Author:
John Stephens
Date Of Creation:
22 January 2021
Update Date:
1 July 2024

Content
Chronic indigestion (or gastrointestinal disturbances) is a condition that involves discomfort in the stomach that lasts more than 7 days a month. Chronic indigestion symptoms can get worse, come and go, or last for a long, difficult time. The most common symptom is a burning pain or discomfort in the upper abdomen. Other possible symptoms include "abdominal pain", feeling full or bloated, belching, nausea, and vomiting. Fortunately, there are ways to help relieve the symptoms of chronic indigestion.
Steps
Part 1 of 4: Identify and treat the cause
Recognize the symptoms of chronic indigestion. Although there are many different signs, there are a few common symptoms that alert you to a problem that needs to be addressed. The most common symptoms include:
- A feeling of bloating or bloating
- Nausea, even vomiting
- Excessive heartburn and belching (above the "normal" level)
- Reflux food from the stomach into the esophagus.
- Throbbing pain or severe pain in the stomach

Understand the main causes of chronic indigestion. Indigestion is not a disease but a symptom of an underlying problem in the digestive system. It is important to identify the underlying cause of indigestion. As its name implies, indigestion is often related to eating and drinking. Overeating and too fast, drinking too much alcohol, and consuming foods that are hard to digest can all cause stomach upset. On the other hand, chronic indigestion can be linked to many other serious problems including:- Functional dyspepsia (no obvious clinical abnormality)
- Stress
- Fat
- Smoking
- Pregnant
- Medications (such as NSAIDs, nonsteroidal anti-inflammatory drugs, aspirin)
- Irritable bowel syndrome (IBS)
- Gastroesophageal reflux disease (GERD)
- Gastroparesis (the stomach cannot digest food properly)
- Helicobacter pylori infection
- Stomach ulcers
- Stomach cancer

Cut or change medications. Sometimes, chronic indigestion is a side effect of long-term use, especially NSAIDs, including aspirin, naproxen (Aleve, Anaprox, Naprelan, Naprosyn), and ibuprofen (Motrin, Advil), along with many other drugs.- NSAIDs can cause intestinal problems and discomfort. Therefore, NSAIDs are not recommended for long-term use.
- Iron supplements are also difficult to digest, which can cause acid reflux, constipation, and upset stomach.
- Certain high blood pressure medications, anti-anxiety medications and antibiotics can cause heartburn, nausea and indigestion, among other side effects.
- If you suspect that your indigestion is caused by medication, you should consult your doctor about switching to another medication.

Take antacids recommended by your doctor to reduce indigestion during pregnancy. Not surprisingly, pregnancy is often associated with indigestion due to pressure from the growing fetus on the digestive system. Up to 8/10 pregnant women experience indigestion during pregnancy.- If the symptoms are mild and cause no significant pain, you can change some eating habits (see below). In addition, you can take over-the-counter antacids to reduce stomach acid production, or take Alginate to reduce indigestion caused by acid reflux (acid reflux from the stomach into the esophagus). In general, you should take antacids or Alginate only when symptoms appear (instead of daily). Read on to section 3 to learn more about some medicines.
- Although there are many concerns about taking medications during pregnancy, antacids or alginates are safe if you take the recommended dose. It's best to consult a doctor if in doubt.
Make dietary changes to reduce chronic indigestion caused by irritable bowel syndrome (IBS). Chronic indigestion is one of the most common symptoms of IBS - characterized by persistent abdominal pain, discomfort, bloating, and changes in bowel habits. The cause of IBS remains unclear and has not been discovered through any testing.
- The best treatment depends on the specific symptoms the patient is experiencing. However, making changes to the diet is often very effective in reducing symptoms.
Seek medical treatment for chronic indigestion for gastroesophageal reflux disease (GERD). GERD is caused by abnormal, persistent reflux of stomach acid into the esophagus. GERD indigestion can be treated with medications (see section 3), lifestyle changes (see section 2) or even surgery, depending on the severity of the indigestion.
- Seeing a doctor if you suspect gastroesophageal reflux is very important. If left untreated, in the long term, GERD can increase the risk of permanent damage and cancer of the esophagus.
Take medicine to relieve indigestion caused by stomach paralysis. Gastroparesis is a condition in which the stomach is unable to function properly due to nerve damage. Gastroparesis is often associated with diabetes.
- There is currently no definitive treatment for gastroparesis, but taking Metoclopramide - a dopamine receptor blocker - can help constrict the stomach, thereby preventing symptoms from peptic paralysis, including indigestion. . In this case, you need to see a specialist referred by a doctor.
Get treatment for indigestion caused by peptic ulcers or stomach cancer. Gastric ulcers and stomach cancer can only be accurately assessed and treated by a specialist. Proper treatment of stomach ulcers and cancer can help relieve indigestion.
- In the meantime, taking an antacid, Alginate or an H2 channel blocker (see section 3) may help relieve indigestion symptoms.
Part 2 of 4: Lifestyle changes
Change the serving size and number of meals. Overeating in one meal requires more peristalsis or synchronous movement of the digestive tract to metabolize food. This can aggravate irritation in the intestinal mucosa. So, you should switch to 6 small and regular meals: 3 meals (breakfast, lunch and dinner) and 3 snacks between meals. Besides, you should avoid eating 2-3 hours before going to bed.
- Try eating half the normal portion size for breakfast, lunch, and dinner. If you don't have frequent indigestion, this will help you feel full but not full after eating.
Avoid consuming foods and drinks that trigger indigestion. There are many foods that can irritate the intestines and stomach. Hot, greasy, and acidic foods are common culprits and should be cut down or eliminated entirely from your diet if you suspect they cause indigestion.
- Avoid greasy foods like fried foods, soft cheeses, nuts, red meats, and avocados.
- Avoid spicy foods like curries and hot sauces.
- Avoid tomatoes and ketchup and citrus fruits like grapefruit and oranges (as well as juices from these fruits).
- Avoid drinking carbonated drinks that cause an unstable stomach.
- Eliminate beverages that contain alcohol and caffeine.
- Try limiting a few foods at a time to narrow the range of foods that cause indigestion. When eliminating foods from your diet each day, watch for any changes and whether your indigestion improves.
Do not open your mouth while chewing. Chewing while opening your mouth or talking can cause you to swallow air, leading to bloating.
Review your posture. Do not lie down or curl up after eating. Along with gravity, lying or bending can cause the backflow of food from the stomach into the esophagus. Likewise, you should avoid dressing or wearing a belt that is too tight to avoid putting pressure on your stomach.
- After eating, wait at least an hour before you can lie down or participate in activities that involve bending. If you cannot not lie down, you can raise your head at an angle of 30-45 degrees to help the digestive system perform the function of breaking down food more easily.
Quit smoking. Consider quitting smoking if you have indigestion. The nicotine in tobacco can relax the muscles in the lower esophagus, making it easier for stomach acids to reflux. Besides, nicotine is also a powerful vasoconstrictor, which can cause atrophy of the intestinal mucosa (excess inflammation of stomach acid). In other words, smoking cigarettes can worsen stomach cramps.
- Quitting smoking also has other health benefits besides helping to reduce indigestion, including a reduced risk of lung cancer and other cancers, heart disease and stroke.
Cut back on alcohol and caffeine. These two substances can cause indigestion and especially heartburn by opening the sphincter of the esophagus, causing stomach acids to return. You may not have a problem drinking just one glass, but effects can occur if you frequently combine a drink with indigestible foods (e.g. drink a morning cup of coffee, a glass of wine with a coffee soup. sour at dinner, then eat oranges again).
- Avoid coffee, tea, soda and other caffeinated beverages. You don't need to avoid it completely, you should limit it. It's best to drink only 1-2 small cups of coffee (90-120 ml) per day.
Weight loss. People who are overweight or obese are more likely to develop indigestion due to the great pressure on the abdomen. Therefore, you should actively lose weight to see if indigestion lessens.
- Try to eat healthy and in moderation. Incorporate a variety of fruits, vegetables and whole grains into your diet. Limit foods high in acid until symptoms improve.
- Exercise regularly. Aim to do at least 30 minutes of moderate-intensity exercise at least 3 times per week. In addition, strength training should be strengthened to convert fat into muscle.
Part 3 of 4: Take medications
Take an antacid. Some easy-to-find antacids, such as Maalox, Rolaids and Tums, contain calcium, magnesium or aluminum, which can neutralize or counteract stomach acids to minimize acid corrosion. Antacids can be purchased over the counter at pharmacies.
- One of the most commonly prescribed antacids is Maalox. The recommended dose is 1-2 tablets, 4 times per day.
- It is helpful in treating common heartburn or indigestion but may not be strong enough in chronic indigestion.
Take an acid blocker. Excess stomach acid that backs up into the esophagus is one of the main causes of chronic indigestion. Acid blockers (or H2 blockers) help reduce stomach acid production, which in turn helps your stomach lower acidity so that when it backs up into the esophagus, it will cause less irritation.
- The most recommended H2 blockers are Ranitidine or Zantac, which can be bought over the counter or over the counter. Ranitidine is available as an oral tablet. In general, most H2 blockers are taken 30-60 minutes before eating (but only up to 2 times per day).
- Acid blockers don't work as quickly as antacids, but the effect is longer.In fact, acid blockers can last for hours and are used as the best preventative approach.
Take proton pump inhibitors (PPIs). PPIs work by blocking a chemical system called the hydrogen-potassium adenosine triphosphatase enzyme system, which produces stomach acids. If the level of stomach acid is low, the abdominal pain caused by chronic indigestion will decrease.
- Doctors recommend using PPIs when acid-blocking medications don't last long or when you have esophageal problems caused by gastroesophageal reflux disease.
- Prilosec is a PPI that is available in an over-the-counter drug form, while others such as Aciphex, Nexium, Prevacid, Protonix, and Prilosec are more potent that require a prescription from a doctor.
Take Alginate. Alginate drugs like Gaviscon (over-the-counter drugs) create a foam barrier that floats on the surface of food in the stomach, preventing stomach acids from backing up into the esophagus. Thanks to its ability to create a barrier between the stomach and esophagus, Alginate is especially helpful in reducing acid reflux and heartburn.
- Alginate works faster than H2 blockers and is more effective than antacids. The drug comes in liquid and oral tablet form for you to choose from.
- Alginate should be taken when symptoms appear, not before eating, as food travels through the esophagus, which can break down the barrier and make it less effective.
Try Reglan. Reglan (or Metoclopramide) helps to increase the spasm of the digestive tract, helping to move food through the digestive system and into the intestines. The increased rate of digestion helps reduce heartburn.
- Reglan should only be used as a short-term treatment drug and only when these drugs are ineffective. Do not take Reglan for more than 12 weeks.
- You will need a prescription from your doctor to buy Reglan. The drug comes in pill or liquid form, usually taken 30 minutes before meals and at bedtime.
Use antidepressants for pain relief. Nonsteroidal anti-inflammatory drugs (NSAIDs) are not recommended for patients with chronic indigestion to relieve pain because they can irritate the intestinal wall and make the illness worse. Instead, antidepressants will be prescribed to help relieve pain. Antidepressants aid in pain relief by reducing the ability of nerve cells to re-absorb brain chemicals such as serotonin and noradrenaline. These chemicals accumulate outside the cells if not reabsorbed, helping to inhibit pain signals reaching the spinal cord.
- The drug Amitriptyline is often prescribed for this purpose. The therapeutic dose is 10-25 mg per day, gradually increasing by 10-25 mg per week.
- Always consult your doctor about taking antidepressants for pain relief.
Part 4 of 4: Understanding the diagnostic process
Go to the doctor. If you suspect that you have chronic indigestion, you should see your doctor for help with treatment. The American Gastroenterology Association recommends seeing a doctor if you have any of the following symptoms:
- You have indigestion more than 3 times per week.
- You often have indigestion, more than 4 times a year.
- You use over-the-counter antacids and other medications for a few months or longer.
- Neither effort to make changes to lifestyle or to take medication will help with indigestion.
- Note if you have chest pain, you should see a doctor immediately or go to the emergency room because it could be a sign of a heart attack mistaken for heartburn or indigestion.
Get a blood test. Your doctor may take a blood sample from you to determine the potential cause of indigestion. Common blood tests that can help diagnose digestive disorders include a CBC test (a whole blood test), which measures the amount of red blood cells, white blood cells, and platelets in the blood; ESR test (blood sedimentation rate test); or CRP (C-reactive protein test), which is a test that assesses inflammation in the body. Blood tests can be used to diagnose and monitor diseases like irritable bowel syndrome (IBS), H. pylori, Celiac's disease, Crohn's disease and many others.
- A blood sample is taken from a vein using a sterile needle and syringe. The blood sample is then placed in a sterile tube and tested in the laboratory.
Endoscopic reception. In some cases, especially persistent indigestion, your doctor may refer you to a specialist in gastrointestinal and liver health. A specialist can perform an endoscopy, a procedure that looks inside the esophagus to see if acid reflux damages the esophageal lining.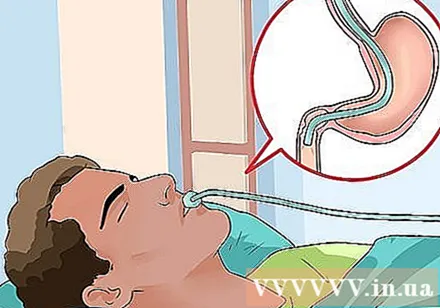
- During the colonoscopy, a medical device is inserted into the colon and monitored by a small camera with a light tube at the tip. This procedure can be done in one of two ways: colonoscopy or laparoscopy.
- During the colonoscopy, a flexible tube is gently inserted into the anal opening, allowing direct observation and examination of the colon (large intestine) and terminal ileum (end of the small intestine).
- During a laparoscopy, a flexible tube is inserted through the mouth, down the esophagus, through the stomach, and to the duodenum (the first part of the small intestine). Usually, your doctor will ask you to keep an empty stomach, ie not to eat or drink for about 6 hours before the procedure.
- During the colonoscopy, your doctor may also take a small tissue sample for testing.
Receive radiographs. Your doctor may recommend this method if you have symptoms of stomach pain, rectal bleeding, and unusual bowel movements (diarrhea or constipation). An x-ray is an X-ray test that can help show an abnormality in the colon. During this test, a liquid containing barium metal is inserted into the rectum. Barium will coat the colon lining to make it easier to see the colon on x-rays.
- Before receiving the test, you may have to "empty" the colon because what's left will be considered abnormal when it comes to the X-ray test. Your doctor may ask you to eat little or no food before midnight and take a laxative to clear the colon. In some cases, your doctor may ask you to follow a special diet before the day of the test (e.g. don't eat solid foods, only drink liquids like water, broth, and black coffee). A week or two before your test, you should ask your doctor if you should stop taking any medications (if any).
- In general, the x-ray test will be slightly uncomfortable but will not cause significant side effects. If present, side effects may be white stools (from barium) or slight constipation. In that case, your doctor may recommend a laxative.