Author:
Peter Berry
Date Of Creation:
19 February 2021
Update Date:
1 July 2024

Content
An ectopic pregnancy is when an egg is fertilized in a place other than the uterus, such as a fallopian tube. An ectopic pregnancy can turn into a serious condition if it is not detected and treated promptly. Therefore, it is essential to identify common symptoms as well as how doctors diagnose and treat ectopic pregnancy.
Steps
Part 1 of 3: Identify the signs of an ectopic pregnancy
Late period. If you are late for your period and have previously had sex without using birth control, get a pregnancy test as soon as possible.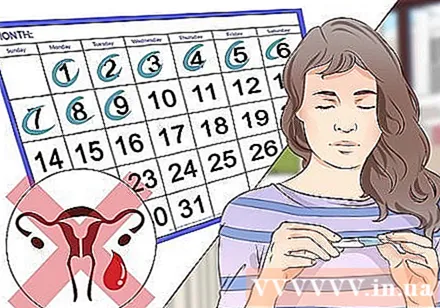
- Even if an ectopic pregnancy does not happen in the uterus, your body will still show signs of pregnancy.
- If you have an ectopic pregnancy, your pregnancy test should theoretically be positive. Note, however, that pregnancy tests can also give false positives or false negatives, so if you have doubts about the results, see your doctor for a blood test.

Look for other signs of pregnancy. During pregnancy, whether an egg is fertilized in the uterus (as usual) or in the fallopian tube or elsewhere (in the case of an ectopic pregnancy), you will experience some or most of the signs. Popular as follows:- tightness in the chest area
- urinating a lot
- nausea, possibly accompanied by vomiting
- no sutra (as stated above).

Lower stomach pain. Lower abdominal pain can be caused by an ectopic pregnancy, whether or not you are determined to be pregnant.- The pain you feel usually occurs when the fetus grows and squeezes other cells, during an ectopic pregnancy, the fetus doesn't have enough space to grow up (for example in the fallopian tube, this is not sites formed to store the fetus).
- Pain in the lower abdomen can be severe, but some women with ectopic pregnancy do not experience it.
- The pain is usually on one side and increases with movement or tension.
- You may also experience shoulder aches as the blood rushed to your lower abdomen stimulates the nerves leading to your shoulder.
- Ligament pain is also very common during pregnancy. Similar to lower abdominal pain, the pain can be on one or both sides and usually comes in waves (each lasting for a few seconds). Ligament pain most often appears in the second trimester. Whereas lower abdominal pain usually occurs in the early part of pregnancy.

Note when vaginal bleeding. When the fallopian tube is stretched or stretched can cause mild bleeding, the bleeding will get worse as the fetus grows to a certain point, at which point the fallopian tube can rupture. Bleeding during pregnancy is a sign that you need to see your doctor, especially if the bleeding is heavy or constant, in which case you need to get emergency medical help as soon as possible.- Heavy bleeding from fallopian tube rupture (which can occur during ectopic pregnancy) can lead to severe blood loss, fainting and, although very rarely, death if not treated promptly.
- In addition to bleeding, you should be on the lookout for some serious signs that need to be addressed promptly, such as severe abdominal pain, feeling light-headed, dizzy, sudden pale, or psychotic.
- Note, "implantation bleeding" is a perfectly normal sign of pregnancy. Implantation bleeding usually occurs about 3 weeks after your last menstrual period with a pink / light brown discharge, you will need a few tampons from the start of the bleeding to the end. Hemorrhage from ectopic pregnancy usually occurs after an egg has implanted and begins to develop in a confined space and is insufficient for further development of the fetus.
- Immediately go to the medical facility to check if you experience heavy bleeding with pale color, lasting more than a day.
Part 2 of 3: Diagnosis of an ectopic pregnancy
Consider the risks of ectopic pregnancy you may face. If you are experiencing any of these symptoms, see if you are at high risk of an ectopic pregnancy. There are certain factors that can cause a woman to have an ectopic pregnancy.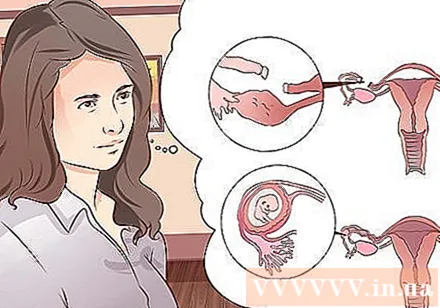
- In general, people with a history of ectopic pregnancy have a higher risk of ectopic pregnancy.
- Other risk factors include: pelvic infections (sexually transmitted infections), having multiple sex partners (as this increases your risk of getting sexually transmitted infections), having abnormalities or tumors. in the fallopian tubes, have undergone lower abdominal or pelvic surgery, IUD insertion, endometriosis or smoke.
- Although tubal ligation is very effective in preventing pregnancy, once an egg has been fertilized, a person who has had this surgery is at a much higher risk of an ectopic pregnancy than usual.
Blood test for β-HCG levels. This is the first step that should be taken in diagnosing an ectopic pregnancy.
- β-HCG is a hormone secreted by the development of the egg and placenta, so levels of this hormone increase as pregnancy continues and is a reliable measure of pregnancy testing.
- If an ultrasound shows no signs of an embryo and the β-HCG level in your blood is higher than 1500 IU / L (usually the level of suspicion is between 1500-2000 IU / L), the doctor will hypothesize. problem with ectopic pregnancy. This is because the β-HCG levels of ectopic pregnancy are often higher than in normal pregnancies.
- If an ectopic pregnancy is diagnosed based on β-HCG levels, the doctor will perform a probe ultrasound to find the embryo and its location.
Vaginal transducer ultrasound. Transvaginal transvaginal ultrasound can identify 75 - 85% of ectopic pregnancies (ie 75-85% of cases where the embryo can be detected and the location of the embryo).
- It should be noted that a negative ultrasound does not completely rule out an ectopic pregnancy. But on the contrary, just a positive ultrasound result (that is, it is confirmed whether the fetus is in the fallopian tube or somewhere other than the uterus) is enough to make a conclusion for the diagnosis.
- If the ultrasound is negative (ie, no conclusion is reached), but the β-HCG level remains high with suspicious symptoms, the doctor may perform a "laparoscopic diagnosis". , that is, a very small incision will be made to place a camera in the lower abdomen to obtain clearer images.
Accept laparoscopic diagnosis. If the blood test and ultrasound are not enough to reach a definitive conclusion and the possibility of you having an ectopic pregnancy persists, your doctor may perform an endoscopic diagnosis to look at the pelvic area and lying organs. in the lower abdomen to see if there are signs of implantation.
- Laparoscopic diagnosis can last from 30 minutes to 1 hour.
Part 3 of 3: Treatment of ectopic pregnancy
Get treatment as soon as possible. Once you have been determined to have an ectopic pregnancy, your doctor will recommend the earliest possible treatment because early treatment of your ectopic pregnancy will have more positive results. At the same time, it is impossible for a fetus to not implant in the uterus to "survive" towards the end of pregnancy, so treat it as soon as possible to avoid possible complications ( may be life-threatening if an ectopic pregnancy is not removed early).
Use medications to stop the growth of the fetus. The most common drug in this case is methotrexate. This drug is given into the body by intramuscular injection once or several times depending on the amount of medication needed to remove an ectopic pregnancy.
- After you have been injected with methotrexate, you will have a blood test to determine your β-HCG levels. Treatment is considered successful when the β-HCG level falls near zero (no detection on blood tests); otherwise, you may be given more methotrexate until the β-HCG level is near 0, if medication cannot be used to control fetal growth, you may need surgery.
Surgery to remove an ectopic pregnancy. During surgery, the doctor may try to save the affected part of the fallopian tube, or may also remove that part if necessary. Surgery is indicated when:
- Pregnant women lose too much blood, need urgent treatment.
- Failure to treat with methotrexate.