Author:
Monica Porter
Date Of Creation:
20 March 2021
Update Date:
1 July 2024

Content
Dry gangrene is a fairly rare disease in which certain parts of the body dry out and turn black due to lack of blood circulation. In severe cases, skin and tissues may even flake off. Dry gangrene differs from other forms of gangrene in that it is not accompanied by an infection caused by a burn or other injury that causes a part of the body to be cut off blood supply and also without discharge or drainage. Dry gangrene usually affects the extremities, especially the hands and feet, but can also affect other organs such as limbs, muscles and even internal organs. People with potentially at-risk conditions such as diabetes, peripheral artery disease or autoimmune diseases have a high risk of developing dry gangrene.
Steps
Part 1 of 3: Lifestyle changes

Stop smoking. Breaking out this habit can help prevent gangrene and progression of the disease, as smoking contributes to the blockage of blood circulation. When the blood stops circulating, tissues die and cause gangrene. Anything that cuts off blood circulation should be avoided, and of course smoking included.- The active ingredient nicotine in tobacco is the culprit that has a strong impact on the blood circulation. It constricts the blood vessels, leading to less blood flow. When the blood flow to an organ becomes less, the oxygen supply is less. A chronic lack of oxygen in the tissues causes necrosis (tissue death) and can lead to gangrene.
- Smoking is also linked to a blood vessel disorder, a cause of the narrowing and stiffening of the blood vessels.
- It is advisable to quit smoking gradually rather than abruptly, because abruptly quitting can lead to severe withdrawal symptoms, making it difficult to keep up with your determination to quit.
- Get help from your doctor in quitting smoking.

Adjust your diet. In gangrene, tissues and muscles are damaged by poor blood circulation. Therefore, patients are encouraged to eat foods rich in protein and high in calories to aid in the healing of tissues and muscles. Protein can also help rebuild damaged muscles, and nutritious foods (instead of empty calories like fast foods) energize the body to help carry out its functions.- Foods that are high in protein but low in fat, thus helping to prevent arterial blockages, include turkey, fish, cheese, lean pork, lean beef, tofu, beans, eggs and peanuts. Avoid foods high in fat such as red meat, butter, lard, hard cheeses, cakes, crackers, and fried foods. Instead you should incorporate more green vegetables into the menu.
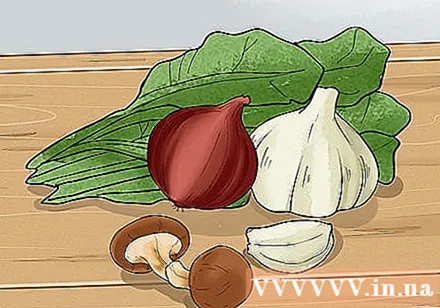
Include foods rich in germanium and other antioxidants in your diet. Germanium is an antioxidant, and although the evidence is still oral, it is thought to help increase oxygen activity in the body. It also boosts the immune system and has anti-cancer properties.- Foods high in germanium include: garlic, onions, shiitakes, whole wheat flour, bran, ginseng, green vegetables and aloe vera.
- Due to the lack of solid scientific evidence for the effects of germanium on the transport of oxygen to tissues in the case of gangrene, there are currently no dosing recommendations for germanium. You can consult your doctor to see if a germanium supplement is helpful for your particular situation.
Be wary of your sugar intake. Although monitoring your sugar intake is essential for everyone, it is especially important in cases of diabetes. People with diabetes need to limit their sugar intake to keep blood sugar at the recommended range based on the time of meals, exercise schedule and time of day. People with diabetes should also regularly check the extremities for any signs of cuts, swelling, redness or infection.
- People with diabetic neuropathy should check their body daily for any symptoms such as numbness in arms, legs, fingers and toes, as these are signs of poor blood circulation. High sugar levels are also linked to high blood pressure and have a negative effect on normal blood flow in the blood vessels.
Limit your alcohol intake. Drinking too much alcohol compared to the recommended daily limit can cause blood pressure to spike, and cholesterol in the blood will also rise, causing blood clots.
- The amount of alcohol you drink per day is limited to 1 drink for women and 2 for men. Note, 1 glass is counted as one beer (350 ml), one glass of wine (150 ml) or mixed wine containing 45 ml of spirits.
Do exercise. While the effects of exercise on the progression and treatment of gangrene are not known exactly, it can help relieve some of the underlying diseases that cause gangrene.One study found that a 30-40 minute treadmill exercise program, three to four days a week, could help with limp symptoms, or painful leg cramps due to leg muscles. not getting enough blood.
- Consider setting up a home workout regimen with medium intensity exercises that can be done on the treadmill or walk around the neighborhood as outlined above. Keep a walking journal to keep track of your exercise and any symptoms or feelings you may be experiencing. Consult with your doctor before entering any exercise regimen for heart disease or pre-existing conditions.
Do exercises for limbs. If you can't move easily, you can practice exercises that increase your passive range. These exercises require someone to help move the joints to the fullest extent of your range of motion to prevent muscle spasm (permanent contractile muscles and joints) and improve blood supply. special parts of the body. These exercises include:
- Head exercises such as head turning, head tilt or head bend, chin to chest touching.
- Shoulder and elbow exercises, such as elbow bends, up and down or back and forth movements.
- Forearm and wrist exercises, such as wrist flexing, hand rotation and up and down movements.
- Hand and finger exercises such as finger flexing, finger stretching and finger rotation.
- Hips and knee exercises such as hip and knee flexion, leg back and forth movement and leg rotation.
- Foot exercises such as flexing, turning and ankle movements, toe flexing and toe stretching.
Take care of all injuries. Wounds and burns need immediate treatment as they can progress to wounds that cannot be healed, especially in diabetics. Whether you already have gangrene or are worried that the disease might develop, it is most important to keep the wound clean and protected as your body attempts to build a network of capillaries underneath the scab. Please follow these steps:
- Wash the wound with a solution of betadine or hydrogen peroxide and apply an antibiotic prescribed by your doctor.
- After washing it thoroughly, cover the wound with a sterile gauze bandage and clean cotton socks. Cotton can absorb moisture away from the wound and also helps to better air circulation, thereby assisting in the healing process.
Apply cayenne, garlic, honey, or onions to the affected area. Caynnen tincture, a liquid extract of cayenne peppers, can help relieve pain, enhance circulatory function, and reduce the risk of infection. Caynnene alcohol is available in pharmacies. Apply to the affected area two or three times a day or as advised by your doctor.
- You can also crush a few cloves of garlic and apply it directly to the wound. This was the standard treatment during World War I and II, thanks to garlic that has antimicrobial properties that help prevent or treat infections in the gangrene and its antiplatelet properties help dissolve blood clots. East causes gangrene.
- Alternatively, you can cover the wound with sliced onions. Cut an onion into slices and cover the affected area with a clean cloth. Let it sit for 5 - 10 minutes, doing it several times a day. This can improve circulation to the affected area.
- Try applying honey to the wound. Honey has long been used to treat burns, wounds and boils. Research is still ongoing, but honey has been shown to have antibacterial properties. Be sure to use sterile and tested honey, though. Spread honey on a cloth or bandage and apply it directly to the wound, or you can buy a gauze impregnated with honey.
Part 2 of 3: Medical treatment
Surgery to remove dead tissue. Surgery is indicated when gangrene is severe and requires removal of dead tissue. Usually the amount of dead tissue needed to remove depends on the amount of blood reaching the affected area and the location of the wound. This is the standard treatment for dry gangrene. These surgeries include:
- Filter out necrotic skin This surgery is aimed at removing dead tissue caused by gangrene. Sometimes necrotic skin can be replaced with new, healthy skin tissue (also called a skin graft).
- Cut If all tissue is dead and medications or other surgeries fail, the limbs or other organs may be removed to prevent gangrene from spreading around and other parts of the body. This surgery is indicated when surgery to remove the necrotic skin is ineffective. Note that, unless it is life-threatening, a decision to have a surgical resection can only be made after you have been thoroughly consulted by a doctor and have all the information needed to make the right choice.
Consider using maggot therapy. As an alternative to surgery, maggot therapy similarly works to remove dead tissue. With this non-surgical therapy, fly larvae are placed into the gangrene area and covered with a gauze bandage. The maggots will eat dead tissue and, luckily, they won't touch healthy tissue. Maggots are also effective against infections because they secrete substances that kill bacteria.
- Some studies suggest that maggot therapy may be more effective than surgical removal of necrotic skin. However, many people are too scared or hesitant to try this therapy because they cannot stand the "fear".
Use high-pressure oxygen therapy. This is an alternative therapy in which the patient is placed in a special chamber filled with compressed air. Next you will be covered with a hood to breathe pure oxygen. It may sound a bit frightening, but this therapy is an effective way to increase the level of oxygen in the blood, supply oxygen to damaged areas and improve blood transport and flow. Blood reaches the gangrene area even in patients with poor blood flow.
- Once the damaged areas have been supplied with enough oxygen, the risk of amputation is reduced. Research has confirmed the effectiveness of high-pressure oxygen therapy in the treatment of diabetic foot gangrene, thereby reducing the risk of amputation.
- You need to check with your doctor about whether high pressure oxygen therapy is right for you.
Restore blood circulation by surgery. The main types of surgery to restore blood circulation are bypass surgery and angioplasty. Studies have shown that these two surgeries are equally effective in restoring blood circulation and reducing the risk of amputation. Angioplasty, however, has a faster recovery time, and bypass surgery may be more effective in the long run. Check with your doctor about which surgery is best for your specific medical history and condition.
- Bridge surgery With this surgery, the surgeon will redirect blood flow by “bridging” through the blockage. A pharmaceutical graft technique is used to connect a vein to the healthy part of one of the arteries.
- Circuit forming During an angioplasty procedure, a tiny balloon is placed in a very narrow or blocked artery. Then this small balloon will swell and widen the blood vessels. In some cases, the surgeon may also insert a metal tube, called a stent, into the artery to dilate the artery.
Use a blood clot-reducing medication. Your doctor may also prescribe anticoagulants to reduce the formation of blood clots, thereby improving blood flow. Warfarin is an anticoagulant drug, usually taken by mouth in pill form (2 to 5 mg) once a day (at the same time). Warfarin inhibits and resists vitamin K, thereby slowing blood clotting. As a result, the blood will dilute and circulate better.
- Remember that anticoagulants will make it easier for you to bleed. You may not be able to take anticoagulants if you have a history of blood problems (such as a blood clotting disorder), cancer, kidney or liver problems, heart disease or high blood pressure, and others. Always consult your doctor before taking any medications that affect blood circulation and blood clotting.
Treat infections. Antibiotics are often prescribed to patients with gangrene caused by infection or those at risk of infection due to open wounds or wounds that are difficult to heal.Usually, the doctor prescribes an antibiotic to a patient with gangrene after tissue removal surgery to fight infection of the remaining tissue. Commonly prescribed prescription drugs include:
- Penicillin G This is an antibiotic that has long been used to treat gangrene. The usual dose is 10-24 million units (every six or eight hours) by intravenous or intramuscular injection. Penicillin G has a bacteriostatic effect, which means inhibiting or preventing bacteria from multiplying and growing. Usually, severe infections or patients undergoing surgery are given an injection because higher doses can be used by injection and to act on the affected area faster than orally. Currently doctors often prescribe a combination of penicillin and clindamycin, a protein inhibitor.
- Clindamycin This drug is used to treat and prevent infection by killing bacteria by blocking the production of protein in bacteria. Bacteria cannot survive without these proteins. The usual dose is 300-600 mg orally every six to eight hours, or 1.2 grams intravenously twice daily.
Start the care process. Usually you will be looked after by the patient care program after surgery. This is a therapy needed to restore the normal function of your legs, hands, toes, or fingers. Part of rehabilitation therapy includes isotonic exercises to maintain function of the affected area. These exercises help the joints connect with the muscles in the arms and legs. Isotonic exercises include:
- Walk fast or slow
- Cycling
- Dance
- Skipping
Part 3 of 3: Understanding the disease
Know the cause of gangrene. Gangrene can occur due to the following factors:
- Diabetes This disease interferes with blood circulation, especially in the lower extremities, and can lead to incurable wounds.
- Vascular diseases Vascular diseases, such as peripheral artery disease (PAD), can decrease blood flow in the body. PAD, for example, occurs when the arteries narrow, mainly by atherosclerosis, hardening the arteries and blood vessels.
- Vasculitis Vasculitis refers to certain autoimmune diseases that cause inflammation in the blood vessels, such as the Raynaud's phenomenon. With these autoimmune diseases, the blood vessels leading to the fingers and feet are temporarily constricted (constriction of the vessels), constricting the vessels, or narrowing the blood vessels. Triggers for Raynaud's include exposure to cold temperatures and stress.
- Tobacco addiction - Tobacco can clog the arteries and thus impair blood circulation.
- External wounds Burns, accidents, wounds or incisions can damage certain cells in the body, leading to slower blood flow. If the wound is not properly treated and the main blood vessel is damaged or weakened, it will no longer be able to transport enough blood to surrounding tissues. This leads to a lack of oxygen supply to the body organs and death of surrounding tissues.
- Cold burns - Exposure to very cold temperatures can prevent normal blood circulation. Cold burns can occur in icy weather in as little as 15 minutes. Cold burns usually work on the fingers and toes. To prevent cold burns, you can wear properly lined gloves and shoes to keep warm and resist moisture.
- Infection Untreated bacterial infection can spread to damaged tissues, causing tissue death and gangrene.
Understand the different types of gangrene. Gangrene can be classified into different types, including:
- Dry gangrene This form of gangrene is characterized by dry and necrotic skin with brown to bluish purple to black in color. This usually progresses slowly and eventually the tissue falls off. Dry gangrene can become wet gangrene if infected.
- Wet gangrene - Common features of wet gangrene are swelling, blistering and wet tissue due to discharge. Wet gangrene develops after an infection of the damaged tissue. This form of gangrene requires urgent treatment because it is rapidly growing and can be very dangerous.
- Breathing gangrene This form of gangrene is a subtype of wet gangrene. In this form of gangrene, the skin surface of the damaged part at first appears normal, but becomes pale and turns gray to reddish as the disease progresses. The blisters on the skin will become more visible and click sounds when pressed. This condition is caused by infection clostridium perfringens, a gas-producing bacteria that causes tissue death by vapor.
- Gangrene of the face - This is a form of gangrene that usually progresses rapidly, mainly occurs in the mouth and face. This form of the disease usually occurs in malnourished children and lives in unsanitary conditions.
- Organ gangrene This form of gangrene occurs when blood flow to internal organs such as the intestines, gallbladder or appendix is blocked. The illness often causes fever and severe pain, which can be fatal if left untreated.
- The Fournier Corruption This form of gangrene is very rare and involves the genitals and urinary tract. The disease occurs more often in men than in women.
- Meleney gangrene - This is an uncommon form of gangrene that occurs after surgery, with damaged and painful skin that occurs within one to two weeks after surgery. The wound is painful and itchy.
Know the symptoms of dry gangrene. Dry gangrene is a serious illness that requires urgent treatment. Anyone with the following symptoms should see a doctor immediately to avoid complications:
- The affected area is numb and cold, and the skin is atrophy
- Limping or cramps (such as condition in the legs when walking)
- A "needle-stick" sensation, numbness or tingling
- The affected area becomes discolored (it may be red, pale, purple and gradually turn black if left untreated)
- The affected area is dry
- Pain
- Septic shock (low blood pressure, possible fever, confusion, dizziness, shortness of breath). Septic shock is considered a critical condition and requires immediate medical attention. This is rare in gangrene, but it can also happen if not treated properly.
Seek medical emergency. This is not a disease that can be delayed. You may have to amputate your limbs or other body parts if not treated quickly. See a doctor as soon as possible for treatment as soon as possible.
- Note that some people feel no pain when they have dry gangrene, so they don't see a doctor until the limbs have turned black. Be cautious and notify your doctor as soon as you notice any of the symptoms listed above. Don't let it go until the situation gets serious.
- While home remedies are also good, they are often not effective enough in treating dry gangrene. You need early treatment for symptoms to improve faster.
Warning
- You should consult your doctor as soon as you recognize any of these symptoms to ensure timely diagnosis and treatment.
- If you are at risk of developing dry gangrene, especially if you have diabetes or peripheral artery disease, you should learn about dry gangrene and carefully monitor any symptoms. See your doctor regularly to stay informed about risks and symptoms.