Author:
Florence Bailey
Date Of Creation:
21 March 2021
Update Date:
1 July 2024

Content
- Steps
- Part 1 of 3: Getting Ready to Take a Throat Swab
- Part 2 of 3: Taking a smear effectively
- Part 3 of 3: Understanding the Process
- Tips
More often than not, the classic cold and hoarse throat will go away on its own after a week or so. However, sometimes things can be more serious and not go away as easily - like when you decide to go to the doctor, who can order a throat swab for you. In order to determine the causative agent that is the cause of the infection, you need to do some tests. One of the most important tests is called a throat swab. To learn how to make it - or make it yourself - start with Step 1 below.
Steps
Part 1 of 3: Getting Ready to Take a Throat Swab
 1 Double check that the patient is not rinsing his mouth or taking antibiotics. A patient who has used a rinse solution or has taken any antibiotics (or anti-inflammatory drugs) before taking a swab may have inaccurate data. When either of the above two actions is performed, most organisms are flushed off the throat or tonsils, which is bound to result in a sample mismatch that will not be sufficient to collect and analyze a throat swab.
1 Double check that the patient is not rinsing his mouth or taking antibiotics. A patient who has used a rinse solution or has taken any antibiotics (or anti-inflammatory drugs) before taking a swab may have inaccurate data. When either of the above two actions is performed, most organisms are flushed off the throat or tonsils, which is bound to result in a sample mismatch that will not be sufficient to collect and analyze a throat swab. - The patient may ask, “why not rinse or remove the organisms? Isn't that the point? " Yes, it is, but remind him that it will not completely cure the infection. Organisms can disappear from the surface, but they will still remain in the body, which means that the infection has not technically gone away.
- Apart from avoiding these two actions, no preparation is needed. The patient can eat and drink as usual.
- The patient may ask, “why not rinse or remove the organisms? Isn't that the point? " Yes, it is, but remind him that it will not completely cure the infection. Organisms can disappear from the surface, but they will still remain in the body, which means that the infection has not technically gone away.
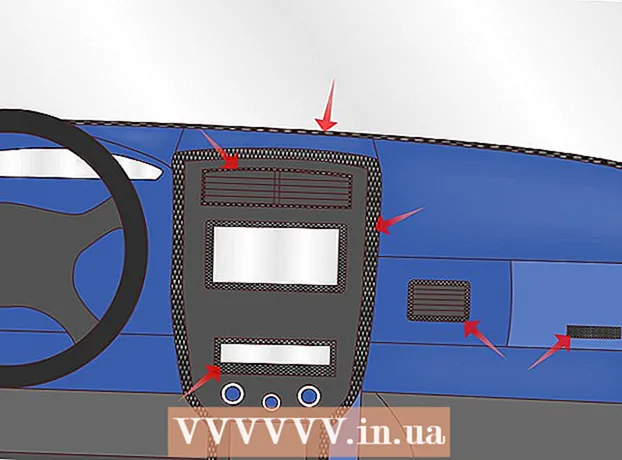
 2 Label the container. The container that will hold your swab for analysis is called a “blood agar plate”. Label it with the patient's name to avoid confusion when sent to the laboratory. Write legibly with a permanent marker or pen.
2 Label the container. The container that will hold your swab for analysis is called a “blood agar plate”. Label it with the patient's name to avoid confusion when sent to the laboratory. Write legibly with a permanent marker or pen. - If the smear is assigned to the wrong patient, he or she will not be able to receive proper treatment, leading to serious complications. Follow exactly the directions the doctor gave you or the patient.
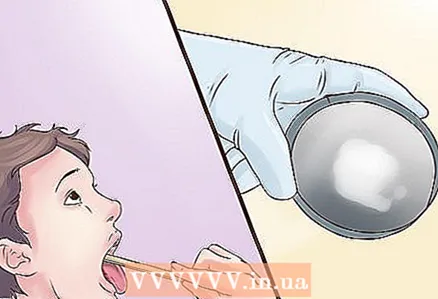
 3 Place the pressure spatula on the patient's tongue. Let him easily tilt his head back and tell him to open his mouth as wide as possible. Then, using a flat stick (much like an ice cream stick), place it on your tongue and press forward slightly to get a better view of your mouth and throat.
3 Place the pressure spatula on the patient's tongue. Let him easily tilt his head back and tell him to open his mouth as wide as possible. Then, using a flat stick (much like an ice cream stick), place it on your tongue and press forward slightly to get a better view of your mouth and throat. - Examine the patient's mouth, as well as his throat, for visible red or sore spots. In such places it will be necessary to take a smear.
 4 Prepare the patient for very short-term discomfort. The patient may feel a vomiting spasm when the shaving brush touches his tonsils or the back of his throat, but this will not last more than a couple of seconds, so it will not be unpleasant for a long time.
4 Prepare the patient for very short-term discomfort. The patient may feel a vomiting spasm when the shaving brush touches his tonsils or the back of his throat, but this will not last more than a couple of seconds, so it will not be unpleasant for a long time. - As mentioned above, for more serious infections with fever, the procedure can be a little painful if the mouth is very sore. But in these cases, neither you nor the patient should be worried either. The pain will quickly dissipate.
Part 2 of 3: Taking a smear effectively
 1 Take a swab. Take a sterile swab and rub it lightly on the red and swollen areas at the back of your throat or near your tonsils. This will ensure that the leaked pus or mucus gets well on the tampon.
1 Take a swab. Take a sterile swab and rub it lightly on the red and swollen areas at the back of your throat or near your tonsils. This will ensure that the leaked pus or mucus gets well on the tampon. - In case a throat swab is taken from a child, have it on your lap. He must be calm so that the right sample is taken in the right place. This will also prevent any chance of injury to the baby due to any sudden movement during the procedure.
 2 Make a sample. Gently roll the swab over the surface of the blood agar plate. After completing the procedure, discard the swab and squeezing spatula into a biohazard waste container.
2 Make a sample. Gently roll the swab over the surface of the blood agar plate. After completing the procedure, discard the swab and squeezing spatula into a biohazard waste container. - If the doctor takes care of the rest, send the container to the microbiological laboratory, it will be placed in a special environment and analyzed by microbiologists. This will give the doctor the opportunity to find out which microorganism is affecting the patient.
- After a couple of days of analysis by microbiology or pathology laboratories, you will receive a report indicating which microorganism is causing the infection in the patient. Based on this, the doctor will select the drugs that are most effective against the infection caused by that particular organism.
 3 Create a suitable environment and research the content if possible. If you are analyzing the sample yourself, take a blood agar plate and place it in a candle jar. Next, place the vessel in a 35-37 ° Celsius (95-98 ° F) incubator. The vessel should be left in the incubator for at least 18 hours.
3 Create a suitable environment and research the content if possible. If you are analyzing the sample yourself, take a blood agar plate and place it in a candle jar. Next, place the vessel in a 35-37 ° Celsius (95-98 ° F) incubator. The vessel should be left in the incubator for at least 18 hours. - If fungus is suspected, the incubation period should be longer. In some cases, you will not see results within a week.
 4 After 18-20 hours, remove the vessel and examine the bacterial colonies (beta hemolytic content). If you find any trace of a colony, the test is positive and the patient suffers from a bacterial infection. However, further testing will be required to determine which bacteria it is.
4 After 18-20 hours, remove the vessel and examine the bacterial colonies (beta hemolytic content). If you find any trace of a colony, the test is positive and the patient suffers from a bacterial infection. However, further testing will be required to determine which bacteria it is. - If nothing grows in the container, the test is negative. If the test results are negative, the patient may be infected with a viral infection caused by pathogens such as enterovirus, herpes simplex virus, Epstein-Barr virus, or respiratory syncytial virus. Chemical tests or microscopic examinations will need to be done to determine what type of infection is affecting the patient.
Part 3 of 3: Understanding the Process
 1 Know when to take a throat swab. Only for some diseases a throat swab is needed. The process is right for you if the following applies to you:
1 Know when to take a throat swab. Only for some diseases a throat swab is needed. The process is right for you if the following applies to you: - "Sore throat". A throat swab is done when you want to determine the cause of a sore throat. Although most of his diseases are caused by viruses, there are times when bacteria are the cause. A throat swab can tell you the difference between a virus infection and a bacterial infection. It is very important to know if a virus or bacteria is causing the symptoms because you can develop a treatment plan.
- "Carriers". A carrier is a person who is infected but does not experience any of the characteristic symptoms. Identifying the carrier is important because you can isolate it from others, thus preventing the spread of the infection.
 2 Have an idea of what a throat swab is and what it does. When you mention a throat swab, you are talking about a test done to identify the causative agent of a bacterial or fungal throat infection. A throat swab is never done for "viral" infections. Viruses are hard to grow and tests will be very expensive.
2 Have an idea of what a throat swab is and what it does. When you mention a throat swab, you are talking about a test done to identify the causative agent of a bacterial or fungal throat infection. A throat swab is never done for "viral" infections. Viruses are hard to grow and tests will be very expensive. - An ear, nose or throat infection means that various microorganisms have entered our body and live in places like blood and saliva. As a defense mechanism, the body tries to attack these microorganisms in a natural way. As a result, pus appears. Pus mainly contains our body's defense cells (mainly "white bodies" and their by-products) and the infecting organism.
- Mucus also forms in large quantities during infection to trap microorganisms. As a result, we spit it out - this is our body's attempt to get rid of the infection. While the microorganism-laden mucus and pus stink, often painful and accompanied by fever, they are very helpful in diagnosing your condition and ultimately finding the most appropriate treatment for you.
 3 Know what a throat swab can detect. When a throat swab is taken, the causative agent of the infection can be one of the following:
3 Know what a throat swab can detect. When a throat swab is taken, the causative agent of the infection can be one of the following: - "Streptococcus group A".These bacteria are the cause of many diseases, including scarlet fever, strep throat, or rheumatism.
- "Candida albicans". Candida albicans is a fungus that can cause candidal stomatitis, an infection that occurs in the mouth and on the surface of the tongue. It can sometimes spread to the throat, causing an infection.
- "Meningococcus". Meningococcus is a bacteria that causes meningitis, an acute inflammation of the meninges (the protective membranes that cover the spinal cord and brain).
- If the bacteria is identified, you can do a sensitivity or susceptibility test. This is a test that will show you which antibiotic will work best for you against the pathogen.
 4 If you suspect a group A strep infection, consider doing a quick strep test before your throat swab. The results of this analysis will be ready in 10 minutes, and it will take 1 or 2 days to get the result with a throat swab. Thus, it’s very easy to do beforehand to narrow down potential causes.
4 If you suspect a group A strep infection, consider doing a quick strep test before your throat swab. The results of this analysis will be ready in 10 minutes, and it will take 1 or 2 days to get the result with a throat swab. Thus, it’s very easy to do beforehand to narrow down potential causes. - To be clear, a throat swab is more accurate than a rapid strep test. A quick test for streptococcus can also give a false negative result. If this test is positive, a throat swab is not needed, but it should be done if the test is negative.
Tips
- Occasionally, your doctor may ask you to gargle salt and spit it out on the glass for analysis. This procedure is called throat rinsing.