Author:
Charles Brown
Date Of Creation:
3 February 2021
Update Date:
2 July 2024

Content
- To step
- Part 1 of 3: Understanding the condition
- Part 2 of 3: Treating impetigo
- Part 3 of 3: Limiting risk factors
- Tips
Impetigo or impetigo is a common superficial bacterial skin infection most common in children. The infection is very contagious and is easily spread in places where people are close together, such as schools and childcare centers. Because impetigo is spread through skin-to-skin contact, the condition is also common in people who play contact sports, such as wrestling. This rash can get more serious, so it's best to get it treated as soon as possible.
To step
Part 1 of 3: Understanding the condition
 Watch for red blisters. The most common type of impetigo is non-bullous impetigo, where tiny blisters form on the skin that eventually turn into red blisters. These blisters are filled with a yellow or honey-colored liquid. After a few days, these blisters burst and pus flows out for several days.
Watch for red blisters. The most common type of impetigo is non-bullous impetigo, where tiny blisters form on the skin that eventually turn into red blisters. These blisters are filled with a yellow or honey-colored liquid. After a few days, these blisters burst and pus flows out for several days. - After a few days, the blisters will turn into brownish, crusted patches.
- The blisters are usually around the mouth or nose, but they can also be on other parts of the body, such as on the arms and hands.
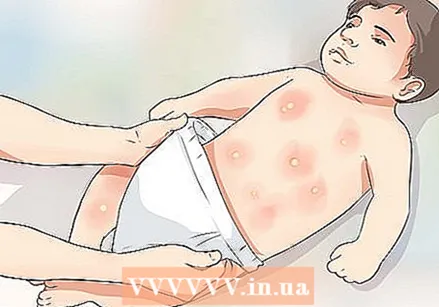 Look for larger blisters on the body. Bullous impetigo is a less common form of impetigo and is usually caused by the disease S. aureusbacteria. This bacteria causes larger blisters to form that are less likely to pop.
Look for larger blisters on the body. Bullous impetigo is a less common form of impetigo and is usually caused by the disease S. aureusbacteria. This bacteria causes larger blisters to form that are less likely to pop. - Bullous impetigo blisters may be on the chest and stomach, and in young children and babies, the area covered by their diaper.
 Check the legs. A third, more serious form of impetigo is ecthyma, which is usually caused by the disease streptococcal bacteria. The infection can also be caused by the staphylococcal bacteria. Usually this form of impetigo occurs first on the legs.
Check the legs. A third, more serious form of impetigo is ecthyma, which is usually caused by the disease streptococcal bacteria. The infection can also be caused by the staphylococcal bacteria. Usually this form of impetigo occurs first on the legs. - Ecthyma is sometimes referred to as "deep impetigo" because the symptoms are similar to other types of impetigo but appear deeper into the skin.
- Look for small blisters with a red border around them. These blisters are often filled with pus and may appear to be very deep in the skin. After the blisters have burst, you will see sores with thick, brownish and black crusts. This type of impetigo is much more painful than the other types.
- The ulcers caused by the infection appear along the edges as if they were "punched out", and the surrounding skin is often red and callused. Unlike the blisters, these sores will not heal or go away on their own.
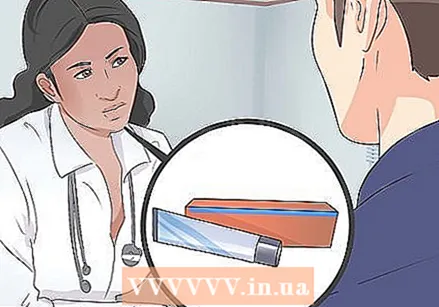
 Go to the doctor. If you think you have impetigo or your child has the condition, it is best to see a doctor. Your doctor can help determine that the rash you or your child has is actually impetigo. He or she can also prescribe the best medicines for you.
Go to the doctor. If you think you have impetigo or your child has the condition, it is best to see a doctor. Your doctor can help determine that the rash you or your child has is actually impetigo. He or she can also prescribe the best medicines for you.  Don't touch the rash. The rash is very contagious, so try to avoid touching the rash as much as possible. If you do touch the rash, wash your hands with antibacterial soap.
Don't touch the rash. The rash is very contagious, so try to avoid touching the rash as much as possible. If you do touch the rash, wash your hands with antibacterial soap. - This rash is often caused by various staph bacteria, which is why the infection is so contagious. The rash can also be caused by strep bacteria and is therefore contagious.
Part 2 of 3: Treating impetigo
 Soak the area to remove crusts. To make sure you can apply medication to the area, you may need to remove the crusts on the rash first. Hold a warm, wet washcloth against the area for a few minutes or soak the area in warm water to soften the scabs. When you're done, gently rub the area with a wet washcloth and soap and rinse your skin with water.
Soak the area to remove crusts. To make sure you can apply medication to the area, you may need to remove the crusts on the rash first. Hold a warm, wet washcloth against the area for a few minutes or soak the area in warm water to soften the scabs. When you're done, gently rub the area with a wet washcloth and soap and rinse your skin with water. - Don't let other people use the washcloth as it can spread the rash.
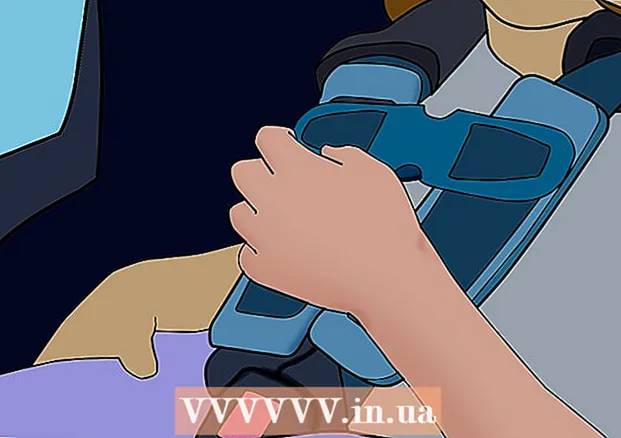
 Apply an antibiotic ointment. The impetigo is usually treated first with an antibiotic ointment and your doctor will prescribe the best ointment for your rash. Put on gloves or a finger condom before applying the ointment. Rub the ointment on the affected area.
Apply an antibiotic ointment. The impetigo is usually treated first with an antibiotic ointment and your doctor will prescribe the best ointment for your rash. Put on gloves or a finger condom before applying the ointment. Rub the ointment on the affected area. - If you don't have gloves, make sure to wash your hands thoroughly after applying the ointment.
- Your doctor can prescribe a topical antibiotic, such as mupirocin, retapamulin, or fusidic acid.
 Take an antibiotic in pill form if your doctor prescribes it for you. Impetus beard is often also treated with an oral antibiotic. Usually you have to take such a pill with some food once or twice a day. A cure lasts a maximum of 10 days.
Take an antibiotic in pill form if your doctor prescribes it for you. Impetus beard is often also treated with an oral antibiotic. Usually you have to take such a pill with some food once or twice a day. A cure lasts a maximum of 10 days. - Your doctor will likely prescribe a topical antibiotic first, unless the rash has spread to a large area of your skin or is not responding to medications. Resistance to oral antibiotics is becoming a problem, so doctors don't prescribe them unless absolutely necessary.
- Your doctor will likely prescribe an oral antibiotic such as diclocacillin or cephalexin. If you are allergic to penicillin, your doctor may prescribe clindamycin or erythromycin for you.
 Always use the medicine for as long as your doctor prescribes. Whether you have been prescribed pills or ointment, you must follow your doctor's instructions regarding the length of the course. Even if the rash appears to be diminishing, the bacteria still may not be completely gone. The infection can come back if you don't complete the course of medicine and it will be more serious.
Always use the medicine for as long as your doctor prescribes. Whether you have been prescribed pills or ointment, you must follow your doctor's instructions regarding the length of the course. Even if the rash appears to be diminishing, the bacteria still may not be completely gone. The infection can come back if you don't complete the course of medicine and it will be more serious. 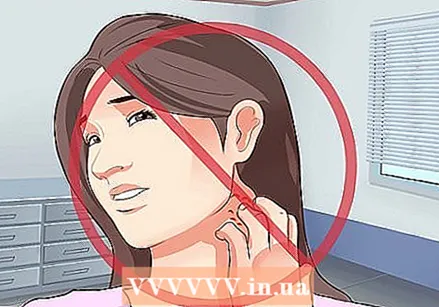 Do not scratch the blisters. It can be tempting to scratch the blisters, but it can also make the rash worse. You can spread the rash over your body or infect someone else with it.
Do not scratch the blisters. It can be tempting to scratch the blisters, but it can also make the rash worse. You can spread the rash over your body or infect someone else with it.  Know when to see your doctor again. If you still have a rash after 7 days and the patches don't seem to be healing, you should go back to your doctor. Your doctor may need to prescribe you a different antibiotic.
Know when to see your doctor again. If you still have a rash after 7 days and the patches don't seem to be healing, you should go back to your doctor. Your doctor may need to prescribe you a different antibiotic. - Your doctor can do some tests to see what type of bacteria is causing your impetigo. Certain types of bacteria, such as the MRSA (Meticillin-resistant Staphylococcus aureus) bacteria, have become very resistant to antibiotics.
 Know what complications can arise. This rash is usually not serious, but it can cause rare complications. Impetus beard caused by the streptococcal bacteria can cause a rare disease called post-infectious glomerulonephritis, which can affect the kidneys. If you have impetigo and your urine is dark in color, you should go back to your doctor to discuss the problem. Other complications include:
Know what complications can arise. This rash is usually not serious, but it can cause rare complications. Impetus beard caused by the streptococcal bacteria can cause a rare disease called post-infectious glomerulonephritis, which can affect the kidneys. If you have impetigo and your urine is dark in color, you should go back to your doctor to discuss the problem. Other complications include: - Scarring, especially from ecthyma
- Cellulitis, a serious infection affecting the tissue under the skin
- Guttate psoriasis, a non-contagious skin condition that causes scaly patches on the skin
- Scarlet fever, a rare bacterial infection that in some cases can be caused by impetigo caused by the streptococcal bacteria
- Sepsis, a bacterial blood infection that requires immediate medical attention
- Staphylococcal scalded skin syndrome (SSSS), a serious but rare skin infection caused by the staph bacteria
Part 3 of 3: Limiting risk factors
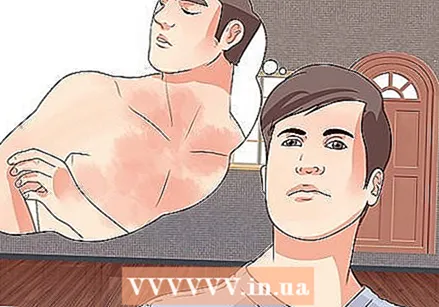
 Avoid other people. Especially during the first few days of the infection, it's a good idea to stay home from work or keep your child home from school or daycare. After starting the treatment you are contagious for a maximum of 2 days.
Avoid other people. Especially during the first few days of the infection, it's a good idea to stay home from work or keep your child home from school or daycare. After starting the treatment you are contagious for a maximum of 2 days. - Children can go back to school 24 hours after starting a course of antibiotics. Cover any blisters created by the impetigo with a waterproof bandage, and make sure your child doesn't take the bandage off at school.
 Wash your hands regularly. Also encourage children to wash their hands. Use clean, running water and soap to wash your hands regularly during your day. If you don't have soap available, use a hand sanitizer that contains at least 60% alcohol.
Wash your hands regularly. Also encourage children to wash their hands. Use clean, running water and soap to wash your hands regularly during your day. If you don't have soap available, use a hand sanitizer that contains at least 60% alcohol. - It is recommended to wash your hands for at least 20 seconds, or about as long as it takes to sing the song "Happy Birthday" twice in its entirety.
- Washing your hands well and regularly can help prevent the infection from spreading further. Touching the pus coming from the blisters can spread the rash. Snot can also spread the rash. Washing your hands regularly reduces the chance of spreading pus and mucus.
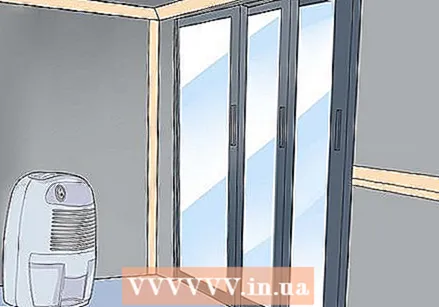 Dry your house well. Impetus beard can spread more easily in a wet and damp environment. The air conditioning already ensures that the air in your house becomes slightly less humid, but if the weather is humid and humid, you better buy a dehumidifier for your house.
Dry your house well. Impetus beard can spread more easily in a wet and damp environment. The air conditioning already ensures that the air in your house becomes slightly less humid, but if the weather is humid and humid, you better buy a dehumidifier for your house.  Cover cuts and scrapes. The infection can most easily enter your body through a cut or scrape. If you or your loved one has a cut, make sure it is covered with a bandage or gauze to provide protection.
Cover cuts and scrapes. The infection can most easily enter your body through a cut or scrape. If you or your loved one has a cut, make sure it is covered with a bandage or gauze to provide protection.  Don't share your things with someone who has impetigo. Whether you have impetigo yourself or someone you know has the infection, make sure that the other person does not share their towels and clothes with other family members. You can easily spread the rash if the fabric of a garment rubs against the infected area.
Don't share your things with someone who has impetigo. Whether you have impetigo yourself or someone you know has the infection, make sure that the other person does not share their towels and clothes with other family members. You can easily spread the rash if the fabric of a garment rubs against the infected area. - Do not share razors and other personal care products with people who have impetigo.
- Wash the infected person's clothes and towels daily. Make sure to wash them separately. Use hot water when washing.
Tips
- Using an antibacterial soap when washing will help remove bacteria from your skin.