Author:
Louise Ward
Date Of Creation:
8 February 2021
Update Date:
1 July 2024

Content
One in eight women is affected by breast cancer, a disease that ranks second only to skin cancer in the number of cases diagnosed with cancer each year. This disease is also the second leading cause of death from cancer, after lung cancer. Although the risk is lower than that of women, men can also be diagnosed with breast cancer. A family history of breast cancer is especially important for you to be proactive and watch for any breast changes. Early recognition and detection of the disease will increase the patient's chances of success in treatment and survival.
Steps
Part 1 of 3: Raising awareness about breast cancer
Understand how research has changed about the effectiveness of breast self-examination. In the past, the monthly self-examination of breast (BSE) was recommended for all women. However, in 2009, after many important studies were published, the American Preventive Services Task Force issued a recommendation to instruct women to do breast self-exams. These studies concluded that BSE did not reduce mortality or increase the number of cancer cases detected.
- As recommended by the American Cancer Society and the American Preventive Services Task Force, BSE should be done according to the wishes of women and they should be aware of BSE's limitations. Perhaps the main thing these organizations want to emphasize is that women should know what normal breast tissue is.
- In other words, BSE cannot (and should not) take the place of an examination of the clinic for abnormalities. However, BSE can help you better understand the normal state of the breast, so you will be able to assist your doctor in detecting changes. BSE should never be used as a substitute for a medical institution breast examination performed by a physician.

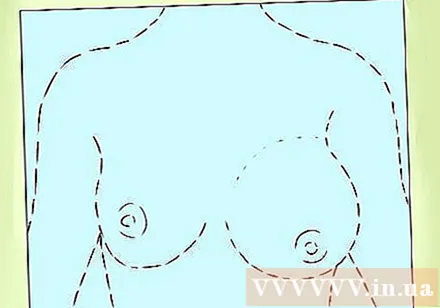
Visual observation. You can do this whenever you want, although the best time to check is after your period, when your breasts are less tight and swollen. Try to do it at the same time every month. Sit or stand in front of a mirror, undress and bra. Arms raised and lowered. Observe the size, shape, tension, and appearance of the breast tissue as well as the surrounding area, especially in the armpit. Changes may include:- The skin is concave and wrinkled like an orange peel (also known as peau d’orange).
- New red streaks or a scaly rash
- Unusual swelling or tenderness.
- Nipple changes, such as retraction, itching, or redness.
- The discharge from the nipple may be colorless, yellow or bloody.

Check by hand. The ideal time to check is during menstruation, when the breasts are least stretched, usually a few days before the end of your period. You can do this by lying down to spread the breast, making the breast tissue thinner and easier to touch, or you can also check in the shower, as soap and water help the fingers to move easily. easier on breast skin. Follow these steps:- Lie on your back with your right hand behind your head. Use the first three fingers of the left hand to feel the right breast tissue. Remember to use the underside of your fingers, not just the tips of your fingers.
- Use three different pressures to examine the breast in three parts: the part just below the skin, the middle part of the breast, and a little more pressure to manipulate the breast tissue close to the chest. Make sure to apply pressure to each area before moving to another area.
- Begin testing along an imaginary line that runs along the side, starting at your armpits and moving with an up and down movement. Start from the collarbone down until it reaches the ribs. Move in the middle until you feel the sternum. It is important to examine the entire breast, so try to feel in order.
- Next, place your left hand under your head and do the same test with the left breast.
- Remember that the breast tissue extends to an area close to the armpit. This is commonly known as the breast base and often develops a lump or cancer.

Get to know your breasts. Know what your breasts look and feel. Become familiar with the texture, line, size, etc. so that you can better communicate with your doctor.- Encourage your spouse to talk to you about changes he may notice. Your partner may notice breast tissue changes that you can ignore because they see your body from a different angle.
Know your risk factors. Some people have a higher risk of breast cancer than others. It should be noted that, even if you fall into one or more of the following situations, it is not certain that you will develop breast cancer; however this really shows that you should pay more attention, regular hospital breast exams and mammograms. Some of the factors that indicate a high risk include:
- Sex: Women are more likely to develop breast cancer than men.
- Age: The risk of breast cancer increases with age. The majority of women with breast cancer are over the age of 45.
- Periods: If you started menstruating before age 12 or entered menopause when you were over age 55, your risk is slightly higher.
- Pregnancy and lactation: Get pregnant early or get pregnant multiple times and breastfeeding can lower your risk of breast cancer. Women who do not have children or become pregnant past the age of 30 have an increased risk of developing breast cancer.
- Lifestyle factors: Obesity, smoking, and alcohol use are all risk factors for breast cancer.
- Hormone replacement therapy (HRT): Having and used to use hormone replacements increases the risk of breast cancer. However, this is controversial, with many for and against, so it's best to talk to your doctor about your personal risks, other options, and monitoring.

Know your personal and family medical history. In addition to the above factors, there are also risk factors associated with the individual, family history, and genetics, including:- Personal medical history: If you have been diagnosed with breast cancer in the past, the cancer cells are more likely to return in that breast or the other breast.
- Family history: You are more likely to get breast cancer if one or more family members have breast cancer, ovarian cancer, uterine cancer, and colon cancer. Your risk doubles if you have a first-class relative (sister, mother, daughter) who is sick.
- Genes: Genetic defects found in the BRCA 1 and BRCA 2 genes can significantly increase the risk of developing breast cancer. You can use a genetic mapping service to know if you have these genes. In general, 5-10% of cases are related to genetic factors.
Part 2 of 3: Recognize typical symptoms
Watch for changes in breast size and shape. Swelling caused by a tumor or infection can deform and change the size of the breast tissue. This change usually occurs on only one breast, but can also occur on both sides.
Note any unusual discharge from the nipple. If you are not breastfeeding at the moment, there will be no discharge. If your nipples are releasing discharge, especially if you're not squeezing your nipples or breast tissue, see your doctor for further testing.
Watch for swelling. Pay special attention to swelling around the breast, collarbone, or armpit. Some invasive forms of breast cancer can cause swelling in these areas before you can feel a lump in the breast tissue.
Watch for protrusions in breast tissue or change in nipples. Lumps in the breast near the skin surface or near the nipple can change tissue shape.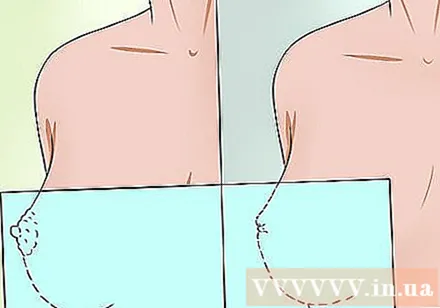
- In some cases, the nipple will sink in or you may notice a protrusion of the skin above the breast tissue.
Tell your doctor about thick, red, hot, or itchy skin. Although rare, inflammatory breast cancer is a particularly invasive and progressive cancer. Symptoms of this type of cancer may appear similar to those of mastitis, such as a warm, itchy, or red sensation in the tissue. If the antibiotic does not cure the condition quickly, you should see your breast surgeon as soon as possible.
Note that pain is not normal. If you experience pain in the breast tissue or nipple area and does not go away quickly, seek medical attention. Breast tissue is normally painless, and pain can indicate an infection, a lump or a tumor. However, breast pain is usually not a sign of cancer.
- Remember that if you are menstruating or pregnant, you may experience temporary breast pain, discomfort, and tightness due to hormone changes. However, if you experience pain that is persistent and unrelated to your menstrual cycle, you should still consult your doctor.
Recognize the signs of metastatic breast cancer. Remember that these signs do not necessarily mean you have breast cancer. However, they do show that you need to see your doctor for further examination. These symptoms include:
- Weight loss
- Bone pain
- Rapidly breath
- A boil in the breast, which is a painful area that may be red, itchy, and drain pus or clear fluid.
Part 3 of 3: Breast cancer screening
Get a specialist breast exam. When you go for a yearly checkup or pelvic exam, ask your doctor to do a manual breast exam for lumps or other suspicious changes. Doctors are trained in examining the breast and will know what to look for. That is why you should never try to do a breast self-examination for a doctor, even if you feel uncomfortable and embarrassed.
- The doctor will examine the outside of the breast. You will be asked to raise your hands to your head and then drop your arms down your sides as the doctor examines the size and shape of your breasts. Then you will have a physical exam. When you lie on the examination table, the doctor will use your finger to examine the entire breast area, including the armpits and collarbones. One visit only lasts a few minutes.
- If you feel uncomfortable, you can have a nurse or family member present in the room during the doctor's visit. If you are female and the doctor is male then this is required in most cases. If you feel nervous, take a deep breath and tell yourself that this is a necessary part of taking care of your health.
Mammogram. A mammogram uses low-radiation X-rays to check breast tissue, and can usually detect lumps before you can feel them. The National Breast Cancer Institute recommends women 40 years of age and older get screening mammograms every year or two. Women under 40 years of age but with high risk factors should consult a doctor about the frequency of mammograms. Even without risk factors or symptoms, you should still have a mammogram every few years as part of your health care regimen.
- During a mammogram, the breasts are placed on a flat surface, pressed down so that the breast tissue is evenly spread and low-energy X-rays are allowed. You will feel some pressure and discomfort, but this is only temporary. The scan is done in both breasts so the radiologist can compare the sides.
- In addition to detecting potentially cancerous tumors, the doctor also checks for calcification, fibroids and cysts with X-ray mammograms of the breast.
Get more tests if you notice lumps or other suspicious changes. If you or your doctor notice a lump or any other warning signs, such as nipple discharge or wrinkled skin, you may need additional tests to find the cause and determine if you are have breast cancer or not. These tests may include:
- Diagnostic mammograms: X-ray images of the breast that can evaluate the tumor. The scan can take longer than the screening mammogram to take because more pictures are needed.
- Supersonic: Ultrasound waves are used to show an image of the breast. This technique is most effective when combined with a mammogram. Despite the advantages of being simple and non-invasive, ultrasound can give many false positives and negatives. However, this technique is often used very effectively in needle biopsy guidance for a suspected tumor.
- Magnetic resonance imaging (MRI): This technique uses a magnetic field to image the breast. You may need an MRI if a diagnostic mammogram cannot identify a tumor or tumor. This technique is also commonly recommended for women at a very high risk of developing breast cancer, for example women with a family history or genetic predisposition to breast cancer.
Do a biopsy. If mammograms and MRI detect lumps or lumps, your doctor may recommend an ultrasound guided biopsy to determine the type of cancer cell and the required surgical or chemotherapy procedure. . During a biopsy, a very small piece of tissue is removed from the suspicious area of the breast and analyzed. This procedure is usually done with a relatively large needle through the numbed skin. Most breast tissue biopsies are outpatient, and you don't need to stay in the hospital overnight. Only in the case of lumpectomy, local anesthesia is needed.
- A tissue biopsy is necessary before selecting a treatment to determine the nature of the cancer. Although the biopsy may seem frightening, and indeed frightening, this test is important to know if the cells in the breast tissue are cancerous and then to determine a treatment regimen. The earlier breast cancer is detected, the higher the survival rate.
- It is important (and very encouraging!) That 80% of women who have a breast biopsy do NOT find breast cancer.
Wait for results. Waiting time for the test results and biopsy can be very stressful and anxious. People deal with this time in many different ways. Some people want to distract themselves with fun activities and keep busy. Others find it helpful during this time to research breast cancer and find out about any treatment options if the diagnosis is positive. Some people also use waiting time to rethink their lives and define (or redefine) their priorities and relationships.
- Get plenty of exercise and eat healthy to stay energized and uplifting. Seek social support from friends, co-workers or family members who have experienced similar situations and can provide helpful advice.
- If you feel so obsessed, overwhelmed, or depressed that your mind and body are at risk of a breakdown, you should let your doctor know. You may need to contact a mental health professional or counselor to talk about your feelings while waiting for your diagnosis.
Advice
- One of the best things you can do for yourself is to better understand what is normal breast tissue condition. This way you will be able to determine if something is "not good".
- Practice freely talking about your health with your doctor and family. This is something you will have to do more and more, especially as you get older. Taking care of your overall health with good nutrition, regular activity and stress management can reduce your risk of many diseases, including cancer.
Warning
- See your doctor for a diagnosis. You cannot diagnose breast cancer at home. Therefore, before you get too nervous or confused, find the answers you need and make the right decisions.
- If you are not satisfied with your doctor's answer, please seek other opinions. It's your body and your life. Listen to inner voices about your health, and it's important to find another opinion.