Author:
Louise Ward
Date Of Creation:
6 February 2021
Update Date:
1 July 2024

Content
Fungus is a fungal disease caused on the outermost layer of skin, which causes red, contagious, scaly bumps. Most people get ringworm at least once in their lifetime. Fungi (Fungi) thrive in warm and humid places, such as between the legs. Foot fungus can be treated at home with over-the-counter (topical) antifungals as well as taking measures to prevent recurrence. However, after cured treatment, the disease can still recur if the fungus has favorable conditions to multiply and grow.
Steps
Part 1 of 3: Diagnosis of Foot fungus
Determine if you are at risk for athlete's foot. If you come into contact with a contaminated surface, which is a favorable environment for fungus to grow, you may develop ringworm. Contaminated surfaces such as swimming pools, changing rooms, or bathrooms, where you go barefoot where someone has been in contact with foot fungus. Some cases can also cause a fungal infection of your feet or toes such as:
- Wear shoes that are too tight to have air circulation.
- Wear plastic insoles.
- Let feet get wet or damp for a long time.
- The feet are often wet.
- Injury to the skin or toenails.
Know the symptoms of fungal foot disease. The most common symptom is skin discomfort caused by fungus. There are three types of foot fungus, which may have slightly different symptoms than the ones you already know. Symptoms can be mild, moderate, or even severe. Some symptoms, such as itching, may get worse as soon as you remove your socks or shoes. Symptoms of athlete's foot include:- Itching and discomfort.
- Peeling or scaly skin.
- Cracked skin.
- Bleed.
- Pain in the affected area.
- The skin is pink or redder than the rest of the feet.

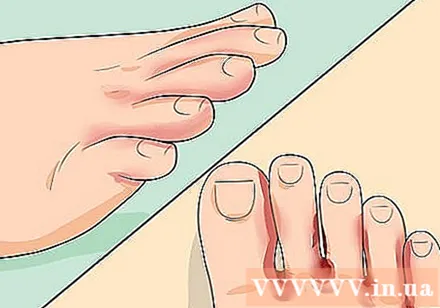
Check your feet carefully for signs of athlete's foot. Look at your feet in the light so you don't miss any sign. Pay special attention to areas between the legs and soles of the feet. If you see any red or dry flaky or scaly skin on your skin and are experiencing the above mentioned symptoms, you should begin treatment immediately.
Check for fungus in the toe. Toe fungus is a type of fungus that usually occurs between the fourth and little toes. Watch for symptoms of foot fungus in these areas such as scaly, flaky or cracked skin. Bacteria can also attack these areas of skin making the skin more infected.
Check for fungus on the soles of your feet. Fungi of the soles of the feet may start with mild swelling or cracking in the heels or areas of the soles of the feet. The disease can get worse, affecting the toenails, causing the toenails to swell, break or come off. Be sure to check for signs of discomfort or fungal infection of your toenails.
Check for blister-like fungus. This fungus can cause blisters on the feet. Blisters usually appear on the soles of the feet. Bacterial infection can co-exist with a fungal blister-skin infection, making symptoms worse.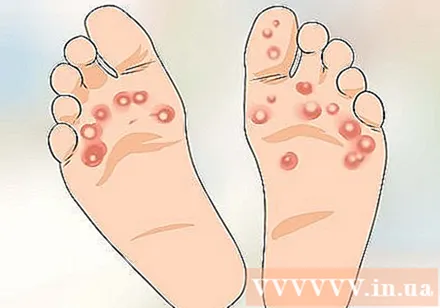
Understand that athlete's foot can spread to other parts of the body. Fungus is an opportunistic disease that can occur anywhere if conditions permit. Always wash your hands thoroughly after coming into contact with infected skin on your feet.
- It can spread to your hands, especially if you come into frequent contact with infected skin on the feet.
- Fungal foot and foot infections can spread to the toenails and nails. It is much more difficult to treat nail fungus than it is for fungus on the skin of the feet.
- Fungal foot dermatitis can develop into an itchy area in the groin and upper thighs when it infects the groin area. Be aware that the fungus that causes ringworm can be spread through towels or hands if you come into contact with the affected leg area and then spread to the groin area.
Go to doctor. A doctor can diagnose fungal foot skin disease by examining an infected area of the foot. They can look for fungal visual signs that are visible to the eyes. Or they may run some tests to confirm the diagnosis:
- Take a piece of skin from the infected skin area to see the cells under a microscope.
- Use a high-pressure light to check your feet for fungus.
- Submit a skin cell sample to the lab for more detailed testing.ref> http://www.mayoclinic.org/diseases-conditions/athletes-foot/basics/tests-diagnosis/con-20014892
Part 2 of 3: Treatment of Foot fungus
Choose an over-the-counter foot fungus. There are many over-the-counter antifungal medications available in creams, liquids, gels, oils, waxes or powders that can effectively treat athlete's foot. Some people take 1-2 weeks to cure, while others it can take up to 4-8 weeks to fully recover. Other quick treatment measures are more expensive but will shorten treatment time.
- Over-the-counter fungus medications usually have one of the following main ingredients: clotrimazole, miconazole, terbinafine or tolnaftate. Treatment usually lasts 1-8 weeks, depending on the type of treatment you choose.
Apply an antifungal. Wash your hands before handling the foot fungus. You should clean the area of the fungus before applying it directly to the redness and the surrounding area. Even if the rash is gone, the fungus may still be on your skin, so you still need to take medication.
- It is best to continue using a powder or cream antifungal for 1 to 2 weeks after all the fungus has been eliminated to make sure that the infection is not.
- Always use the medicine according to the instructions on the package, ampoule, or package insert that came with the medicine. Do not ignore dosage instructions, do not stop taking the drug before the scheduled treatment time - even if symptoms have disappeared.
- Do not remove peeling skin. You can damage the surrounding healthy skin and spread the pathogenic fungus.
Use Burow solution. This solution is used for a variety of skin conditions, usually without a prescription, and can be astringent and anti-fungal. It is especially useful for the treatment of blister-like fungus.
- Follow the directions, and soak your feet several times a day for at least 3 days. Once the blisters have tightened, you can switch to an antifungal medication for the affected area.
- You can also apply Burow solution to a cloth or gauze pad and apply to the affected area.
Make sure to keep your feet as dry as possible. Fungi thrive in warm and humid environments. Try to keep your feet dry all day.
- Change socks and shoes regularly to keep your feet dry. If socks are wet all the time, you should change to a new one. Use clean cotton socks. Synthetic-fiber socks do not absorb sweat as well as cotton.
- One trick is to put a desiccant bag (often found in a dry beef market) attached to the socks for the day. This trick may sound uncomfortable, but silica is extremely desiccant - that's why they come in bags of beef jerky.
- You can use a talc powder or an antifungal powder on the feet and inside of your shoes to help fight fungal infections.
- Wear open muzzle shoes or sandals often in the summer.
Clean your feet twice a day. Wash your feet with soap and water, and especially clean the legs, 2 times a day. Make sure your feet are completely dry after washing them and dry between them with a clean cloth.
Use tea tree oil or garlic. These natural remedies are also effective in treating athlete's foot if used regularly. This is because both tea tree oil and garlic oil contain antifungal compounds that are effective in treating fungal infections. While tea tree oil and garlic oil may help relieve the symptoms of athlete's foot, it is not a cure-all.
Take prescription medications. If you have a severe or persistent fungal infection, your doctor may prescribe a topical or oral antifungal medication for you. Some antifungal prescriptions can cause side effects. Ask your doctor about the medications they will prescribe for you.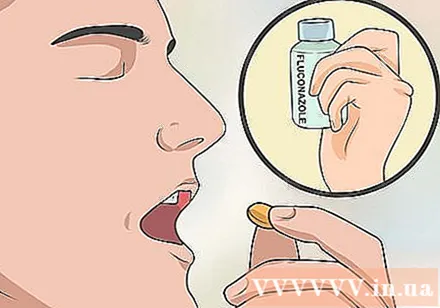
- Antifungal prescription medications may include the ingredients butenafine, clotrimazole or naftifine.
- Antifungal capsules may include ingredients such as fluconazole, itraconazole and terbinafine. It usually takes 2 to 8 weeks to take, depending on the medication you are prescribed.
Part 3 of 3: Prevention of Foot fungus
Wear flip-flops or flip flops when swimming in public pools or bathing. Since ringworm can be contagious, you need to create a layer of protection from the factors that can transmit the disease. Never walk barefoot in public places, especially in warm and humid places.
- Always dry your feet completely after bathing or swimming before putting on shoes.
Change shoes regularly. Let the shoes dry for at least 24 hours before returning to them. The fungus can lodge in your shoes, so you won't want to infect yourself again. To make sure your shoes don't become a factor, wear a different pair of shoes every day.
- Buy new shoes if necessary.
Actively use over-the-counter antifungal drugs. Whenever you feel you may have a fungal infection, immediately use a powder or cream antifungal. When you have to go out during a hot day or exercise, apply an extra antifungal layer to your feet if you are prone to fungal infections. If you go swimming and lose your flip flops, take the next step right away - dry your feet completely and apply powder to prevent infection.
Clean clothes, tools and shoes. Any item that comes into contact with the skin of an infected foot should be cleaned with bleach or other sanitizer. Items include nail tools, shoes, socks and anything that touches your feet. You probably never want to re-infect yourself after spending so much time on treatment.
- Use hot water and a shoe and clothing laundry detergent to kill foot fungus.
Wear slightly wider shoes. Wear shoes so tight that air cannot circulate in the shoe. The fungus is also easy to grow. You can also use sheep wool between your feet so they don't get snuggled together when you're wearing shoes. Wool can be found in pharmacies or pedicure centers. advertisement
Advice
- Dry your groin area before wiping your feet when you shower or swim. Put on socks before wearing underwear to prevent fungal infection of the groin area.
- Consult a healthcare professional for advice on the medication to use.
Warning
- Untreated yeast infection can spread to other areas of the skin or lead to infection.
- If your athlete's foot does not go away or gets worse, see your doctor or specialist.
- If you have diabetes and symptoms of ringworm, you should see your doctor right away.