Author:
John Stephens
Date Of Creation:
24 January 2021
Update Date:
29 June 2024

Content
A mental health treatment plan is a document that specifically documents a client's current mental health problem and outlines the client's goals and strategies to help them overcome this problem. In order to obtain the necessary information for the treatment plan, the staff should interview the client. Information collected during the interview will be written into the treatment plan.
Steps
Part 1 of 3: Conducting a Mental Health Assessment
Collect information. Psychological assessment is the process of gathering information when a mental health worker (counselor, therapist, social worker, psychologist or psychiatrist) interviews a client about a psychological issue. Present and past, family history and social problems in current and past work, school and relationships. Psychosocial assessments can check if you have recently abused medications or used psychiatric drugs.
- Mental health staff may consult client's medical and mental health records during the psychological assessment. Do not forget to sign a statement regarding the disclosure of personal information.
- Be sure to clearly explain the security limitations. Let the customer understand that what you say is confidential, but there will be exceptions if the customer intends to harm himself or others, or becomes aware of abuse in the community.
- Be willing to stop the evaluation if the client is in a panic. For example, if the client intends to commit suicide or kill someone, you need to change tactics and intervene in the crisis immediately.
Follow each step of the evaluation process. Most mental health facilities provide assessment forms for staff to fill out during the interview process. Here's an example of how to hit your mental health (steps in order):- Referral reason
- Why do customers come for treatment?
- How are they introduced?
- Current symptoms and behavior
- Depressed mood, anxiety, taste changes, sleep disturbances, etc.
- Anamnesis
- When did the disease start?
- The intensity / frequency / duration of the disease?
- Have you made an effort to solve the problem of the disease? If yes, what?
- Weakness in everyday life
- Trouble at home, at school, at work, in relationships.
- Psychological / psychiatric history
- Such as previous treatments or hospitalizations.
- Concerns about risks and safety at the present time
- Having thoughts of harming yourself and others.
- If the patient arouses the above concerns, immediately stop the evaluation and proceed with crisis intervention procedures.
- Current and previous prescription, psychological and medical conditions
- Include the name of the medication, the dose, the length of time the medication was taken, and whether or not to be prescribed.
- Pre-use of stimulants
- Alcohol and drug abuse.
- Family circumstances
- Socio-economic level
- Parents' occupation
- Parental marital status (married / separated / divorced)
- Cultural circumstances
- Emotional / medical biography
- Relationship in the family
- Biographies of individuals
- New-born - Developmental milestones are closely related to parents, toilet training, early medical history.
- Early and mid-childhood period - change in school, academic performance, friendships, interests / activities / interests.
- Adolescence - Early dating, puberty reaction, manifestation of rebellion.
- Early and mid-adulthood - career / career, satisfaction with life goals, personal relationships, marriage, economic stability, medical / emotional history, relationship with parents.
- Late adulthood - medical history, response to possible decline, economic stability
- Mind status
- Personal appearance and hygiene, speech, mood, impact, etc.
- Other features
- Self-concept (likes / dislikes), happiest / saddest memories, fear, first memories, memorable / repetitive dreams
- Summarize and point out first impression
- Write a brief summary of the patient's problems and symptoms in narrative format. In this section, the counselor can observe the patient's response during the assessment.
- Diagnose
- Use the collected information to fill out a diagnostic form (DSM-V or description)
- Recommendations
- Receiving therapy, referring to a psychiatrist, treating with drugs, etc. This is the next step after a clinical diagnosis. Effective treatment will help you get better.
- Referral reason

Pay attention to your behavior. Counselors conduct a summary mental health test (MMSE) related to the client's appearance and how they interact with employees and other customers at the facility. The therapist can make decisions depending on the client's mood (sadness, anger, indifference) and influence (emotional expression, ranging from being open, expressing many emotions to monotonous. , do not show emotion). Observation helps the counselor make the appropriate diagnosis and treatment plan. Here are some of the things you should look for when doing the mental state test:- Appearance and level of hygiene (clean or sloppy)
- Eye contact (elusive, little, or normal)
- Nerve motor (calm, nervous, rigid, or agitated)
- Speech (soft, loud, pressured, tongue twitching)
- Communication style (stimulating, sensitive, cooperative, silly)
- Orientation (whether or not customer knows current time, date and situation)
- Intellectual function (intact, impaired)
- Memory (intact, weakened)
- Mood (normal, irritable, about to cry, anxious, depressed)
- Effects (consistent, unstable, weakening, tedious)
- Sensory disturbances (hallucinations)
- Disorders of thinking processes (concentration, assessment, insight)
- Disorder content of thoughts (delusions, phobias, suicidal thoughts)
- Behavioral disturbances (anger, impulse control, demanding)
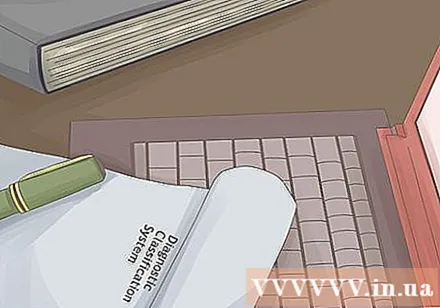
Make a diagnosis. Diagnosis is crucial. Sometimes a client will receive multiple diagnoses such as Depressive Disorder and Alcohol Abuse. A diagnosis should be made before completing a treatment plan.- Diagnosis is made based on the client's symptoms and compliance with the criteria outlined in the DSM. The DSM is the diagnostic classification system created by the American Psychiatric Association (APA). Use the latest version of the DSM-5 to give an accurate diagnosis.
- If you don't have a DSM-5, you can borrow a boss or colleague. Do not rely on online sources to make a diagnosis.
- Use client's routine symptoms to make a diagnosis.
- If you are unsure of the diagnosis or need professional help, speak with your supervisor or consult an experienced doctor.
Part 2 of 3: Goal Development
Determine possible goals. After completing an initial assessment and making a diagnosis, you need to think about treatment interventions and goals. Often times, clients need help setting goals so it's better to prepare them before discussing them with them.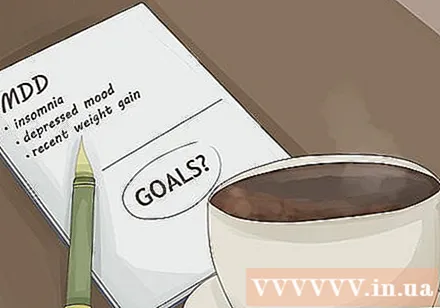
- For example, if a client is diagnosed with Depressive Disorder (MDD) the goal should be symptom relief of MDD.
- Think about a viable goal for your client's symptoms. For example client suffers from insomnia, depressed mood and weight gain (symptoms of MDD). You can create separate goals for outstanding issues.
Think about interference. Intervention is key to change in treatment. Therapeutic intervention is what will change your client.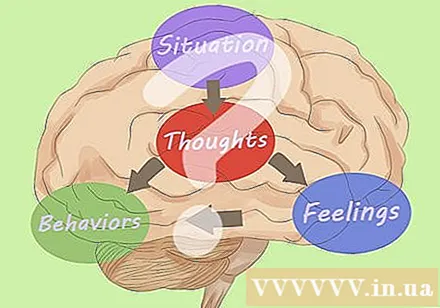
- Defining treatment methods, interventions, such as: activity scheduling, cognitive-behavioral therapy, cognitive restructuring, behavioral testing, homework assignments, skills instruction deal like relaxation, meditation and grounding.
- Make sure to comply with what you know. Part of the therapist's ethics is that you act within authority without harming the patient. Do not try to use a therapy that you have not trained in unless you are under the supervision of a specialist.
- If you are new, use a reference book of the therapies you use. They will keep you on the right track.
Discuss your goals with your customers. After making the initial assessment, the therapist and client proceed to set appropriate goals for the treatment. You need to discuss this before making a treatment plan.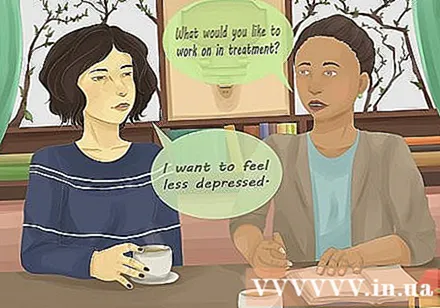
- Treatment plan includes direct client feedback. Together, the counselor and client decide on the goals set in the treatment process and the strategies used to achieve them.
- Ask the client what they need during treatment.It could be: "I want to relieve depression." Then, you can come up with suggestions for appropriate goals to alleviate their depression symptoms (such as doing cognitive-behavioral therapy CBT).
- Try to use an online form to set goals. You can ask your customers questions:
- What do you look forward to when attending therapy? What would you like to change?
- What do you need to do to achieve your goal? Suggestions and give ideas if customers have problems.
- On a scale of 0 to 10, 0 means nothing and 10 is completely achieved, what level do you want to achieve? This helps you ensure the fitness of your goals.
Set out specific treatment goals. The goal of treatment determines the type of treatment. The goal also determines most of the treatment plan. You can use the SMART goal approach: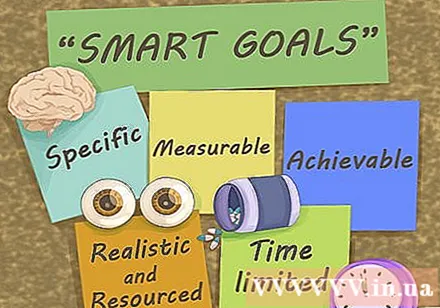
- Specific (specific) - Set out as clear as possible goals, such as reducing the severity of depression, including reducing nighttime insomnia.
- Measurable - How do you know when you are accomplishing your goal? Make sure you can quantify it, eg reduce your depression level from 9/10 to 6/10. Or reduce insomnia from 3 nights to 1 night per week.
- Achievable (doable) - Ensuring the rationality of the goal. For example, alleviating insomnia from 7 nights to 0 nights weekly is a difficult goal to achieve in the short term. Consider changing to 4 nights per week. After you have reached your 4-night goal, you can set a goal to eliminate insomnia completely.
- Realistic (realistic) - can you complete the goal with current resources? Do you need any help to achieve your goal? How do you access resources?
- Time-limited - Set a time limit for each goal, such as 3 months or 6 months.
- The full goals look like this: Alleviate the client's insomnia symptoms from 3 nights to 1 night per week for 3 months.
Part 3 of 3: Treatment Planning
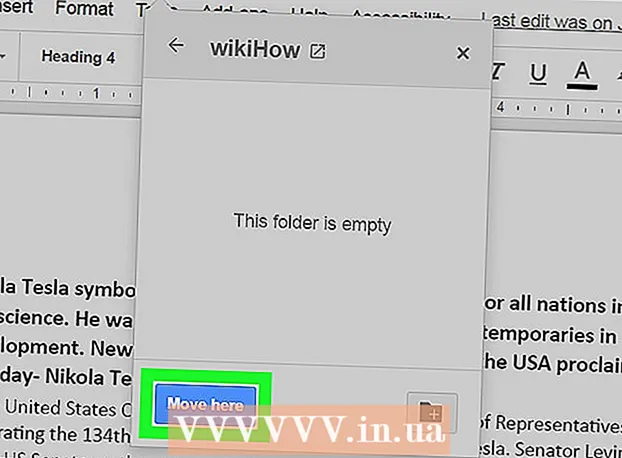
Record each part of your treatment plan. The treatment plan includes goals that the counselor and therapist decide. Many facilities have a treatment plan form available, and counselors simply need to fill it out. Part of the form is to check the line corresponding to the client's symptom. The basic treatment plan includes the following information:
- Customer name and diagnosis.
- Long-term goals (eg client states "I want to cure my depression.")
- Short-term goal (Mitigate insomnia from 8/10 to 5/10 in 6 months). A perfect treatment plan needs at least 3 goals.
- Clinical intervention / Type of service (individual, group therapy, cognitive-behavioral therapy, etc.)
- Commitment of customers (things the client agrees to do, such as once a week therapy, completing home therapy exercises, practicing coping skills learned during treatment)
- Date and signature of therapist and client
Record your goals. The goal should be as clear and concise as possible. Keep in mind your SMART plan and set specific, quantifiable, achievable, realistic, and time-limited goals.
- You can record each target individually or concurrently with that target's intervention and customer consensus.
Demonstrates the specific intervention you use. The counselor will write the treatment strategy the client chooses. The therapies used to accomplish this goal could be covered in this section, such as personal or family therapy, detoxification, or drug use management.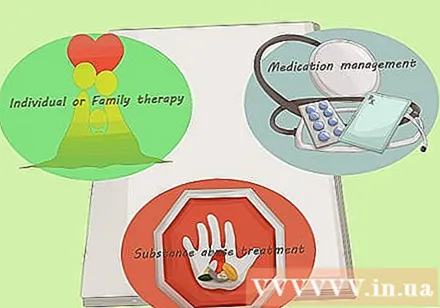
Sign a treatment plan. The client and counselor sign the treatment plan to show consent for treatment.
- Make sure to sign for confirmation right after completing the plan. You want the form date to be accurate to represent the client's consent in the treatment plan's goal.
- If the treatment plan is not endorsed, the insurance company may not pay for the services performed.
Review and adjust if needed. Maybe you will accomplish goals and set new goals during the client's treatment. The treatment plan should include the date on which the counselor and client review treatment progress. Decisions to continue with the current treatment plan or to change to another plan will be made at that time.
- Maybe you want to check your goals weekly or monthly to determine progress. You might ask, "How many times have you lost sleep this week?". After the client reaches his or her goal of just one night of sleep a week, you can move on to a different goal (either completely eliminating insomnia or improving sleep quality).
Advice
- The treatment plan is documentary that can be changed according to the needs of the client.
What you need
- Evaluation form or table
- Medical and mental health notes
- Treatment plan form or table