Content
- Steps
- Part 1 of 4: Immediate Medical Treatment
- Part 2 of 4: Medical Examination and Diagnosis
- Part 3 of 4: Precautions
- Part 4 of 4: Risk Factors
- Tips
- Warnings
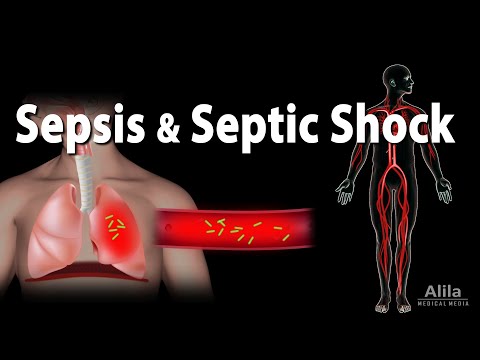
A simple infection can lead to a rapidly developing life-threatening reaction (various organs can fail as a result). Previously, this reaction was called "blood poisoning." If inflammation begins to spread throughout the body, sometimes they talk about systemic inflammatory response syndrome (SSVO), which is also called in some cases or at certain stages sepsis or “septic shock.” This syndrome is a specific set of signs (symptoms) that indicate a particular disease or disorder.
Although SIRS (sepsis) can develop rapidly due to a common infection, it is preceded by mild inflammatory sepsis. Sepsis is an immune condition caused by an infection (most commonly bacteriabut sometimes viruses, parasites or fungus), which, in the opinion of doctors, can quickly become serious and critical. Bacteria can enter the bloodstream, spread from the site of infection (for example, a diseased tooth or gum) throughout the body, penetrate into other organs and damage them - in this case, they speak of a complication of the initial infection. This spread of bacteria throughout the body can cause sepsis.
Sepsis occurs due to the fact that the immune system begins to intensively fight the infection, which leads to an extensive inflammatory process throughout the body, and as a result microscopic blood clots... These clots begin to block small blood vessels, capillaries. This impairs blood flow and oxygen supply and causes vital organs to malfunction, their tissues become damaged and begin to die off (gangrene). Tiny blood clots can enter the brain, heart, lungs, and kidneys, as well as tissues in the hands, feet, and fingers.
- Sepsis occurs when the body's own chemicals enter the bloodstream. to fight infection, and initiates inflammation in the immune system, sometimes throughout the body.
- Mild sepsis can sometimes quickly lead to another condition called "septic shock," causing blood pressure to drop enough to cause death.
With sepsis, it is not so much harmful microbes that are dangerous as the body's reaction to the disease, which can quickly lead to dangerous inflammation or end in chronic diseases. Inflammation is the body's natural defense against disease, necessary to fight germs, but overreaction can lead to death!
Mild and then severe sepsis occurs as a "complication" of infection and develops as the body fights the initial infection and tries to prevent its possible spread.
Attention:the information in this article is for informational purposes only. Before using any methods, consult your doctor.
Steps
Part 1 of 4: Immediate Medical Treatment
 1 Get immediate medical attention if there is any indication that you may have mild or severe sepsis due to a possible infection (see the symptoms below). Emergency medical care allows you to better heal and recover from mild initial stages of sepsis. Every minute counts: the chances of a successful cure quickly diminish over time, as tiny blood clots can damage various organs and limbs and cause tissue death.
1 Get immediate medical attention if there is any indication that you may have mild or severe sepsis due to a possible infection (see the symptoms below). Emergency medical care allows you to better heal and recover from mild initial stages of sepsis. Every minute counts: the chances of a successful cure quickly diminish over time, as tiny blood clots can damage various organs and limbs and cause tissue death.  2 You should see your doctor to assess your condition and to prescribe appropriate treatment for an infection that can cause pain, sometimes throbbing. The infection can be invisible (internal) and very dangerous if not treated. At first, mild sepsis can then lead to serious complications, including amputation, organ failure, septic shock, and even death with a 50% chance - although this is not necessary, there is such a risk! For example, drug-resistant streptococcal infections can cause big problems. Streptococcus is a very common bacterium that can cause SIRS. Sometimes it seems that the infection has passed, while it "lurked" in some organs - this can lead to their gradual inflammation, weakening and damage ..
2 You should see your doctor to assess your condition and to prescribe appropriate treatment for an infection that can cause pain, sometimes throbbing. The infection can be invisible (internal) and very dangerous if not treated. At first, mild sepsis can then lead to serious complications, including amputation, organ failure, septic shock, and even death with a 50% chance - although this is not necessary, there is such a risk! For example, drug-resistant streptococcal infections can cause big problems. Streptococcus is a very common bacterium that can cause SIRS. Sometimes it seems that the infection has passed, while it "lurked" in some organs - this can lead to their gradual inflammation, weakening and damage .. - The initial stage of mild sepsis is treated with antibiotics - it responds quickly and well to treatment and has a low mortality rate compared to more severe sepsis with complications (septic shock syndrome), in which death occurs in about 50% of cases.
 3 Note the following symptoms of sepsis while the patient is resting (pulse and respiratory rate should be checked at rest):
3 Note the following symptoms of sepsis while the patient is resting (pulse and respiratory rate should be checked at rest):- high temperature (more than 38.5 ° C), chills are possible;
- or low body temperature, less than 35 ° C, when the patient is warmtrembling is possible;
- low blood pressure;
- rapid heart rate (more than 90 beats per minute);
- rapid breathing (more than 20 breaths per minute), shallow or intermittent breathing;
- probable or confirmed infection.
 4 If you suspect that any symptoms indicate severe sepsis, the patient needs intensive care. If the patient already has signs of mild sepsis and then develops any of the following symptoms of severe sepsis, seek immediate medical attention. These symptoms may indicate severe sepsis requiring intensive care... If the patient has at least one of these signs and symptoms, this may indicate that he has failed any organ (or several organs):
4 If you suspect that any symptoms indicate severe sepsis, the patient needs intensive care. If the patient already has signs of mild sepsis and then develops any of the following symptoms of severe sepsis, seek immediate medical attention. These symptoms may indicate severe sepsis requiring intensive care... If the patient has at least one of these signs and symptoms, this may indicate that he has failed any organ (or several organs): - a sudden, unexplained change in mental state, such as an unusual clouding of consciousness, disorientation in space, dizziness, sudden speech problems, changes in behavior, possible seizures;
- a significant decrease in the amount of urine produced (kidney dysfunction)although it can also be caused by severe dehydration due to persistent diarrhea and / or vomiting, which is also very serious;
- irregular heartbeat, significant change in heart rate;
- abdominal pain (can be caused by damage or failure of the pancreas, kidneys, liver, and other organs);
- labored or labored breathing, unusual tiredness, delirium;
- laboratory tests show a low platelet count: usually platelets are directed by the body to sites of injury or infection to signal and control leukocytes and other cells in inflammatory processes, but in severe sepsis, their concentration begins to fall!
 5 If several of the above symptoms are observed, immediate medical attention and hospitalization are required. Severe cases often require intensive antibiotic treatment over several days or weeks.
5 If several of the above symptoms are observed, immediate medical attention and hospitalization are required. Severe cases often require intensive antibiotic treatment over several days or weeks. - Timely early treatment of worsening sepsis, usually given in a hospital's intensive care unit with antibiotics and large amounts of intravenous fluids, greatly improves the chances of survival and helps prevent blood clots, gangrene, or even septic shock.
Part 2 of 4: Medical Examination and Diagnosis
 1 Diagnosing sepsis can be challenging because the signs and symptoms observed can be caused by other conditions. Often, doctors will order a series of tests and tests to look for the initial infection.
1 Diagnosing sepsis can be challenging because the signs and symptoms observed can be caused by other conditions. Often, doctors will order a series of tests and tests to look for the initial infection. - Various blood tests can help diagnose infection, assess blood clotting, liver and kidney dysfunction, oxygen supply problems, and electrolyte imbalances.
- Tests of other body fluids. Urinalysis can be used to determine the presence of bacteria. Analysis of wound discharge can help determine which antibiotic is best for treatment. Sputum analysis helps to determine which microbe is causing an infectious disease.
- Imaging tests can detect infection-related soft tissue problems in internal organs (lungs, liver, pancreas, intestines, spine, and so on).
Part 3 of 4: Precautions
 1 Be careful. Watch for inflammation and infection. The initial symptoms of sepsis depend on where the infection originated, these may be seemingly minor signs, how:
1 Be careful. Watch for inflammation and infection. The initial symptoms of sepsis depend on where the infection originated, these may be seemingly minor signs, how: - a scratch on the knee, a deep cut with a sheet of paper, a puncture wound from a nail;
- a tampon left without replacement for longer than the prescribed time;
- inflammation can be triggered or exacerbated by stress and the following factors:
- poor nutrition, lack of sleep, overwork;
- smoking, anxiety, anxiety, excess belly fat;
- allergies, pollution and various chemicals.
- a serious infectious disease, for example:
- pneumonia, pulmonary infection;
- an infection in the abdomen can cause sepsis and life-threatening peritonitis;
- renal infection followed by sepsis and possible renal failure;
- infectious blood poisoning, bacteremia - the presence of bacteria in normally sterile blood is a very bad sign ...
 2 Prevention of infections.
2 Prevention of infections.- Get flu and pneumonia shots. These common conditions weaken the immune system and thus increase the risk of sepsis. Vaccination helps prevent them.
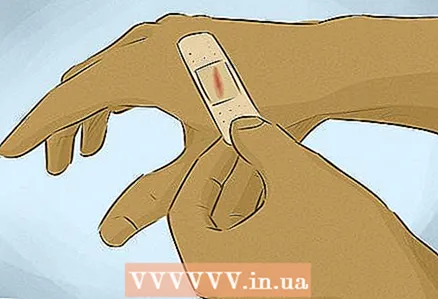
- Rinse, heal, and bandage cuts, stitches, and other injuries well. The infection can even penetrate the blisters with chickenpox.
- Wash your hands regularly. If you, a family member, or a friend is in the hospital, ask all healthcare providers to wash their hands and use new rubber gloves when handling each patient.
- Not use antibiotics to treat the common cold and other mild viral illnesses. This misuse of antibiotics can lead to the development of drug-resistant bacteria, increasing the risk of sepsis.
- Drug-resistant bacteria. Nowadays, many types of bacteria have acquired resistance to the antibiotics that used to kill them. Such drug-resistant bacteria often cause infection, which leads to sepsis.
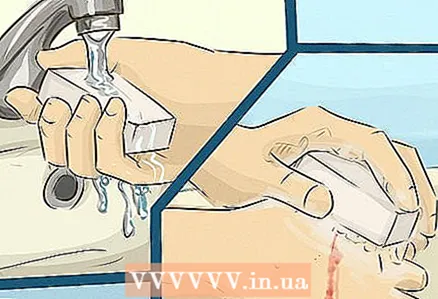 3 To avoid introducing germs, do not touch with unwashed hands:
3 To avoid introducing germs, do not touch with unwashed hands:- cuts, sores, scratched areas of the skin (this will help prevent staphylococcal infection);
- face, mouth, eyes and other openings in the body (this will help prevent infection colibacillus):
- wash your hands before and after going to the restroom after touching doorknobs in public places, and so on.
Part 4 of 4: Risk Factors
 1 Avoid sleep deprivation, overexertion, and fatigue, especially when you are sick or recovering from an illness. Sleep for at least seven hours every night. Lack of sleep lowers immunity.
1 Avoid sleep deprivation, overexertion, and fatigue, especially when you are sick or recovering from an illness. Sleep for at least seven hours every night. Lack of sleep lowers immunity.  2 Consider the following risk factors. Sepsis is more common and is more dangerous for the following categories of people:
2 Consider the following risk factors. Sepsis is more common and is more dangerous for the following categories of people: - in young children and the elderly with weak immunity;
- in people with a weakened immune system - for example, with certain diseases or taking certain medications;
- in seriously ill people, often in the intensive care unit, whose body is weakened by the fight against the disease;
- for wounds and injuries, such as burns;
- in patients with invasive devices, such as intravenous catheters (for IVs or pumps) or breathing tubes, which can cause infection and worsen the body's inflammatory response.
Tips
- The likelihood of tiny blood clots forming during infection can be reduced by taking daily antioxidant supplements as well as the anticoagulants that may have anti-inflammatory propertiese.g. 1/2 aspirin tablet (aspirin not recommended for children). It also helps to strengthen the cardiovascular system and avoid stroke.
- To avoid irritation of the lining of the stomach and esophagus, uncoated non-steroidal anti-inflammatory drugs (NSAIDs) tablets can be dissolved in a spoonful of water (note: this method is useful if you are not using aspirin or ibuprofen tablets with a special coating that prevents them from dissolving in the stomach and thereby reduces irritation of the gastric mucosa and esophagus).
- Drugs such as paracetamol and ibuprofen do not cause Reye's syndrome, but there is a link between this syndrome and aspirin use, especially in children and adolescents. When severe, aspirin-induced Reye's syndrome can lead to cerebral edema, liver problems, coma, and sometimes death, especially in young children.
- Natural anticoagulants slow blood clotting, which can help prevent inflammatory clotting in mild sepsis. In addition, certain foods and herbs, such as grapes, berries, and vegetables, may contain beneficial anti-inflammatory substances (but be careful: in general, very healthy dark green leafy vegetables can speed up blood clotting).because they contain vitamin K), such as tomatoes and peppers, cinnamon, ginger, and so on.
- If you are taking anticoagulants, check with your doctor before using vitamin K supplements or eating dark green leafy vegetables, as they can interfere with blood clotting (for example, when you are taking warfarin or Coumadin, which are derived from coumarins).
- Large blood vessels in the legs and lower torso can form large blood clots if seated for several hours, such as on long flights or long periods of driving, which can lead to deep vein thrombosis, whereby displaced clots can damage the heart and / or lungs:
- Sepsis can cause gangrene if microscopic pieces of dead tissue (i.e., those that not get enough blood, nutrients and oxygen through small capillaries) will increase clots, and as a result, special medications or removal of dead tissue (for example, by amputation of fingers or feet) will be required. Complications caused by the penetration of gangrene into vital organs can be fatal.
- Eat healthy foods, for example, it is best to eat 5-6 small servings of natural foods throughout the day. Not Eat processed foods, refined grains, fats added to crumbly dough, margarine, preservatives, low nutritional value fast foods and fried foods, and avoid pork and meat from other animals that feed on waste, such as bottom dwellers such as catfish and shellfish.
- Exercise and walk more... Consume vitamins, herbs, omega-3 fatty acids (wild-caught cold water fish are a good source of these acids), all B vitamins, vitamins D3 and E, various nuts and seeds (try to eat them every day, especially walnuts, pecans, etc. almond).
- Eat light and dark vegetables (remember that dark green leafy vegetables speed up blood clotting), as well as fruits of various colors (cherries and other berries, melons, and so on) to improve your health.
Warnings
- The risk of sepsis increases with flu, severe colds and other infectious diseases, as well as in the case of diabetes or metabolic syndrome (that is, obesity, high blood pressure and diabetes mellitus). Besides, infants, children, and the elderly may have weak immunity.
- Weak resistance to common infectious diseases means weakened immunity, and this can lead to complications in the form of sepsis (SIR), which is caused by increased inflammation due to the inability to quickly and easily defeat a minor infection.
- After severe sepsis, the risk of future infections may increase as it weakens the body's resistance and immunity.
- Blood thinners (anticoagulants) can cause or increase severe bleeding in some wounds and internal bleeding from ulcers, as well as the likelihood of head injury and hemorrhage in brain tissue. Bleeding may not always be slowed down or stopped with medications such as vitamin K. Not all anticoagulants (with the exception of warfarin) can be interrupted with a large enough dose of vitamin K. After taking some anticoagulants, it is sometimes necessary to resort to measures such as transfusion to stop bleeding squeezing, clamping, applying ice packs, using drugs that constrict blood vessels, and moxibustion, which tightens cuts and lacerations by controlled exposure to heat or burn-causing chemicals, all slow the oozing of blood until the effect of the anticoagulant will stop. Eating lots of dark green vegetables that are rich in vitamin K can also help reverse the effects of warfarin, but not some other anticoagulants.
- Some of the more modern anticoagulants that were released around 2010, not are susceptible to the action of vitamin K, so they can be very dangerous in case of bleeding.