Author:
Judy Howell
Date Of Creation:
4 July 2021
Update Date:
1 July 2024

Content
- To step
- Method 1 of 2: Treating a minor ice burn at home
- Method 2 of 2: Medical treatment for a severe ice burn
- Tips
- Warnings
Ice burns are burns to the skin caused by extreme cold instead of heat. If you've been exposed to high altitudes and freezing winds, or have been in direct contact with a frozen object and are experiencing symptoms, you've likely suffered an ice burn. If you have the symptoms of a mild skin frostbite, such as mild skin discoloration, numbness, itching, tingling, or pain, you can treat your ice burn at home. To treat the symptoms of a severe skin frostbite, such as blistering, long-term numbness and / or skin discoloration, or infection, seek medical attention as soon as possible.
To step
Method 1 of 2: Treating a minor ice burn at home
 Remove the frozen item from your skin. If you think you have an ice burn, immediately remove the source of cold that is in direct contact with your skin. If you have an ice burn from high altitude and / or exposure to freezing wind, move to a lower area as soon as possible and cover your skin as soon as it is safe to do so.
Remove the frozen item from your skin. If you think you have an ice burn, immediately remove the source of cold that is in direct contact with your skin. If you have an ice burn from high altitude and / or exposure to freezing wind, move to a lower area as soon as possible and cover your skin as soon as it is safe to do so.  Remove all wet or cold clothing. Once you have removed / neutralized the cause of your burn, take off any wet or cold clothing that could prolong your exposure to the cold. The goal is to return your body, especially the affected area, to a normal temperature as soon as possible.
Remove all wet or cold clothing. Once you have removed / neutralized the cause of your burn, take off any wet or cold clothing that could prolong your exposure to the cold. The goal is to return your body, especially the affected area, to a normal temperature as soon as possible. 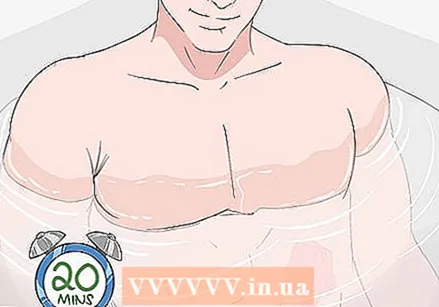 Immerse the burned area in warm water for 20 minutes. To treat your ice burn, pour warm (but not boiling!) Water into a bathtub, plastic container, or large saucepan. The water should be between 37 and 40 degrees Celsius. Immerse the affected skin area in the warm water and let it soak for 20 minutes, without taking it out.
Immerse the burned area in warm water for 20 minutes. To treat your ice burn, pour warm (but not boiling!) Water into a bathtub, plastic container, or large saucepan. The water should be between 37 and 40 degrees Celsius. Immerse the affected skin area in the warm water and let it soak for 20 minutes, without taking it out. - Avoid using water above 40 degrees, as that can actually make the ice burn worse.
- While your skin is immersed in the warm water, you may experience a stinging sensation. This indicates that your skin is thawing and the feeling is returning.
 Do not soak the frozen body part for more than 20 minutes. Remove it from the warm water after 20 minutes and let the skin warm up again for another 20 minutes. This will give your skin time to return to its normal temperature.
Do not soak the frozen body part for more than 20 minutes. Remove it from the warm water after 20 minutes and let the skin warm up again for another 20 minutes. This will give your skin time to return to its normal temperature. - If you notice that your burn is improving and the pain has subsided 20 minutes after you stop soaking, you may not need to repeat the soaking in warm water.
- Around 20 degrees Celsius is generally considered to be room temperature. If you don't have a room at room temperature, cover your burn loosely with a blanket or extra clothing.
 If your skin still feels cold, repeat the soaking in warm water. If you still have frostbite symptoms after 20 minutes at room temperature, reheat the water and soak the affected body part in warm water for an additional 20 minutes.
If your skin still feels cold, repeat the soaking in warm water. If you still have frostbite symptoms after 20 minutes at room temperature, reheat the water and soak the affected body part in warm water for an additional 20 minutes. - After repeating the 20-minute warm water treatment one more time, wait another 20 minutes before moving on to the next step.
- If after a second week and 20 minutes of rest your symptoms are still not resolved, contact your doctor or go to the ER immediately.
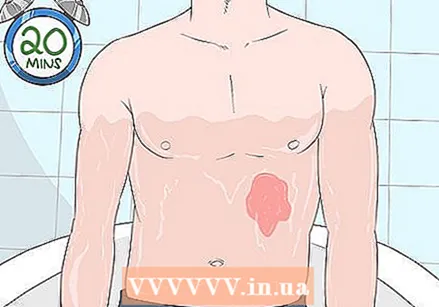
 Apply a warm compress for about 20 minutes. If your symptoms start to subside after 1-2 weeks with warm water, but your skin is still a little numb or cold, gently apply a warm compress to the burned area. Keep the compress on the burn for about 20 minutes. You can use a hot water bottle as a compress or a washcloth that you have held under warm running water for a while.
Apply a warm compress for about 20 minutes. If your symptoms start to subside after 1-2 weeks with warm water, but your skin is still a little numb or cold, gently apply a warm compress to the burned area. Keep the compress on the burn for about 20 minutes. You can use a hot water bottle as a compress or a washcloth that you have held under warm running water for a while. - If putting a warm compress on the burn hurts, gently wrap a warm blanket around you instead so that the burn is warm and covered.
 Remove the compress so that your skin can return to its normal temperature. After holding the compress on your ice burn for about 20 minutes, remove it. Allow your skin to relax at room temperature until the affected area has returned to normal body temperature.
Remove the compress so that your skin can return to its normal temperature. After holding the compress on your ice burn for about 20 minutes, remove it. Allow your skin to relax at room temperature until the affected area has returned to normal body temperature.  Use aloe vera ointment if the frozen skin is not cracked or otherwise damaged. Apply the aloe vera ointment generously to the affected skin at least 3 times a day. This can soothe the burn and shorten recovery time by helping the skin to retain moisture.
Use aloe vera ointment if the frozen skin is not cracked or otherwise damaged. Apply the aloe vera ointment generously to the affected skin at least 3 times a day. This can soothe the burn and shorten recovery time by helping the skin to retain moisture. - Aloe vera can also help your skin make new cells more quickly.
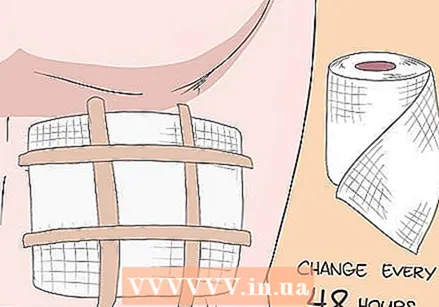 Cover the burn loosely with some gauze bandage. To protect the burn from bacteria or other contaminants, cover the affected area with some gauze, held in place with bandage tape. Be careful not to tape the gauze too tightly so that your burn can still "breathe".
Cover the burn loosely with some gauze bandage. To protect the burn from bacteria or other contaminants, cover the affected area with some gauze, held in place with bandage tape. Be careful not to tape the gauze too tightly so that your burn can still "breathe". - To keep the wound clean, you need to change the gauze at least every two days. When changing the gauze, you can gently clean the burn with some lukewarm water and reapply aloe vera if necessary.
- Keep your burn covered until it is almost completely healed and the pain is gone.
- Minor ice burns should be completely healed within 2 weeks.
Method 2 of 2: Medical treatment for a severe ice burn
 If the frostbite symptoms are severe, get yourself treated by a doctor. Check your ice burn for symptoms of a severe ice burn and see a doctor immediately if you have such symptoms. Common symptoms of a severe frostbite include skin cracks or blisters, a white, gray, or yellowish skin tone that does not fade even after your skin has warmed up, and / or numbness, extreme cold, or hardening even after heating.
If the frostbite symptoms are severe, get yourself treated by a doctor. Check your ice burn for symptoms of a severe ice burn and see a doctor immediately if you have such symptoms. Common symptoms of a severe frostbite include skin cracks or blisters, a white, gray, or yellowish skin tone that does not fade even after your skin has warmed up, and / or numbness, extreme cold, or hardening even after heating. - In very severe cases, you can also no longer use the muscles in the affected area.
- You may also show signs of an infection such as pus or green discharge, fever and / or increasing pain.
- While minor ice burns can sometimes blister or crack, this is usually a sign that the ice burn is serious. Even if your ice burn is not that severe, cracks and / or blisters can make it difficult to properly clean and care for the wound. Therefore, if your wound is open, you should always seek medical attention, regardless of its cause or severity.
 If you have frostbite symptoms, go to the ER. If your skin turns black or blue, or if you have severe pain that penetrates deep into your body, you may also have frostbite and should seek immediate medical attention. The difference between an ice burn and a frostbite is often very subtle. While an ice burn causes a painful burn to the surface of your skin, frostbite occurs when both your skin and the tissue beneath it freeze and become damaged.
If you have frostbite symptoms, go to the ER. If your skin turns black or blue, or if you have severe pain that penetrates deep into your body, you may also have frostbite and should seek immediate medical attention. The difference between an ice burn and a frostbite is often very subtle. While an ice burn causes a painful burn to the surface of your skin, frostbite occurs when both your skin and the tissue beneath it freeze and become damaged. - Although with both ice burns and frostbite, the skin can turn white, red, or pale yellow, generally only with a frostbite your skin turns blue or black.
- Do not reheat frozen tissue if there is a chance it will freeze again before reaching the ER.
- Do not rub the frozen area as this can cause further tissue damage.
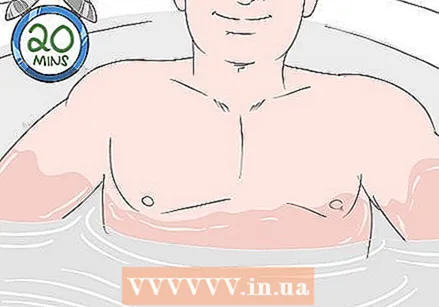
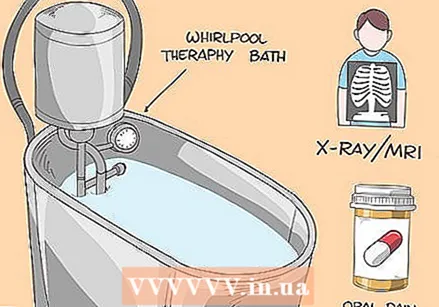 Get treatment for your specific symptoms. The treatment your doctor will give you will depend on the severity of the ice burn, the symptoms you have, and whether you also have frostbite. In most cases, your doctor will start by rewarming the skin using a 20-minute warm water bath or bubble bath. Your doctor will also likely prescribe oral pain medications, infection-fighting medications, and possibly an IV of medication to help restore blood flow to the affected area.
Get treatment for your specific symptoms. The treatment your doctor will give you will depend on the severity of the ice burn, the symptoms you have, and whether you also have frostbite. In most cases, your doctor will start by rewarming the skin using a 20-minute warm water bath or bubble bath. Your doctor will also likely prescribe oral pain medications, infection-fighting medications, and possibly an IV of medication to help restore blood flow to the affected area. - If both the skin and tissue are damaged, your doctor may also perform a procedure to remove all or part of the burned area.
- In severe cases, the doctor may also perform an X-ray, bone scan, or MRI to determine the extent of the damage.
- It can take anywhere from a few weeks to a few months for a severe ice burn to fully heal. If you also had deeper frostbite symptoms, the affected area may never fully recover.
Tips
- To relieve the pain, you can take an over-the-counter pain reliever such as ibuprofen.
- Ibuprofen and acetaminophen can also help reduce swelling from frostbite.
- You can try to prevent ice burns by wearing clothing that covers your skin and is thick enough for the wind and weather.
- If you have a cold-induced injury that is not frozen, you should also seek emergency care.
Warnings
- Ice compresses are one of the most common causes of ice burns. To avoid burns when using an ice pack, place a towel between your skin and the ice pack.
- While anyone can get an ice burn under certain circumstances, people who participate in winter sports, smoke, take beta-blockers, or have a neuropathic condition that reduces their ability to perceive pain or cold are more likely to get an ice burn.
- Young children and older adults are also more likely to get ice burn because their bodies are usually less able to regulate body temperature.
- Very rarely, tetanus can be a complication of frostbite.