Content
- Steps
- Part 1 of 3: Notice Changes in Foot Sensitivity
- Part 2 of 3: Notice Other Stop Changes
- Part 3 of 3: Notice Other Symptoms of Neuropathy
- Tips
- Warnings
Diabetes is a chronic disease in which the production of insulin in the pancreas is disrupted or the cells are less sensitive to the effects of this hormone. Insulin is needed by the cells in the body to absorb glucose. If a person with diabetes does not receive appropriate treatment, their blood glucose levels remain consistently high. This leads to damage to organs and nerves, especially the small peripheral nerves that innervate the tissues of the eyes, feet and hands. According to the American Department of Health, 60-70% of people with diabetes suffer from various forms of damage to the nerve tissue (neuropathy). Most often, the first symptoms associated with diabetes appear on the feet. That is why it is important to know exactly how these symptoms manifest and to check the condition of the feet regularly to avoid irreversible tissue damage and disability.
Steps
Part 1 of 3: Notice Changes in Foot Sensitivity
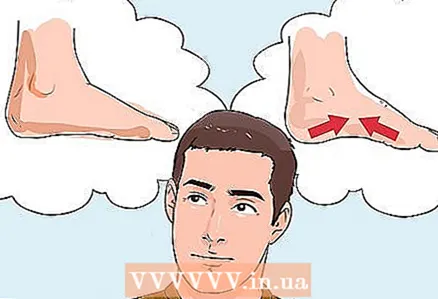
 1 Pay attention to the feeling of numbness in the feet. One of the first and widespread symptoms of peripheral neuropathy that diabetes patients pay attention to is a decrease in the sensitivity of the feet and a feeling of tissue numbness. Often, numbness occurs in the area of the fingers, then spreads to the entire foot and gradually rises up, covering the ankle. Usually, the process develops on the soles of both legs, although sometimes numbness initially occurs in only one limb or is felt more strongly in one of the feet.
1 Pay attention to the feeling of numbness in the feet. One of the first and widespread symptoms of peripheral neuropathy that diabetes patients pay attention to is a decrease in the sensitivity of the feet and a feeling of tissue numbness. Often, numbness occurs in the area of the fingers, then spreads to the entire foot and gradually rises up, covering the ankle. Usually, the process develops on the soles of both legs, although sometimes numbness initially occurs in only one limb or is felt more strongly in one of the feet. - Loss of sensitivity is accompanied by a decrease in a person's ability to feel pain from exposure to high and low temperatures. Because of this, people with diabetes have an increased risk of burns when they take a hot bath, as well as the risk of frostbite in winter.
- Chronic loss of sensation of the feet leads to the fact that the patient with diabetes often does not notice cuts, calluses and other injuries in the area of the feet. This phenomenon quite often occurs with this disease, which increases the risk of infection of the lesions. In some cases, the neuropathy is so severe that the infection in the wounds develops over a long period, sometimes spreading into deeper tissues and even seizing the bones of the foot, without the patient even noticing it. Treatment of such an infection requires a long course of IV generation antibiotics, and in some cases even the patient's life is threatened.
- As a rule, symptoms of peripheral neuropathy, including loss of sensation, are more pronounced at night when the person is in bed.
 2 Pay attention to the burning and tingling sensations. Another characteristic symptom is an unpleasant tingling sensation, goose bumps, and burning. All this is similar to the sensations that arise in the foot when blood circulation is resumed, if you "sat" the leg. These discomforts, called parasthesia, range from mild to severe and usually show up differently in the right and left feet.
2 Pay attention to the burning and tingling sensations. Another characteristic symptom is an unpleasant tingling sensation, goose bumps, and burning. All this is similar to the sensations that arise in the foot when blood circulation is resumed, if you "sat" the leg. These discomforts, called parasthesia, range from mild to severe and usually show up differently in the right and left feet. - The tingling and burning sensation usually occurs in the lower part of the foot (sole), and later the process can spread to the overlying areas of the feet.
- These discomforts sometimes resemble a fungal infection (athlete's foot) or insect bites, although itching is rarely felt with a diabetic foot.
- Peripheral neuropathy in the tissues of the foot develops because high blood sugar (glucose) levels are toxic and cause damage to small peripheral nerves.
 3 Pay attention if you experience increased sensitivity to touch (hyperesthesia). In rare cases, people with diabetes may develop another type of sensory impairment - increased sensitivity to touch. Instead of the symptoms of a typical diabetic foot (decreased sensitivity and numbness of the foot), some patients develop sensitivity (or even hypersensitivity) to touch. For example, in patients with hyperesthesia, unbearable pain occurs even due to touching the skin of the feet with bed linen.
3 Pay attention if you experience increased sensitivity to touch (hyperesthesia). In rare cases, people with diabetes may develop another type of sensory impairment - increased sensitivity to touch. Instead of the symptoms of a typical diabetic foot (decreased sensitivity and numbness of the foot), some patients develop sensitivity (or even hypersensitivity) to touch. For example, in patients with hyperesthesia, unbearable pain occurs even due to touching the skin of the feet with bed linen. - This complication of diabetes often resembles a gout attack or acute inflammatory arthritis, and in some cases, the patient may be misdiagnosed.
- Patients describe sensations arising from increased sensitivity of the foot as pain that resembles a burn or an electric shock.
 4 Pay attention to cramping or sharp pain. As peripheral neuropathy intensifies, the pathological process spreads to muscle tissue. One of the first symptoms to indicate that the complications of diabetes have affected the muscles is cramps or sharp shooting pains in the feet, most often in the sole area. The cramps and pain can be so excruciating that a diabetic person cannot walk; at night, when a person is in bed, the pain sensations tend to intensify.
4 Pay attention to cramping or sharp pain. As peripheral neuropathy intensifies, the pathological process spreads to muscle tissue. One of the first symptoms to indicate that the complications of diabetes have affected the muscles is cramps or sharp shooting pains in the feet, most often in the sole area. The cramps and pain can be so excruciating that a diabetic person cannot walk; at night, when a person is in bed, the pain sensations tend to intensify. - Unlike normal seizures, where muscle contraction or twitching can be seen, diabetic foot cramps often have no external manifestations.
- Another sign that distinguishes ordinary cramps from diabetic foot cramps is that pain and discomfort do not diminish or disappear when walking.
- In some cases, pain and cramps in a diabetic foot resemble symptoms of a stress fracture or Willys-Ekbom disease, which poses a risk of misdiagnosis.
Part 2 of 3: Notice Other Stop Changes
 1 Pay attention to muscle weakness. Glucose of high concentration penetrates into the nerve fibers, and therefore, according to the law of osmosis, water enters the fibers. Because of this, the volume of nerve fibers increases, and the blood supply to the nerve tissue deteriorates, so the nerve tissues begin to die off. If the nerve fiber that innervates the muscle tissue dies off, nerve signals no longer enter the muscles. In the absence of nerve stimulation, the muscles atrophy (dry out). As a result of muscle atrophy, the feet are reduced in size, in addition, muscle weakness affects a person's gait, making it staggering and unstable. People who have had diabetes for a long time can often only walk with a cane or even have to use a wheelchair.
1 Pay attention to muscle weakness. Glucose of high concentration penetrates into the nerve fibers, and therefore, according to the law of osmosis, water enters the fibers. Because of this, the volume of nerve fibers increases, and the blood supply to the nerve tissue deteriorates, so the nerve tissues begin to die off. If the nerve fiber that innervates the muscle tissue dies off, nerve signals no longer enter the muscles. In the absence of nerve stimulation, the muscles atrophy (dry out). As a result of muscle atrophy, the feet are reduced in size, in addition, muscle weakness affects a person's gait, making it staggering and unstable. People who have had diabetes for a long time can often only walk with a cane or even have to use a wheelchair. - Weakness in the muscles of the feet and ankles is often accompanied by damage to the nerves responsible for transmitting signals to the brain for balance and coordination of movements, so people with diabetes have significant difficulty walking.
- Nerve damage and weakness in the muscles and ligaments of the ankles lead to decreased reflexes. For example, tapping the Achilles tendon produces, at best, only a weak response (twitching of the foot).
 2 Check to see if you have developed finger deformities. If a person develops muscle weakness in the feet and gait changes, they have to position their legs differently when walking and transfer additional stress to the fingers. Excessive pressure and abnormal weight loading often lead to deformities of the fingers, such as hammer curvature. Hammer curvature occurs when the shape of one of the three middle toes of the foot changes. The pathology develops in the distal joint, as a result of which the finger bends and resembles a hammer in shape. In addition to hammer curvature and other deformities, uneven gait and imbalance often lead to a redistribution of pressure to different areas of the foot, which leads to excessive stress on certain areas of the sole. As a result, trophic ulcers form on the feet, and if tissues are involved in the infectious process, this can lead to a number of serious problems.
2 Check to see if you have developed finger deformities. If a person develops muscle weakness in the feet and gait changes, they have to position their legs differently when walking and transfer additional stress to the fingers. Excessive pressure and abnormal weight loading often lead to deformities of the fingers, such as hammer curvature. Hammer curvature occurs when the shape of one of the three middle toes of the foot changes. The pathology develops in the distal joint, as a result of which the finger bends and resembles a hammer in shape. In addition to hammer curvature and other deformities, uneven gait and imbalance often lead to a redistribution of pressure to different areas of the foot, which leads to excessive stress on certain areas of the sole. As a result, trophic ulcers form on the feet, and if tissues are involved in the infectious process, this can lead to a number of serious problems. - In some cases, the hammer toe will disappear on its own, but in most cases, surgery is required to correct the defect.
- A typical deformity in a diabetic foot is an enlargement of the big toe bone caused by constantly pressing the big toe against the other toes.
- If you have diabetes, it is very important to choose the right shoes - they should be loose. In this way, the fingers will not be squeezed, and the risk of deformation will be reduced. Women with diabetes should not wear high-heeled shoes.
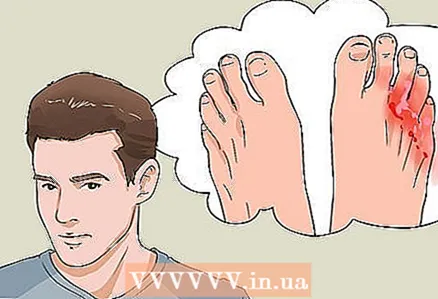
 3 Be extremely alert for any signs of injury or infection to the foot. Apart from bone fractures from falls while walking, foot injuries are the most common complication faced by people with diabetes. Because of the desensitization, people with diabetes often fail to notice minor damage to the skin of their feet, such as abrasions, shallow cuts, calluses, and insect bites. For this reason, such minor injuries can become inflamed, which in turn is potentially dangerous in terms of spreading the infection into the surrounding tissues. In severe cases, this can result in the amputation of the toe or even the entire foot.
3 Be extremely alert for any signs of injury or infection to the foot. Apart from bone fractures from falls while walking, foot injuries are the most common complication faced by people with diabetes. Because of the desensitization, people with diabetes often fail to notice minor damage to the skin of their feet, such as abrasions, shallow cuts, calluses, and insect bites. For this reason, such minor injuries can become inflamed, which in turn is potentially dangerous in terms of spreading the infection into the surrounding tissues. In severe cases, this can result in the amputation of the toe or even the entire foot. - Visual signs of infection include tissue swelling, discoloration (the skin becomes bluish or reddish), and discharge of whitish pus or other fluid from the wound.
- An infected wound often gives off an unpleasant odor, as pus and blood are released from it.
- People with chronic diabetes often have a weakened immune system, resulting in a longer wound healing time.
- If a serious open wound (such as an ulcer with signs of gangrene) develops at the site of a minor abrasion, seek medical attention as soon as possible.
- Doctors recommend that people with diabetes get their feet checked at least once a week. When a patient comes to the next appointment with his doctor, he must examine the condition of the patient's feet for complications.
Part 3 of 3: Notice Other Symptoms of Neuropathy
 1 Pay attention to similar symptoms on the hands. Although peripheral neuropathy usually begins in the lower extremities (mainly in the feet), similar processes develop in the small peripheral nerve fibers that innervate the hands, fingers, and forearms. So be careful and check regularly to see if the aforementioned symptoms that indicate complications of diabetes are showing up in the tissues of your hands.
1 Pay attention to similar symptoms on the hands. Although peripheral neuropathy usually begins in the lower extremities (mainly in the feet), similar processes develop in the small peripheral nerve fibers that innervate the hands, fingers, and forearms. So be careful and check regularly to see if the aforementioned symptoms that indicate complications of diabetes are showing up in the tissues of your hands. - As already mentioned, pathological processes in the feet develop from the fingers and rise up. Similarly, complications in the upper limbs first appear in the area of the hands and then spread to the area of the forearms.
- Complications of diabetes in the tissues of the hands resemble in their manifestations carpal tunnel syndrome and Raynaud's disease (in this disease, the arteries, when exposed to low temperatures, narrow more than normal). For this reason, the patient may be misdiagnosed.
- It is much easier to monitor the health of your hands and check them regularly for complications - you usually wear socks and shoes on your feet.
 2 Check for symptoms of autonomic neuropathy. The autonomic nervous system provides automatic regulation of heart contractions and controls the functioning of internal organs: the bladder, lungs, stomach, intestines, genitals and eyes. Diabetes (hyperglycemia) affects nerve fibers, which causes a variety of complications, including heart palpitations, hypotension, urinary retention, urinary incontinence, constipation, bloating, loss of appetite, trouble swallowing food, erectile dysfunction, and vaginal dryness.
2 Check for symptoms of autonomic neuropathy. The autonomic nervous system provides automatic regulation of heart contractions and controls the functioning of internal organs: the bladder, lungs, stomach, intestines, genitals and eyes. Diabetes (hyperglycemia) affects nerve fibers, which causes a variety of complications, including heart palpitations, hypotension, urinary retention, urinary incontinence, constipation, bloating, loss of appetite, trouble swallowing food, erectile dysfunction, and vaginal dryness. - Excessive sweating (or no sweating at all) of the feet or other parts of the body is a typical sign of autonomic neuropathy.
- Extensive autonomic neuropathy leads to dysfunction of internal organs, therefore, patients with diabetes often develop heart disease and renal failure.
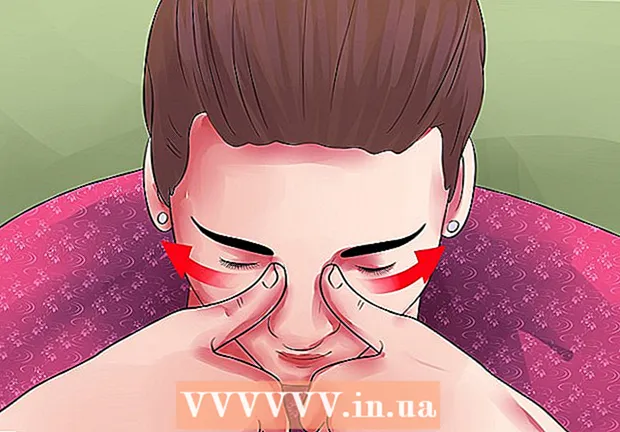
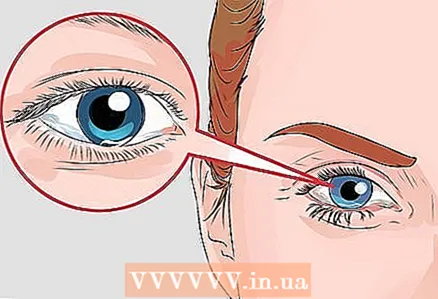 3 Pay attention to any changes in vision. Peripheral and autonomic neuropathies affect the functioning of the eyes, in addition, vision suffers from dysfunction of small blood vessels caused by the toxic effects of glucose. Infection of the tissues of the feet and the associated risk of amputation of the feet and legs is one of the greatest fears of people with diabetes. The second serious danger that every diabetic patient remembers is loss of vision. Complications affecting the visual system include difficulty adapting to low light conditions, blurred vision, watery eyes, and gradual loss of visual acuity leading to blindness.
3 Pay attention to any changes in vision. Peripheral and autonomic neuropathies affect the functioning of the eyes, in addition, vision suffers from dysfunction of small blood vessels caused by the toxic effects of glucose. Infection of the tissues of the feet and the associated risk of amputation of the feet and legs is one of the greatest fears of people with diabetes. The second serious danger that every diabetic patient remembers is loss of vision. Complications affecting the visual system include difficulty adapting to low light conditions, blurred vision, watery eyes, and gradual loss of visual acuity leading to blindness. - Diabetic retinopathy is characterized by damage to the blood vessels that feed the retina, which is the most common cause of vision loss in diabetic patients.
- It has been proven that adults with diabetes have a two to five times higher risk of developing cataracts than those without the disease.
- People with diabetes have an increased risk of developing cataracts (clouding of the lens) and glaucoma (increased pressure in the eye and damage to the optic nerve).
Tips
- If you have diabetes, you should check your feet daily for symptoms of complications. This should be done even if you are taking diabetes medications.
- If you experience any of the above symptoms, make an appointment with your doctor or see an endocrinologist for a doctor to check your health.
- Trim your nails regularly (every week or every two weeks).If you're worried about getting your toes hurt when trimming your nails, you can entrust your foot care to a professional who does a medical manicure.
- Always wear shoes with socks and slippers when you are at home. Avoid walking barefoot or wearing tight shoes - this increases the risk of blisters.
- People with diabetes often experience excessive sweating of the feet and the skin of the feet looks shiny. In this case, you need more socks than me so that they always remain dry.
- Wash your feet daily with warm (but not hot) soap and water. Rinse off the soap thoroughly with clean water and pat dry with a towel (do not rub). Make sure to dry the skin well between your toes.
- It is recommended to regularly make foot salt baths. This will help disinfect the skin of your feet and reduce the risk of bacterial infections.
- If the skin of the feet is very dry, cracks and damage may form on it at the point where the shoes are squeezed. Remember to regularly apply moisturizer to your feet. Lubricate dry areas of skin with moisturizing lotion or petroleum jelly, being careful not to get the product on the skin between your toes.
Warnings
- If you notice black or greenish areas on the surface of the foot, seek medical attention immediately: this may be a sign of gangrene (tissue death).
- Do not use moisturizing lotion on the skin between your toes - this can lead to the development of fungus.
- If your foot has an ulcer or an unhealed wound, see your doctor right away.