Author:
Roger Morrison
Date Of Creation:
3 September 2021
Update Date:
1 July 2024
Content
- To step
- Part 1 of 3: Recognizing the symptoms
- Part 2 of 3: Symptoms of a complicated fungal infection
- Part 3 of 3: Knowing the risk factors
- Tips
- Warnings
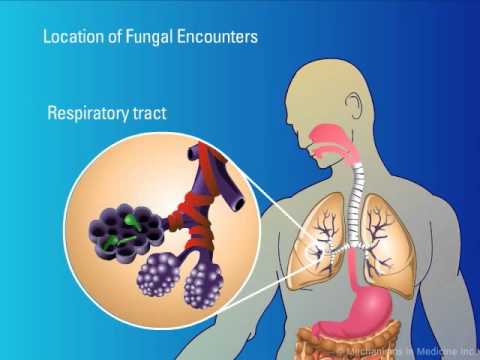
Yeast is a candida fungus that is normally found in the body alongside good bacteria and is usually kept in check by the immune system. Sometimes the balance between fungi and bacteria gets disrupted, which can lead to an overabundance of mold. Too much fungus causes what is known as a yeast infection, which can develop in various parts of the body, such as the skin, mouth, throat and, especially, the vagina. Don't be ashamed if you have a yeast infection; about 75% of women will have a fungal infection at least once in their life. A yeast infection can be very annoying, so it is important to diagnose the infection and treat it as soon as possible. In order to diagnose yeast infection, you need to know what symptoms to look out for.
To step
Part 1 of 3: Recognizing the symptoms
 Look for red spots. A fungal infection can develop in areas such as the crotch, the folds of the buttocks, between the breasts, in the mouth and intestines, between the toes and fingers, and in the navel. In general, fungus thrives in areas that are damp and have more folds and folds than other areas of the body.
Look for red spots. A fungal infection can develop in areas such as the crotch, the folds of the buttocks, between the breasts, in the mouth and intestines, between the toes and fingers, and in the navel. In general, fungus thrives in areas that are damp and have more folds and folds than other areas of the body. - The red spots may become thick and resemble small, red pimples. Try not to scratch these bumps; if you scratch and they open, you can spread the infection to other parts of your body.
- Know that babies regularly suffer from yeast infections, which cause them to develop diaper rashes that look like the red, tiny pimples described above. This mainly occurs in the folds of the skin, on the thighs and around the genitals, and is caused by the moisture in the dirty diaper when worn for too long.
 Watch for itching. The skin and areas of the body affected by the fungal infection will be itchy and very sensitive to the touch. It can also be irritated by clothing or other objects rubbing against the infected area.
Watch for itching. The skin and areas of the body affected by the fungal infection will be itchy and very sensitive to the touch. It can also be irritated by clothing or other objects rubbing against the infected area. - The infection may also cause a burning sensation on and around the area where the fungus is.
 Watch for symptoms specific to different types of fungal infections. There are three main types of fungal infections: vaginal infections, skin infections and throat infections. Each species has its own specific symptoms, in addition to the general symptoms listed above.
Watch for symptoms specific to different types of fungal infections. There are three main types of fungal infections: vaginal infections, skin infections and throat infections. Each species has its own specific symptoms, in addition to the general symptoms listed above. - Vaginal yeast infection: If you have a vaginal yeast infection, which is what most people mean when they say they have a yeast infection, you will notice that your vagina and vulva are red, swollen, irritated, and itchy. It can hurt or burn when you urinate or have sex. A vaginal yeast infection usually, but not always, is accompanied by a thick, white, odorless discharge that resembles cottage cheese. Know that 75% of women will get a yeast infection at some point in their life.
- Skin infection: If you have a fungal infection on the skin of your hands or feet, you may see a rash, spots, and blisters between your toes or fingers. You may also see white patches appear on your nails.
- Thrush: A fungal infection in the throat is also called thrush. You will notice that your throat is red and that there are white, fluid-filled bumps or spots in the back of your mouth, near your throat, and on the tongue. You may also notice that you get cracks in the corners of your mouth and that it is difficult to swallow.
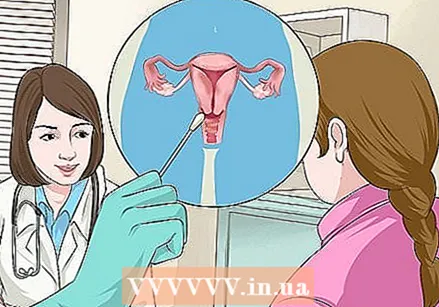
 Go to the doctor. If you experience the symptoms listed above, you should see your doctor to confirm the diagnosis. This is especially important if you have a vaginal infection for the first time. It is important to have the diagnosis confirmed as there are different types of vaginal infections that are sometimes mistaken for a yeast infection. In fact, research shows that only 35% of women were able to correctly diagnose yeast infection on the basis of the symptoms.
Go to the doctor. If you experience the symptoms listed above, you should see your doctor to confirm the diagnosis. This is especially important if you have a vaginal infection for the first time. It is important to have the diagnosis confirmed as there are different types of vaginal infections that are sometimes mistaken for a yeast infection. In fact, research shows that only 35% of women were able to correctly diagnose yeast infection on the basis of the symptoms. - Once you have had a vaginal yeast infection, which has been diagnosed by your doctor, you can subsequently make the diagnosis yourself and treat the infection with over-the-counter remedies.
- Know that a recurring yeast infection could be a sign that something more serious is going on, such as diabetes, cancer, or HIV / AIDS.
- Also call your doctor if the symptoms do not improve after three days, if you have a fever, or if the symptoms change (e.g. the vaginal discharge changes color, you get different rashes on your body, etc.)
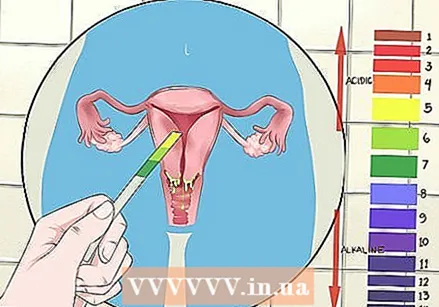 Buy a pH test. If you suspect you have a vaginal yeast infection, the best-known type of yeast infection, and you've had it before, you can buy a pH test and diagnose it yourself.Normally, the vagina's pH is around 4, which means it is slightly acidic. Follow the instructions that come with the test.
Buy a pH test. If you suspect you have a vaginal yeast infection, the best-known type of yeast infection, and you've had it before, you can buy a pH test and diagnose it yourself.Normally, the vagina's pH is around 4, which means it is slightly acidic. Follow the instructions that come with the test. - To take the test, hold a pH strip against the wall of your vagina for a few seconds. Compare the color of the paper with the table included with the test. The number in the table next to the color that most closely matches the color of the strip is the pH of your vagina.
- If the result is above 4, see your doctor. This does not indicate a fungal infection, but may be a sign of another infection.
- If your rash is below 4, you probably have a yeast infection.
Part 2 of 3: Symptoms of a complicated fungal infection
 Look at the shape of the rash. If the fungal infection is allowed to grow untreated, it can take on the shape of a circle that can be red or colorless. This can occur with both vaginal and skin infections.
Look at the shape of the rash. If the fungal infection is allowed to grow untreated, it can take on the shape of a circle that can be red or colorless. This can occur with both vaginal and skin infections. - This circle can cause hair loss if the affected area is a hairy part of the body (such as a man's beard, scalp, or groin).
 Check if your fingernails are affected. A skin infection can spread to the nail bed if left untreated. If the fungal infection also affects the fingernails, it will appear as a red, swollen, and painful area around the fingernail. Eventually, the nails may fall off, leaving a discolored white or pale yellow nail bed.
Check if your fingernails are affected. A skin infection can spread to the nail bed if left untreated. If the fungal infection also affects the fingernails, it will appear as a red, swollen, and painful area around the fingernail. Eventually, the nails may fall off, leaving a discolored white or pale yellow nail bed.  Assess whether you belong to a certain risk group. Certain risk groups are more likely to have a complicated fungal infection, such as:
Assess whether you belong to a certain risk group. Certain risk groups are more likely to have a complicated fungal infection, such as: - People who have had four or more fungal infections within a year
- Pregnant women
- People with untreated diabetes
- People with a weakened immune system (due to medicines or a condition such as HIV)
 Know that a yeast infection will not pass Candida albicans caused is considered complicated. Most fungal infections are caused by the candida fungus Candida albicans. Sometimes, however, another candida fungus is responsible for the infection. This makes the situation more difficult, as most over-the-counter and prescription drugs are made to treat the body Candida albicans to fight. Therefore, infections caused by other fungi often require more aggressive treatment.
Know that a yeast infection will not pass Candida albicans caused is considered complicated. Most fungal infections are caused by the candida fungus Candida albicans. Sometimes, however, another candida fungus is responsible for the infection. This makes the situation more difficult, as most over-the-counter and prescription drugs are made to treat the body Candida albicans to fight. Therefore, infections caused by other fungi often require more aggressive treatment. - Know that the only way to diagnose another type of Candida fungus is to have your doctor take a sample and examine it to identify the fungus.
Part 3 of 3: Knowing the risk factors
 Know that antibiotic treatment can lead to a fungal infection. Long-term use of antibiotics not only kills the pathogenic bacteria in the body, but also the "good bacteria". This can cause an imbalance in the flora of the mouth, skin and vagina, causing an abundance of fungi.
Know that antibiotic treatment can lead to a fungal infection. Long-term use of antibiotics not only kills the pathogenic bacteria in the body, but also the "good bacteria". This can cause an imbalance in the flora of the mouth, skin and vagina, causing an abundance of fungi. - If you have recently taken antibiotics and get a burning or itchy feeling, you may have a yeast infection.
 Know that pregnant women are more likely to get yeast infections. Pregnancy increases the amount of sugar in the vaginal secretions (due to estrogen and progesterone), which is why a fungus thrives. If the yeast thrives, it creates an imbalance in the normal vaginal flora, which can lead to a yeast infection.
Know that pregnant women are more likely to get yeast infections. Pregnancy increases the amount of sugar in the vaginal secretions (due to estrogen and progesterone), which is why a fungus thrives. If the yeast thrives, it creates an imbalance in the normal vaginal flora, which can lead to a yeast infection.  Reduce the chance by making some adjustments in your lifestyle. Illness, obesity, poor sleep and stress increase the risk of a fungal infection.
Reduce the chance by making some adjustments in your lifestyle. Illness, obesity, poor sleep and stress increase the risk of a fungal infection. - Obesity is primarily a potential risk factor, because overweight people have more folds in their skin, where it is warmer and more moist than people who are not overweight. These large folds create the ideal conditions for yeast to grow.
- Obesity has also been linked to diabetes, making these people twice as likely to get a yeast infection.
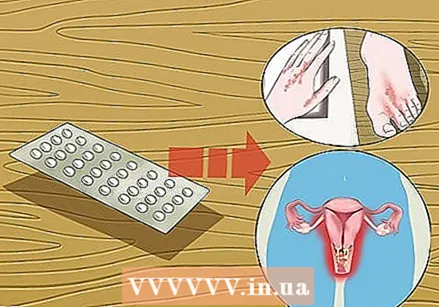 Know that the birth control pill is also a risk factor. The pill and the "morning after pill" cause a change in hormone levels - especially estrogen - which can make you more likely to get a fungal infection.
Know that the birth control pill is also a risk factor. The pill and the "morning after pill" cause a change in hormone levels - especially estrogen - which can make you more likely to get a fungal infection. - The more estrogen in the contraceptive pill, the greater the risk of a yeast infection.
 Understand that your cycle can also affect your chances of getting a yeast infection. A woman is most likely to have a fungal infection around her period. During menstruation, estrogen releases glycogen (a type of sugar found in cells) through the vaginal wall. When the amount of progesterone peaks, cells in the vagina are shed, making the sugar available for the yeast, which can then multiply.
Understand that your cycle can also affect your chances of getting a yeast infection. A woman is most likely to have a fungal infection around her period. During menstruation, estrogen releases glycogen (a type of sugar found in cells) through the vaginal wall. When the amount of progesterone peaks, cells in the vagina are shed, making the sugar available for the yeast, which can then multiply. 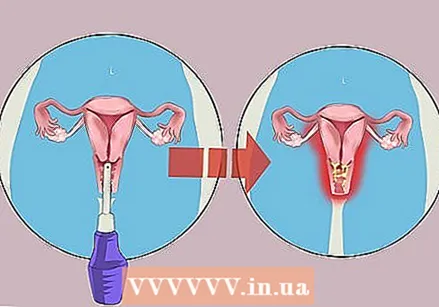 Be aware that excessive use of douches can cause a yeast infection. Vaginal douches are usually used to clean the vagina after menstruation, but this is actually unnecessary and can even be harmful. According to obstetricians and gynecologists, the overuse of vaginal douches can disrupt the balance of the vaginal flora and acidity, thus also disrupting the balance between good and bad bacteria. The good bacteria create an acidic environment, and destroying them creates an abundance of bad bacteria, which can eventually cause a fungal infection.
Be aware that excessive use of douches can cause a yeast infection. Vaginal douches are usually used to clean the vagina after menstruation, but this is actually unnecessary and can even be harmful. According to obstetricians and gynecologists, the overuse of vaginal douches can disrupt the balance of the vaginal flora and acidity, thus also disrupting the balance between good and bad bacteria. The good bacteria create an acidic environment, and destroying them creates an abundance of bad bacteria, which can eventually cause a fungal infection.  Keep in mind that a medical condition can also be a risk factor for fungal infections. Certain illnesses or conditions are related to fungal infections.
Keep in mind that a medical condition can also be a risk factor for fungal infections. Certain illnesses or conditions are related to fungal infections. - For example, a suppressed immune system, due to HIV or a recent organ transplant, can cause a fungal infection.
- Thyroid or hormone imbalance and diabetes can also contribute to the growth of fungi.
Tips
- To prevent fungal infections, keep the folds in your skin as dry as possible.
Warnings
- It's important to remember that the first time you have a vaginal yeast infection, get it diagnosed by your doctor. There are all kinds of other vaginal infections that are often mistaken for a yeast infection, but must be treated in a different way. After the initial diagnosis, you can continue to treat a fungal infection at home (if there are no complications).