Author:
Mark Sanchez
Date Of Creation:
6 January 2021
Update Date:
3 July 2024

Content
- Steps
- Method 1 of 5: Interim Measures
- Method 2 of 5: Treating a fungal infection
- Method 3 of 5: Treating Bacterial Vaginosis
- Method 4 of 5: Treating STDs
- Method 5 of 5: Treating Non-Infectious Vaginitis
Most women experience unpleasant vaginal itching at some point in their lives. In some cases, mild itching disappears on its own, but it also happens that it does not go away due to illness or allergies. Depending on the specific cause of the itching, home remedies are often sufficient, but it also happens that you need to see a doctor.
Steps
Method 1 of 5: Interim Measures
 1 Apply cold compresses. Regardless of what causes vaginal itching, it can be temporarily relieved with a cold compress (such as a damp, soft washcloth) applied to the labia.
1 Apply cold compresses. Regardless of what causes vaginal itching, it can be temporarily relieved with a cold compress (such as a damp, soft washcloth) applied to the labia. - Take a clean face washcloth for a cold compress and hold it under a stream of cold water until it gets wet. Then squeeze out the excess water and apply the washcloth to the vaginal area for 5-10 minutes.
- Be sure to wash the washcloth after use. Use a fresh, clean loofah for the next compress.
- You can also use an ice pack. Remember to wrap it in a clean towel and don't apply the compress for more than 20 minutes at a time.
 2 Avoid irritants. Washing powder, soap, and other products can irritate the mucous membranes and cause vaginal itching. Switch to unflavored laundry detergents and avoid using fabric softener to avoid itching in your vagina due to an allergic reaction. You can also use a mild cleanser to avoid irritation from regular shower gel.
2 Avoid irritants. Washing powder, soap, and other products can irritate the mucous membranes and cause vaginal itching. Switch to unflavored laundry detergents and avoid using fabric softener to avoid itching in your vagina due to an allergic reaction. You can also use a mild cleanser to avoid irritation from regular shower gel. - Try using Dove soap or Cetaphil mild skin cleanser, for example.
- Do not use scented detergents, wet wipes, powders, or other products that can irritate the vaginal area.
 3 Try using a humidifier. Get a water-based cream or emulsion ointment from your local drugstore that can help reduce vaginal itching. Follow the directions for use and remember that these remedies will not correct the cause of the itching.
3 Try using a humidifier. Get a water-based cream or emulsion ointment from your local drugstore that can help reduce vaginal itching. Follow the directions for use and remember that these remedies will not correct the cause of the itching.  4 Don't scratch the itchy area. Scratching can increase irritation and itching. What's more, it can lead to skin damage and infection, so don't brush the irritated area under any circumstances.
4 Don't scratch the itchy area. Scratching can increase irritation and itching. What's more, it can lead to skin damage and infection, so don't brush the irritated area under any circumstances. 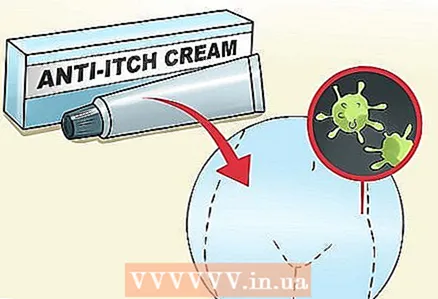 5 Get rid of the cause of the itching. Itching in the vagina can occur for unknown reasons and go away on its own, but if you experience severe or persistent itching, it can be caused by more serious causes. In this case, it is necessary to find out these reasons and try to get rid of them: for example, to cure an infectious disease or avoid contact with irritants.
5 Get rid of the cause of the itching. Itching in the vagina can occur for unknown reasons and go away on its own, but if you experience severe or persistent itching, it can be caused by more serious causes. In this case, it is necessary to find out these reasons and try to get rid of them: for example, to cure an infectious disease or avoid contact with irritants.
Method 2 of 5: Treating a fungal infection
 1 Look for a fungal infection (candidiasis, or thrush). Fungal infections can be difficult to distinguish from other infections, so if in doubt, see your doctor. A fungal infection is often accompanied by symptoms such as inflammation, burning, and pain in the vagina, watery or thick, odorless, white vaginal discharge.
1 Look for a fungal infection (candidiasis, or thrush). Fungal infections can be difficult to distinguish from other infections, so if in doubt, see your doctor. A fungal infection is often accompanied by symptoms such as inflammation, burning, and pain in the vagina, watery or thick, odorless, white vaginal discharge. - A different type of vaginal discharge may indicate a different type of infection.
- Pregnancy, antibiotics, diabetes, or a weakened immune system are more likely to have a fungal infection.
- If you are pregnant and suspect you have an infection, see your doctor. Another type of infection can harm the fetus.
 2 Take over-the-counter medications. There are many creams and vaginal suppositories (suppositories) available for treating fungal infections that can be purchased at your local pharmacy. These remedies are usually sufficient to treat most fungal infections.
2 Take over-the-counter medications. There are many creams and vaginal suppositories (suppositories) available for treating fungal infections that can be purchased at your local pharmacy. These remedies are usually sufficient to treat most fungal infections. - These drugs have different durations of action. In case of recurrent fungal infection, use products that are designed to be used within seven days.
- If you experience severe discomfort, use a medicine that contains an anti-itch ingredient.
- Many formulations contain active ingredients such as butoconazole, clotrimazole, miconazole, and terconazole. These substances have been shown to be quite effective in treating fungal infections.
 3 Consider other treatments. If standard medicines don't work for you, or if you want to use natural remedies, try other methods.
3 Consider other treatments. If standard medicines don't work for you, or if you want to use natural remedies, try other methods. - Use boric acid suppositories. This acid is very effective in killing the yeast that causes thrush. Boric acid suppositories are available at your local pharmacy. Never try to clear the infection with boric acid powder, as it can aggravate irritation. Remember that boric acid is poisonous and avoid oral sex when using it.
- Try tea tree oil. You can treat fungal infections with a tampon dipped in tea tree oil. Use this method with caution and remove the swab if any discomfort occurs. Although tea tree oil is believed to have antifungal properties, more research is needed to confirm its effectiveness in treating fungal infections.
- Treat infection with probiotics. There is some evidence that fungal infections can be eliminated by increasing the number of beneficial bacteria in the body. To do this, you can put lactobacillus tablets, which are sold in pharmacies and health food stores, directly into the vagina. You can even try eating probiotic-rich yogurt or applying it to your vaginal area. Keep in mind, however, that these treatments are less effective than standard treatments and can be quite expensive.
 4 Know when to see a doctor. In most cases, you can get rid of a fungal infection yourself at home, but sometimes you have to seek medical attention. It is usually recommended to see a doctor if you have never had a fungal infection before, as in this case, you may be wrong with the diagnosis. You should also consult a doctor if self-treatment does not work.
4 Know when to see a doctor. In most cases, you can get rid of a fungal infection yourself at home, but sometimes you have to seek medical attention. It is usually recommended to see a doctor if you have never had a fungal infection before, as in this case, you may be wrong with the diagnosis. You should also consult a doctor if self-treatment does not work. - If over-the-counter medications are not working for you, your doctor may prescribe oral medications.
- A fungal infection is often accompanied by a thick, white vaginal discharge. If the discharge is grayish, yellowish, or greenish, see your doctor, as this may not indicate a fungal infection, but another disease.
- If you want to make sure that you have a true fungal infection, but do not want to visit a doctor, you can purchase a self-testing tool at home, such as the Vagisil Screening Test.However, if self-treatment has not worked, you should still consult a doctor.
 5 Try to prevent future fungal infections. You may not be able to completely avoid recurrent fungal infections in the future, but there are many ways to reduce their chances.
5 Try to prevent future fungal infections. You may not be able to completely avoid recurrent fungal infections in the future, but there are many ways to reduce their chances. - Don't take antibiotics unless absolutely necessary. Antibiotics can disrupt the bacterial balance in the vagina and thus cause a fungal infection. They should only be taken if you really need them.
- Wear cotton underwear.
- Avoid overly tight tights, stockings, and underwear.
- Keep the vaginal area cool and dry. Change wet clothes in time and try to avoid hot baths.
- If you are taking birth control pills that contain estrogen and have had repeated fungal infections, consider switching to other birth control pills (such as progestin-only pills), as elevated estrogen levels can contribute to fungal infections.
Method 3 of 5: Treating Bacterial Vaginosis
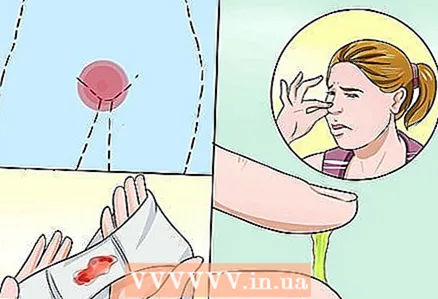
 1 Recognize the symptoms. Bacterial vaginosis is characterized by symptoms such as burning, inflammation, thin, grayish-white discharge, and foul odor of fish from the vagina. The disease may be accompanied by all of these symptoms, only some of them, or they may be absent altogether.
1 Recognize the symptoms. Bacterial vaginosis is characterized by symptoms such as burning, inflammation, thin, grayish-white discharge, and foul odor of fish from the vagina. The disease may be accompanied by all of these symptoms, only some of them, or they may be absent altogether. - The exact causes of bacterial vaginosis are unknown, and some women are more prone to it than others. Many women have bacterial vaginosis at least once a year. This may be due to the decreased levels of naturally occurring beneficial bacteria.
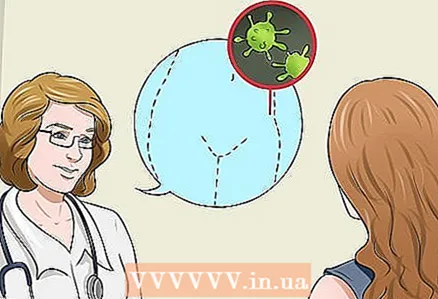 2 See your doctor. Unlike a fungal infection, bacterial vaginosis is difficult to self-treat at home. To get rid of the infection and accompanying symptoms, you should see a doctor who will prescribe the right medication. This can be either an oral agent such as Metronidazole or Tinidazole, or a cream such as Clindamycin.
2 See your doctor. Unlike a fungal infection, bacterial vaginosis is difficult to self-treat at home. To get rid of the infection and accompanying symptoms, you should see a doctor who will prescribe the right medication. This can be either an oral agent such as Metronidazole or Tinidazole, or a cream such as Clindamycin. - To diagnose bacterial vaginosis, your doctor will do a pelvic exam and take a swab from your vagina to check under a microscope. In addition, the doctor can use a test strip to check the pH level in the vagina.
- It is especially important to immediately start treating bacterial vaginosis during pregnancy, as in this case it can lead to serious complications.
 3 Prevent recurrence of vaginosis. While you may not be immune to recurring vaginosis, there are a few simple rules that can help you reduce your risk.
3 Prevent recurrence of vaginosis. While you may not be immune to recurring vaginosis, there are a few simple rules that can help you reduce your risk. - Do not flush the vagina, as this can upset the bacterial balance and lead to infection.
- Do not use perfumed products such as soap, tampons, sprays, and the like.
- Limit the number of sex partners. While the reasons for this remain unclear, women with more sexual partners, who have recently changed partners, or have a female partner are more prone to bacterial vaginosis.
- Dry your vaginal area after showering and avoid hot baths.
- Always wipe from front to back after using the bathroom to prevent fecal bacteria from entering your vagina.
Method 4 of 5: Treating STDs
 1 Learn about the warning signs of sexually transmitted diseases (STDs). Vaginal itching is common in many different STDs. If you experience any of the symptoms listed below, or simply suspect that you may have contracted an STD, see your doctor immediately. Be aware that sometimes STDs go on without any symptoms.
1 Learn about the warning signs of sexually transmitted diseases (STDs). Vaginal itching is common in many different STDs. If you experience any of the symptoms listed below, or simply suspect that you may have contracted an STD, see your doctor immediately. Be aware that sometimes STDs go on without any symptoms. - Trichomoniasis is usually accompanied by redness, strong vaginal odor, and yellow-green vaginal discharge.
- Chlamydia is often asymptomatic, but it can also cause abnormal bleeding, vaginal discharge, and abdominal pain.
- Gonorrhea is usually accompanied by thick, cloudy or bloody vaginal discharge, itching, and painful urination.
- Herpes usually results in red pimples, blisters, and sores in the vaginal area.
- Human papillomaviruses usually cause small, flesh-colored warts around the genitals (there can be quite a few of these warts).
 2 See a doctor. In case of STDs, you need to see a doctor who will prescribe the appropriate treatment. If not treated correctly, some STDs can lead to serious complications, so you need to see your doctor immediately and start taking the medication they are prescribed.
2 See a doctor. In case of STDs, you need to see a doctor who will prescribe the appropriate treatment. If not treated correctly, some STDs can lead to serious complications, so you need to see your doctor immediately and start taking the medication they are prescribed. - Gonorrhea, chlamydia, syphilis, and trichomoniasis are treated with antibiotics. Your doctor will prescribe oral or injectable antibiotics depending on the type of infection.
- Although human papillomaviruses are not treatable, your doctor may be able to suggest measures that will reduce the likelihood of new genital warts forming in the future.
- Herpes can be suppressed with antiviral drugs, which reduce the chances of recurrences, although it cannot be completely cured and there is no guarantee that you will not infect others.
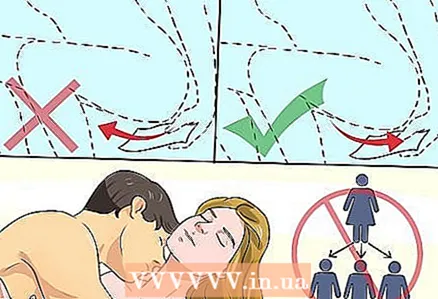
 3 Prevent future infections. The best way to avoid infections later on is to follow safe sex guidelines.
3 Prevent future infections. The best way to avoid infections later on is to follow safe sex guidelines. - The best way to protect yourself from STDs is to abstain from active sex life or have one sex partner you are confident in.
- If you have multiple sex partners, always use condoms when having sex to avoid getting an infection.
Method 5 of 5: Treating Non-Infectious Vaginitis
 1 Learn about the causes and symptoms of the disease. Non-infectious vaginitis is a general term that refers to vaginal irritation that is not caused by any kind of infection. It can be caused by a variety of reasons, including an allergic reaction, skin irritation, or hormonal imbalances.
1 Learn about the causes and symptoms of the disease. Non-infectious vaginitis is a general term that refers to vaginal irritation that is not caused by any kind of infection. It can be caused by a variety of reasons, including an allergic reaction, skin irritation, or hormonal imbalances. - Non-infectious vaginitis can be difficult to distinguish from infection. Fungal infections are often confused with irritation caused by laundry detergents, so you should see your doctor if you are unsure of what exactly is causing your symptoms. Non-infectious vaginitis is often accompanied by a burning sensation in the vagina, vaginal discharge, and pelvic pain.
 2 Stop using possible irritants. Itching in the vagina can be caused by an allergy to certain foods, such as soap or moisturizer.
2 Stop using possible irritants. Itching in the vagina can be caused by an allergy to certain foods, such as soap or moisturizer. - Do not use perfumed products if you have skin sensitivities.
- If vaginal itching occurs soon after using a new remedy, stop using it immediately, replace it with another, and avoid products that contain the same ingredients in the future.
 3 Pay attention to hormonal changes. Many women experience vaginal itching just before and during menopause due to a decrease in estrogen levels. To counter this, your doctor may prescribe estrogen creams, pills, or vaginal rings.
3 Pay attention to hormonal changes. Many women experience vaginal itching just before and during menopause due to a decrease in estrogen levels. To counter this, your doctor may prescribe estrogen creams, pills, or vaginal rings. - If you experience vaginal dryness during menopause, it can be relieved with vaginal moisturizers or water-based sex lubricants.
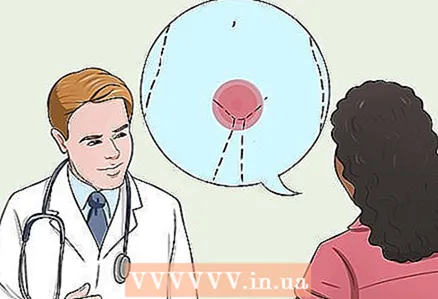
 4 Get rid of skin conditions. Sometimes skin conditions can irritate the skin around the vagina. In this case, it is best to see a dermatologist.
4 Get rid of skin conditions. Sometimes skin conditions can irritate the skin around the vagina. In this case, it is best to see a dermatologist. - With lupus lichen, white flaking patches form on the skin. This condition can be treated with a prescription steroid cream.
- Eczema and psoriasis can also cause vaginal itching. In this case, the gynecologist or dermatologist will prescribe the appropriate medications for you.