stress, allergies, overexposure to water, dry skin, and exposure to certain metals such as nickel.- Eczema is initially an itchy, small patch of blisters. When it breaks, the skin appears scaly.
- Women are twice as likely to get eczema as men.
- Chronic leukoplakia usually develops less often after middle age.
Method 2 of 4: Control atopic eczema

Apply corticosteroid cream. Although it takes up to 3 weeks, this cream significantly reduces eczema flare-ups. Your doctor can prescribe drugs that are stronger than over-the-counter medications.- The best time to apply the cream is right after bathing. Apply the cream to the eczema area.
- Corticosteroid creams should only be used when instructed by your doctor because the cream can have serious side effects if used for too long on a specific area of skin.
Take a warm bath. Warm water can help reduce eczema symptoms and flush toxins from the skin. Children with eczema should only take a warm bath once a day for no more than 10 minutes. You can add a little bath oil to the water and apply moisturizer or corticosteroid cream to your baby after bathing.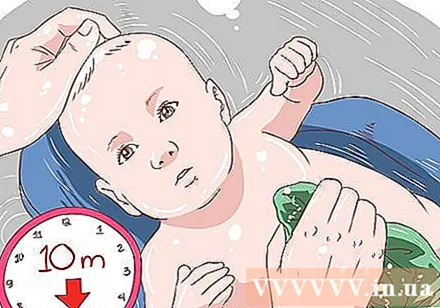
- Oatmeal glue is also effective in some cases. You can buy oatmeal glue at a drugstore. Put the glue in a bath of warm water and soak for 10-15 minutes.
- When your skin becomes infected, take a bath to soften the flakes. Gently rub the scales away after soaking so that the cream can be applied directly to the skin.
- Do not add bath soaps or other additives to the bath to avoid skin irritation.
Ask your dermatologist about a bleach bath. A bleach bath may sound harmful, but it is actually very helpful in destroying skin bacteria caused by eczema. If your doctor agrees, you can place 1/2 cup of household bleach in a tub of warm water. You or your child can soak in a bleach bath once a day for no more than 5-10 minutes.
- To make a bleach bath for babies and toddlers, add 1 teaspoon of bleach to 4 liters of water.
- Do not apply bleach directly to the skin. This action may cause irritation.
Get rid of irritants. While not easy, getting rid of irritants or allergens can help control atopic eczema.Irritants such as soap, laundry detergent, perfume and cigarette smoke can all cause atopic eczema flare-ups.
- When removing irritants that affect people with atopic eczema, try getting rid of them one at a time. For example, you can start using a more natural laundry detergent. If the laundry detergent is not an irritant, you can try changing the bath soap to a different one.
Eliminate allergens. With atopic eczema, you may become more sensitive to certain allergens, including foods and airborne allergens. They may cause a normal response or cause atopic eczema to flare. You should find ways to identify allergens by keeping a food diary so you can track an allergic reaction to a consumed food.
- In food allergies, foods such as peanuts, wheat, soy, milk and eggs can cause an allergic reaction, including eczema, in children and adults with atopic eczema.
- You may also be sensitive to certain airborne allergens such as pet hair, pollen, and dust.
- Ask your doctor about an allergy test if you can't identify the allergen or allergen yourself.
- Some food allergies, especially peanuts, can be life-threatening. If you suspect that you or your child has a food allergy, seek medical help immediately.
Avoid using certain fabrics. Fabrics that rub against skin such as wool and some man-made fabrics can cause atopic eczema flare-ups. Therefore, you should choose fabrics that do not rub the skin and wear clothes that fit. Natural fabrics such as cotton, silk and bamboo are suitable options. Avoid using wool fabrics.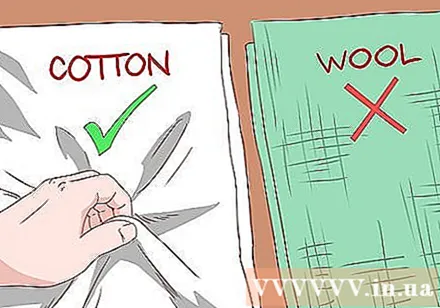
- In addition, you can buy clothes that do not mark or be sure to remove the clothing label when wearing to avoid rubbing the skin.
- Always wash new clothes before you wear them, as they can still be contaminated with dyes and irritating chemicals.
Apply a moisturizer or lotion twice daily. Always keep your skin moist to minimize eczema flare-ups. Besides, moisturizer also helps soften the skin, soothe the pain of eczema.
- Choose a cream that is thick and without flavoring. Aromatherapy can irritate the skin if the skin is eczema. In fact, some products like moisturizer wax are also very effective.
Try moist wraps. Moist wrap therapy is the process of applying a moist bandage to your skin at night to soothe the eczema area. This therapy helps to cool down the skin, prevents you from scratching the itch and helps moisturize the skin.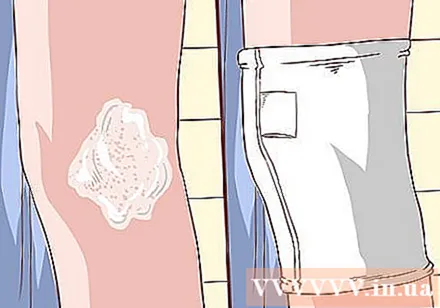
- First, apply corticosteroid cream to the eczema area. Then apply moisturizer all over. Remember, corticosteroid cream should only be applied to eczema.
- Soak a washcloth, clean gauze or paper towel in water with a small amount of odorless shower oil. Wrap a wet washcloth around the eczema area, especially the area most severely affected. You may need to wrap your entire arm and leg if your eczema is severe. You can try wearing damp clothing if your breasts are irritated.
- Remove the bandage the next morning. Or you can also wrap the bandage all day, but remember to remove it when it is dry.
- Place a cool, slightly damp washcloth on your face, but don't wrap it around your face. Apply for about 5 minutes.
Don't scratch. Scratching makes the rash worse. In fact, scratching the rash can cause the skin to thicken and cause infection.
- If it is difficult to control the scratching, keep your fingernails short or wrap your fingertips with a band-aid.
Take an antihistamine. Oral antihistamines such as Diphenhydramine (Benadryl) can help relieve itching caused by eczema. Since the drug can cause drowsiness, it is best to take it before bed.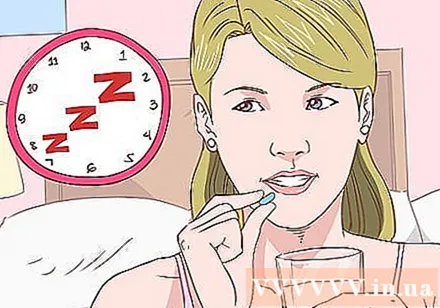
Ask your doctor about other options. If the atopic eczema does not go away with home treatment, your doctor may recommend other topical or oral medications. In addition, your doctor may refer you to a dermatologist for a prescription for other medications.
- If the skin is infected or has an open wound due to scratching, your doctor may prescribe an antibiotic.
- Your doctor may prescribe a corticosteroid medication either by mouth or by injection. These drugs inhibit inflammation by "mimicking" the natural effects of hormones in the body in larger doses. It also has the potential to cause side effects and is not recommended for mild eczema or long-term use.
- Another option is a skin regeneration cream. Calcineurin inhibitors (eg Tacrolimus, Pimecrolimus) have the ability to alter the immune system when applied to the skin, helping to reduce atopic eczema flare-ups. These drugs can cause serious side effects, so they should be used only in severe cases.
Method 3 of 4: Control contact eczema
Get rid of irritants. If you notice a rash when you touch something, wash your skin thoroughly with warm water and soap.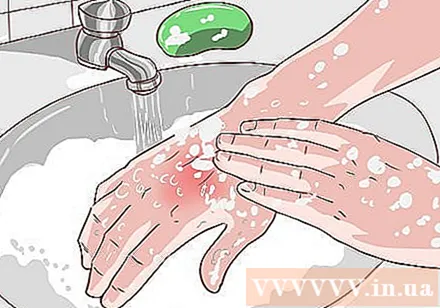
- The skin may become red, small, itchy, with small blisters and / or warm skin.
- Also, wash / wash off items that come into contact with irritants that you use regularly like clothes.
Don't scratch. Although it is difficult to restrain, you should avoid scratching as much as possible. Scratching will make your rash worse and possibly cause infection.
Use an antihistamine. Because contact eczema is a form of allergic reaction, you can take over-the-counter antihistamines such as Loratadine or Cetirizine. Take it once a day for symptom control.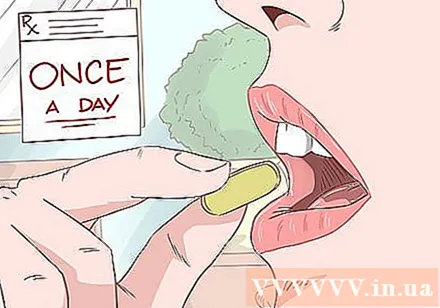
Eliminate irritants and allergens. Similar to atopic eczema, contact eczema can be triggered by allergens or irritants, even if you only inhale or eat them. Make sure to swap out soap and laundry detergent to determine what triggers are, and keep a food diary to identify foods that trigger a flare-up of your eczema.
- Note there can be more than two factors causing eczema. Eczema can have flare-ups caused by both makeup and sunscreen. In addition, sunlight can sometimes be a trigger for eczema when combined with another irritant.
Ask your doctor about an allergy skin test. A skin patch test is one way to help determine the cause of contact eczema. Your doctor will apply certain allergens and irritants to your skin and you will take them with you for 48 hours. When you return to the clinic, your doctor will determine which triggers you are reacting to to help avoid future exposure.
Avoid allergens and irritants. Once you've identified the cause of your contact eczema, avoid them. For example, if a laundry detergent or soap causes eczema contact, you will need to switch to another brand product, preferably natural and fragrance-free.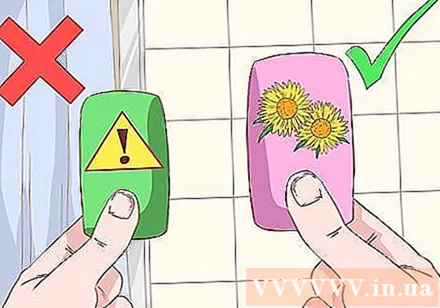
Use moisturizers regularly. Moisturized skin is less prone to eczema. In addition, moisturizer can help relieve eczema pain by softening chapped skin.
- Apply a thick moisturizer to your skin several times a day.
Try wet wrap. As is the case with atopic eczema, severe contact eczema can be treated with a wet wrap. Apply a wet bandage or towel over the moisturized area overnight to soothe the skin.
Use steroid creams. Like atopic eczema, contact eczema can be relieved with steroid creams. Apply the cream to eczema-prone skin after bathing or at night.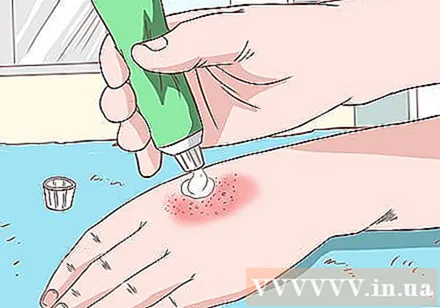
Ask your doctor about oral corticosteroids. If the reaction is too severe, ask your doctor about oral corticosteroid medications. Medications can help reduce inflammation in the body.
- You may also need to take antibiotics if the rash becomes infected.
Method 4 of 4: Control leech eczema
Use a moisturizer or ointment. Creams and ointments are especially helpful in the case of leech eczema - which usually appears on the hands and feet. Choose a moisturizer specifically formulated for the skin of your hands and feet.
- Moisturizing waxes can also help keep skin moisturized.
- You can buy skin protection creams like Tetrix to help reduce your exposure to irritants. Tetrix cream is very useful in cases where you have to control irritants like water, cement or nickel while working.
Use corticosteroid creams. Corticosteroid creams are very effective for any form of eczema. Your doctor may prescribe a corticosteroid cream to help treat flare-ups.
- Apply the cream after showering or before going to bed. In fact, you can apply evening cream and then wear cotton gloves to keep it in your hand.
Don't scratch. Scratching will make the rash worse. In addition, bursting blisters will also make the rash worse.Letting the blisters heal on their own instead of breaking them will help the skin heal faster.
Avoid water. Unlike other forms of eczema, water can irritate eczema. Therefore, you should avoid exposing your hands and feet to water as much as possible.
- Sweating can cause an eczema flare-up. If you sweat a lot, your doctor may prescribe medication to help you treat the disease.
- Also, dry hands thoroughly if they get wet.
Avoid certain metals and other irritants. Metals like nickel, chromium, and cobalt can cause eczema flare-ups. Working with concrete can expose you to these metals. Other chemicals in the workplace and environment can also cause an eczema flare-up.
- Wear gloves to avoid hand contact with irritants.
Use Calamine. This lotion helps to soothe the rash and relieve itching.
- You can apply lotion after washing your hands or after bathing.
Try soaking your hands in witch hazel water. You can buy witch hazel products from pharmacies. Witch hazel is an astringent. Soaking your hands in witch hazel helps soothe the rash and speed the recovery process.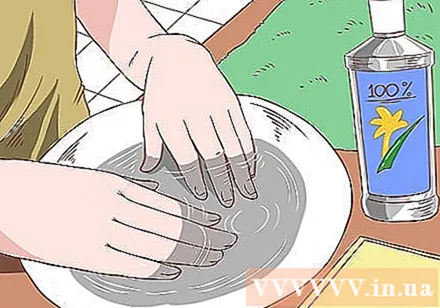
Try relaxation techniques. Eczema can flare up when you are stressed. Therefore, find ways to reduce your stress levels by incorporating calming habits in your life such as meditation.
- Identify the cause of your stress. Identifying the cause of your stress, be it work or life, is the first step in coping with stress. Avoid or change the things you can do like ignoring the bad news, and try to change your tolerance of other stressors.
- Identify the cause of your stress. Identifying the cause of your stress, be it work or life, is the first step in coping with stress. Avoid or change the things you can do like ignoring the bad news, and try to change your tolerance of other stressors.
Talk to your doctor about immunosuppressive creams or medications. Eczema is an immune response so an immunosuppressant cream or medicine may help. Some drugs in this group include Tacrolimus and Pimecrolimus.
- Your doctor can decide which cream or oral medication is more effective in your case.
Ask your doctor about phototherapy. This phototherapy can help reduce the severity of eczema, especially when taken in combination with medications to help you absorb the ultraviolet light used.
- Usually, this treatment is used only when other treatments are ineffective.
Advice
- See your doctor if you suspect you have eczema. Your doctor can help you come up with the best treatment plan.
Warning
- See your doctor right away if you notice signs of infection such as a lot of red, warm, swollen, or pus skin.