Author:
Peter Berry
Date Of Creation:
18 February 2021
Update Date:
3 July 2024

Content
The knee is protected by a crescent-shaped plate of cartilage called the meniscus. The meniscus acts as a protective pad to the outside and inside of the knee, helping to balance the knee's gravity. A torn or damaged meniscus interferes with the proper functioning of the knee and can cause pain, swelling, and stiffness in the knee joint. If left untreated, this can lead to knee instability, loss of normal knee movement, and persistent knee pain. You can follow the steps described in this article to heal torn meniscus with medication, home care, and physical therapy - or a combination of the three.
Steps
Part 1 of 4: Home care
Use the PRICE method. You can speed up the recovery process by using the "PRICE" method - short for "Protection," "Rest (rest)," "Immobilize (motionless), "" Compression, "and" Elevation. " The first rule (protection) is to avoid further damage to the pain, which can lead to more serious complications. Here's what to avoid: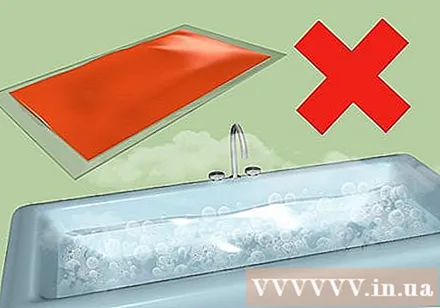
- Heat. When exposed to heat, the blood vessels dilate and possibly cause additional bleeding, so avoid hot baths, saunas, hot compresses, or even exposure to hot environments.
- Move a lot. Consider limiting some activities to avoid further injury to the pain.
- Massage. Any pressure exerted on the pain can lead to further damage.

Rested. Patients are usually advised to avoid being active for 24 to 72 hours after the injury. Adequate rest will help the wound heal properly, while also preventing damage to surrounding muscles and tissue.- Some exercises may help after the first 72 hours have passed; These exercises will be discussed below. You should perform these exercises under the supervision of a physical therapist. If not, it is best not to practice.

Keep your knees motionless. The knee can be immobilized with braces and bandages to prevent unnecessary movement that could further damage muscles and tissues. Talk to your doctor about the best practices for immobilization in your case.
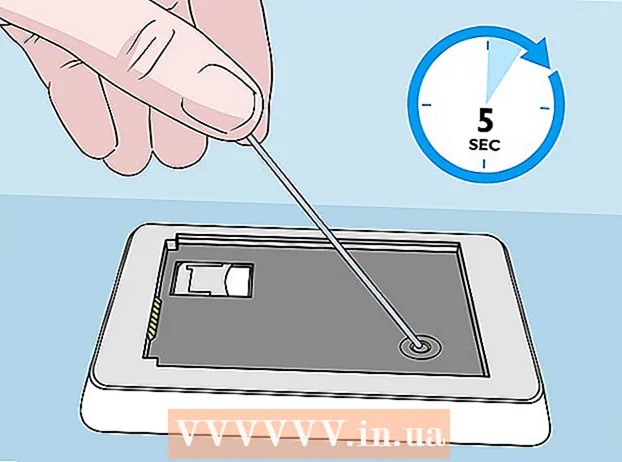
Use a pressure bandage. For the first 24-72 hours after injury, cover the affected area with ice in a damp washcloth for 15-20 minutes, 2-3 hours apart. Follow the instructions above to make sure you don't damage tissue from a cold burn.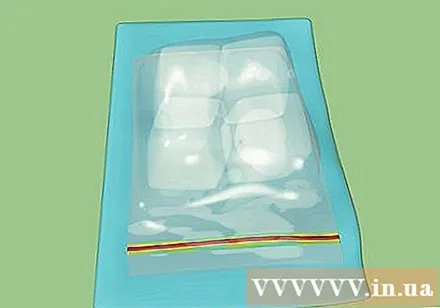
- When exposed to cold temperatures, blood vessels will contract, blood flow will decrease and the swelling will be less in pain. The compresses also help stimulate the lymph to transport nutrients to the damaged tissues around the injury.
- Lymph also works to remove waste from the cells and tissues of the body that play an important role in tissue regeneration.
- When exposed to cold temperatures, blood vessels will contract, blood flow will decrease and the swelling will be less in pain. The compresses also help stimulate the lymph to transport nutrients to the damaged tissues around the injury.

Knee elevation. Raising the site of the injury is a very important method to ensure proper blood circulation and healing. The knee elevation helps to reduce blood flow, thereby reducing swelling.- When sitting or lying down, keep your knees up on several pillows. Lie down is best, but you can also sit so that your pelvis is lower than your knee.
Part 2 of 4: Taking medications
Take a pain reliever. Over-the-counter pain relievers can be very helpful. However, it is best to discuss this with your doctor before starting any medication. Your doctor can know which medicine is best for you and / or may prescribe stronger medications for you.
- If the pain is severe and there is swelling, you might consider taking celebrex; the first dose of 400 mg is taken, followed by 200 mg twice daily.
- If you are lucky enough to have only mild pain and no swelling, you can take Tylenol 650-1000mg every 4-6 hours as needed.
- If you drink alcohol, be careful. Some drugs react with alcohol. Consult your doctor if this is the case.
Take NSAIDs. NSAIDs are a group of nonsteroidal anti-inflammatory drugs. However, this medication should not be used within the first 48 hours of an injury, because inflammation is considered one of the body's compensatory mechanisms. In other words, taking this medication during this time period may interfere with your recovery.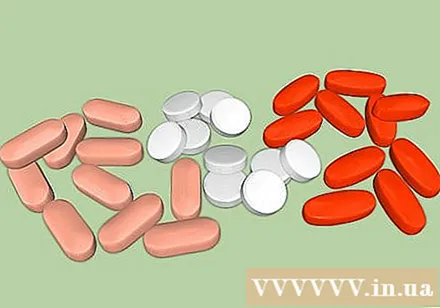
- Some examples of this group of drugs are ibuprofen, aspirin, and naproxen. All of the above drugs work by blocking certain chemicals in the body that cause inflammation in the wound.
Practice physical therapy. We will discuss physical therapy exercises in the next section. Be aware that physical therapy is often very effective at shortening the recovery process. You should talk to your doctor before starting therapy; They will know which exercise is right for you.
- Only perform exercises under the guidance of a therapist to make sure it is exercising properly and not hurting further.
Consider surgery. This option should only be taken into account when other methods are ineffective. Knee surgery may be performed to repair and join the damaged meniscus tissue to restore normal function.
- This is the meniscus removal surgery, which is the complete removal of the meniscus. Your doctor will know if this is the right choice for you.
Part 3 of 4: Physical therapy exercise
Find a licensed physiotherapist. Physiotherapy includes various exercises to help you recover. An expert physiotherapy regimen can help you regain the strength of your meniscus and optimize its function.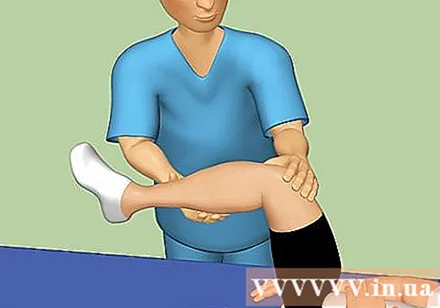
- The first five exercises described below can be performed immediately, followed by the rest once the pain has subsided.
- These exercises include muscle movements that help stimulate blood circulation and transport oxygen to the wound. An adequate supply of oxygen helps maintain cell integrity, restore function, and help repair damaged tissues.
Passive knee stretches. This exercise is often recommended when the patient loses the ability to straighten the knee.Here's how to do this exercise:
- While lying down, place a curled towel under the heel of the injured leg to raise it at least 15 cm.
- Relax your leg muscles for 2 minutes and let gravity slowly straighten your knees.
- Repeat the above step 3 times and perform the exercise as many times as you want.
Heel slide. When the pain begins to subside, you can try a heel slide exercise. Proceed as follows: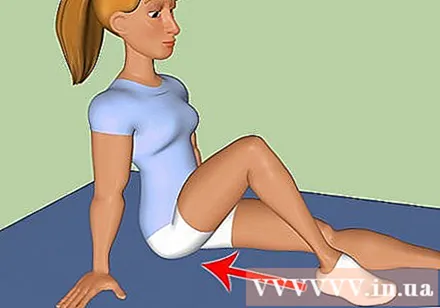
- Enter a sitting position, legs stretched in front of you and slowly slide the injured heel toward your buttocks.
- Return to starting position and repeat the exercise for 15 reps.
Stand with calves stretched. In a standing position, rest your hands on the wall at eye level. The injured leg is placed behind, the heel touches the floor. The other leg is in front and bent at the knee. With your back foot slightly inward, slowly lean against the wall until you feel the calf relax.
- Hold this position for 15-30 seconds and return to starting position. This exercise can be repeated several times a day.
Stretch hamstrings on the wall. Lie on the floor, buttocks placed near the entrance, stretch the injured leg on the exit door. Next, raise the injured leg up high and prop it up against the wall next to the doorframe. Hold this position until you feel the back of your thighs relax. Repeat 3 times.
- You can stay in a stretching position as long as you are comfortable. This stretching exercise is especially pleasant, as the entrance keeps the leg free of pressure to maintain the stretch, and the arms are also free from pressure to hold the leg.
Try raising your legs while stretching. Lie on the floor, legs stretched out. The knees of healthy legs are slightly bent, and feet flat on the floor. Tighten the thigh muscle of the injured leg and lift about 20 cm above the floor. Slowly return your feet to the starting position. Repeat 15 times.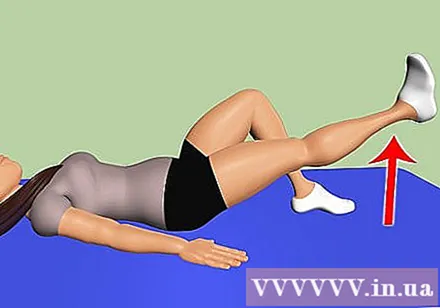
Do squats against the wall with the ball. Put your head, shoulders, and back up against the wall. Feet placed 90 cm from the wall. Place the ball behind your back and slowly lower yourself to a 45 degree angle. Hold this position for 10 seconds, then return to starting position. Repeat 10 times.
- This exercise is also great for the core muscles. Try raising your hands 90 degrees while in a squatting position and lowering your hands when returning to starting position.
Practice high steps. In a standing position, raise the injured leg at least 7.5 cm - 12.5 cm from the floor, with the other leg on the floor. Slowly alternate positions with each leg, doing these two movements 15 times.
- Once your knees are strong enough, you can try doing the step-steps like the ones you see in the gym. Experiment with different heights for maximum elongation.
Practice your knees. Wrap the elastic bandage around the ankle of the injured leg and tie it to the door at eye height to your feet. Face toward the door, slightly sagging knee of injured leg and tightening muscle. Hold this position while stretching your healthy leg back. Do these 2 moves 15 times.
- Alternatively, you could try stretching your knees with resistance. Tie a loop of elastic bandage and tie it to the door at knee height. Step the injured leg into the ring and bend the knee about 45 degrees, with the other leg lifted off the floor. Slowly straighten your legs and tighten your thigh muscles. Repeat this exercise 15 times.
Part 4 of 4: Understand your condition
Recognize the symptoms. A meniscus tear is the most common knee injury. If you suspect that you have had a meniscus tear, watch for the following signs:
- A feeling of rattling in the knee. Rattles often appear during activities using the knee. This sound is normal if the knee doesn't move for a few minutes and then you try to bend the knee, but if you bend your knee many times and the clumping sound persists then this could be a symptom. find the knee has a problem.
- Swelling and stiffness. Fluid present in joints helps the joints to move easily. When the meniscus tears, too much fluid builds up, causing the knee to swell. Swelling is often accompanied by stiffness. Joint stiffness is a condition in which the knee joints are difficult to move and is inability to move during knee-use activities.
- Pain. Swelling and stiffness are also associated with pain. Pain is evident when pressed against the knee or when moving the knee. You may not be able to bend your knee due to the pain. The knee looks locked and cannot move.
Look for a mild meniscus tear. In this case, you will experience moderate pain during the injury. Pain may be accompanied by mild swelling. In addition, tissues are gradually damaged.
- The throbbing pain can be relieved after 2-3 weeks of limited vigorous activity. Some movements like squatting, knee bends, heavy lifting, and twisting can cause symptoms to return.
Recognize a moderate meniscus tear. A person with moderate meniscus tears will experience a sharp pain in both sides and between the knee, especially when squatting or twisting. The inflammation may worsen in 2-3 days and harden the knee joint. The patient is still able to walk, but knee flexion is limited.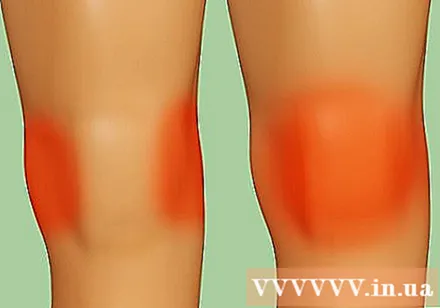
- Symptoms usually subside within 1-2 weeks, but can persist with the use of the knee. The pain can last for many years if the disease is not treated.
Know if you have a severe meniscus tear. This is often accompanied by more severe pain and sudden swelling and stiffness. You may experience throbbing pain, pounding pain, and severe pain. Inflammation can be seen clearly in 2-3 days. Some torn pieces of the meniscus can even move into the joint joints.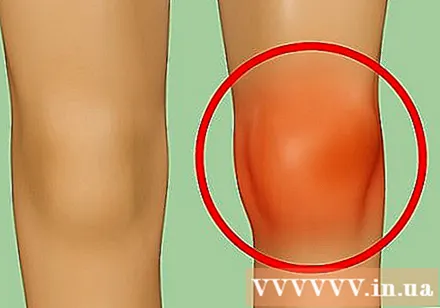
- These symptoms can lead to knee instability or inability to walk normally as well as knee straightening. This, of course, requires medical treatment.
Learn how to diagnose. Your doctor will look at your medical record to assess the association between your current symptoms and previous damage to your knee. You will be examined and tested to evaluate the function of the knee such as: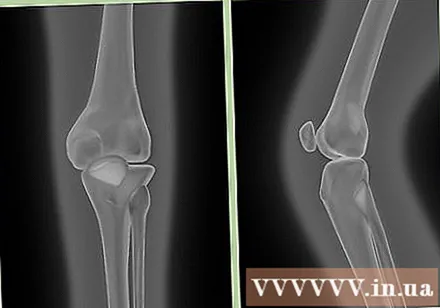
- Examination of the knee. Each knee is examined for pain, loss of stability, decreased range of motion, pain in certain positions, and unable to put weight on the sore leg.
- X-ray. This test is used to evaluate the knee bone to determine inflammation.
- Magnetic resonance imaging (MRI). Magnetic resonance tests are often ordered by an orthopedic doctor for confirmation. This test provides a clear picture of the location and severity of the meniscus tear as well as the surrounding ligaments, tendons and cartilage.
- Knee arthroscopy. The orthopedist will do an endoscopy to examine the inside of the knee joint by passing an instrument called an endoscope through a small incision. This device has a camera and light system for direct observation or treatment of meniscus tears.
If the patient has pain, the doctor can numb the knee. Some patients may experience pain when their doctor performs certain exams and tests. In these cases, your doctor may recommend a knee drain or local anesthetic injection. This procedure will not cause additional pain.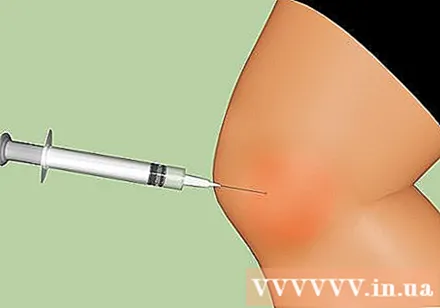
- The above procedures can help relieve pain and facilitate examination. However, if none of the above works, the assessment may be postponed until the inflammation or pain subsides.
Advice
- Excessive twisting or turning can risk the meniscus tearing. Both contact sports or vigorous knee-intensive sports should be avoided.
- Weak bones are part of the aging process. For the elderly, knee problems are common.