Author:
Alice Brown
Date Of Creation:
28 May 2021
Update Date:
1 July 2024

Content
- Steps
- Method 1 of 3: Determine the cause
- Method 2 of 3: Treating Onycholysis
- Method 3 of 3: Preventing Onycholysis
Onycholysis is a gradual and painless separation of the nail from the nail bed. This is usually due to trauma, but there may be other reasons as well. See your doctor to determine the cause of onycholysis. If there is a medical problem, your doctor will prescribe treatment so that your nails can heal. If onycholysis is caused by injury or prolonged exposure to moisture or chemicals, the problem may go away with proper treatment and preventive measures.
Steps
Method 1 of 3: Determine the cause
 1 See your doctor if you have symptoms of onycholysis. The doctor will examine your nails and determine the cause of the condition. He may also take a tissue sample from under one of your nails to check for fungus or other infections. See your doctor if:
1 See your doctor if you have symptoms of onycholysis. The doctor will examine your nails and determine the cause of the condition. He may also take a tissue sample from under one of your nails to check for fungus or other infections. See your doctor if: - one or more nails have risen from the nail bed;
- the border between the nail bed and the white part of the nail has a curved shape;
- most of the nail (or several) has become dull or discolored;
- one or more nail plates are deformed and the edges are bent.
 2 Tell your doctor about any medications you are taking. Some medications can cause nails to react to sunlight and separate from the nail bed as a result. Most often, this reaction is caused by drugs from the group of psoralens, tetracyclines and fluoroquinolones. Tell your doctor about the prescription and over-the-counter drugs you are taking so that they can be ruled out as a likely cause of the illness.
2 Tell your doctor about any medications you are taking. Some medications can cause nails to react to sunlight and separate from the nail bed as a result. Most often, this reaction is caused by drugs from the group of psoralens, tetracyclines and fluoroquinolones. Tell your doctor about the prescription and over-the-counter drugs you are taking so that they can be ruled out as a likely cause of the illness.  3 Tell your doctor if you have had psoriasis or any other skin condition in the past. Tell your doctor if you have already been diagnosed with psoriasis as it can cause onycholysis. If you have not been diagnosed with this, tell your doctor about any skin conditions you have recently. Symptoms of psoriasis include:
3 Tell your doctor if you have had psoriasis or any other skin condition in the past. Tell your doctor if you have already been diagnosed with psoriasis as it can cause onycholysis. If you have not been diagnosed with this, tell your doctor about any skin conditions you have recently. Symptoms of psoriasis include: - dry, chapped, or bleeding skin;
- red spots on the skin;
- silvery scales on the skin;
- itching, burning, or pain.
 4 Talk about recent injuries to your hands and feet. Trauma to the nail bed can lead to gradual and painless onycholysis. Tell your doctor about any recent injuries that may have affected your nails. This could be a blow or puncture injury in which the nail could break off or come off.
4 Talk about recent injuries to your hands and feet. Trauma to the nail bed can lead to gradual and painless onycholysis. Tell your doctor about any recent injuries that may have affected your nails. This could be a blow or puncture injury in which the nail could break off or come off. - Injuries can be minor (like hitting your finger on an object) or more serious (pinching your finger in a car door).
 5 Consider environmental factors. Exposure to stress factors can lead to nail damage and, over time, to onycholysis. Think about your hygiene habits, nail care, and physical activity to determine what activities could lead to onycholysis. Factors related to your actions or environment include:
5 Consider environmental factors. Exposure to stress factors can lead to nail damage and, over time, to onycholysis. Think about your hygiene habits, nail care, and physical activity to determine what activities could lead to onycholysis. Factors related to your actions or environment include: - prolonged exposure to water (for example, swimming or washing dishes);
- Frequent use of nail polish, false nails, or nail polish remover
- Frequent exposure to chemicals such as cleaning products
- walking in closed toe shoes with uneven pressure distribution due to flat feet.
Method 2 of 3: Treating Onycholysis
 1 Trim your nails to prevent further damage. Nails that come off the nail bed are very easily injured. Ask your doctor if they can remove the raised portion of the nail. Removing the nail yourself can cause severe pain and lead to infection and further damage.
1 Trim your nails to prevent further damage. Nails that come off the nail bed are very easily injured. Ask your doctor if they can remove the raised portion of the nail. Removing the nail yourself can cause severe pain and lead to infection and further damage. - If you have an infection under your toenail, removing it will allow you to apply the medicine directly to the infected area.
 2 Use antifungal agents if onycholysis is caused by a fungal infection. Before the nail can grow back, you need to get rid of the fungus and bacteria that are underneath. After your doctor diagnoses a fungal infection, he or she will prescribe oral and topical antifungal agents to treat it. Take or apply these products exactly as directed until a new, healthy nail begins to grow.
2 Use antifungal agents if onycholysis is caused by a fungal infection. Before the nail can grow back, you need to get rid of the fungus and bacteria that are underneath. After your doctor diagnoses a fungal infection, he or she will prescribe oral and topical antifungal agents to treat it. Take or apply these products exactly as directed until a new, healthy nail begins to grow. - Depending on the severity and nature of the infection, oral medications will need to be taken for 6 to 24 weeks.
- Topical creams and ointments should be applied every day around the nail bed. It usually takes a long time for them to take effect.
- Oral medications are generally more effective than topical medications, but they come with additional risks, such as potential liver problems.
- Consult your doctor again after 6-12 weeks of treatment.
 3 Ask your doctor about treatment options for onycholysis caused by psoriasis. Onycholysis is often the result of a disease such as psoriasis, which can be treated in several ways. Discuss these with your doctor to determine which one will give the best result. Psoriasis is treated in the following ways:
3 Ask your doctor about treatment options for onycholysis caused by psoriasis. Onycholysis is often the result of a disease such as psoriasis, which can be treated in several ways. Discuss these with your doctor to determine which one will give the best result. Psoriasis is treated in the following ways: - oral medications such as methotrexate, cyclosporine, and retinoids
- topical agents such as corticosteroids, synthetic vitamin D, anthralin, calcineurin inhibitors, salicylic acid, and topical retinoids;
- phototherapy, such as UVB phototherapy, narrowband UVB phototherapy, and excimer laser therapy;
- alternative natural therapies, such as aloe vera, fish oil, and topical application of holly mahonia.
 4 Ask your doctor about vitamin supplements if your body is deficient in vitamins and minerals. Lack of vitamins and minerals will make your nails weak and brittle, making it harder for them to grow back after onycholysis. Ask your doctor if you should start taking vitamin supplements to strengthen your nails. Iron is especially helpful in this.
4 Ask your doctor about vitamin supplements if your body is deficient in vitamins and minerals. Lack of vitamins and minerals will make your nails weak and brittle, making it harder for them to grow back after onycholysis. Ask your doctor if you should start taking vitamin supplements to strengthen your nails. Iron is especially helpful in this. - Biotin, one of the B vitamins, can also improve nail health.
- Taking a multivitamin daily will ensure that you get all the vitamins your body needs.
- Your doctor may also recommend making some changes to your diet to increase your intake of certain vitamins and minerals.
 5 Treat your nails with a prescription desiccant after they get wet. To protect your nails from excess moisture while they are healing, apply a desiccant to them if your hands and feet get wet. Ask your doctor if they can prescribe a desiccant (such as 3% thymol in alcohol). This liquid desiccant must be applied directly to your nails with a dropper or small brush.
5 Treat your nails with a prescription desiccant after they get wet. To protect your nails from excess moisture while they are healing, apply a desiccant to them if your hands and feet get wet. Ask your doctor if they can prescribe a desiccant (such as 3% thymol in alcohol). This liquid desiccant must be applied directly to your nails with a dropper or small brush. - This desiccant should be used for 2-3 months as the nails heal.
Method 3 of 3: Preventing Onycholysis
 1 Keep your nails dry and clean. Wash your nails frequently throughout the day to prevent the growth of bacteria or fungi underneath. Lather your nails with mild hand soap and rinse thoroughly. After that, do not forget to wipe them dry.
1 Keep your nails dry and clean. Wash your nails frequently throughout the day to prevent the growth of bacteria or fungi underneath. Lather your nails with mild hand soap and rinse thoroughly. After that, do not forget to wipe them dry. 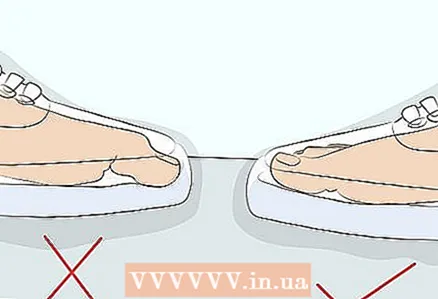 2 Wear the correct size shoes. Shoes that are too small will put pressure on your toes, increasing the likelihood of injury. Permanent injury to the nails can lead to the development of onycholysis.
2 Wear the correct size shoes. Shoes that are too small will put pressure on your toes, increasing the likelihood of injury. Permanent injury to the nails can lead to the development of onycholysis.  3 Do not wear wet or wet shoes for a long time. Dampness can lead to fungal growth and therefore onycholysis. Wear waterproof shoes when going for a walk or exercising in wet weather. Remove sweaty socks and shoes immediately after finishing your workout to prevent bacteria growth.
3 Do not wear wet or wet shoes for a long time. Dampness can lead to fungal growth and therefore onycholysis. Wear waterproof shoes when going for a walk or exercising in wet weather. Remove sweaty socks and shoes immediately after finishing your workout to prevent bacteria growth. - If your shoes get wet, let them air dry.
- If you exercise a lot, consider purchasing multiple pairs of sneakers to avoid wearing wet or wet shoes.
 4 Wear gloves when cleaning or doing laundry. Prolonged exposure to chemicals and frequent immersion of hands in water can lead to onycholysis. Protect your hands with rubber gloves while cleaning the house, washing dishes, or similar activities. Gloves will also protect long nails from injury when doing housework.
4 Wear gloves when cleaning or doing laundry. Prolonged exposure to chemicals and frequent immersion of hands in water can lead to onycholysis. Protect your hands with rubber gloves while cleaning the house, washing dishes, or similar activities. Gloves will also protect long nails from injury when doing housework.  5 Keep your nails short and clean. It is easier for moisture and bacteria to collect under long nails, which increases the risk of onycholysis. To prevent this, trim your nails regularly to keep them short and tidy. Trim your nails with clean nail clippers and smooth the edges with a file.
5 Keep your nails short and clean. It is easier for moisture and bacteria to collect under long nails, which increases the risk of onycholysis. To prevent this, trim your nails regularly to keep them short and tidy. Trim your nails with clean nail clippers and smooth the edges with a file. - Short nails are also less prone to damage and injury.