Author:
Bobbie Johnson
Date Of Creation:
2 April 2021
Update Date:
1 July 2024
Content
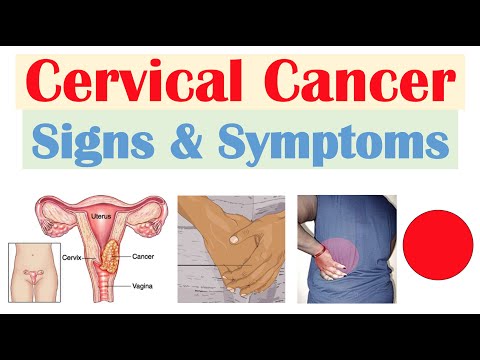
Cervical cancer, or cancer of the cervix (the lower part of the uterus), occurs in women of various ages, but the largest number occurs between the ages of 20 and 50. The vast majority of women who have cancer are not monitored regularly by a gynecologist and do not undergo PAP screening. Fortunately, with early detection and treatment, cervical cancer is curable. The main symptoms are abnormal uterine bleeding and pain. Symptoms appear already at the stage when abnormal cells invade the surrounding tissues. Therefore, if such symptoms appear, you should consult a doctor as soon as possible. Regular screening for PAP and HPV helps detect a precancerous condition - that is, detect cancer before it becomes cervical cancer.
Steps
Method 1 of 2: Symptoms
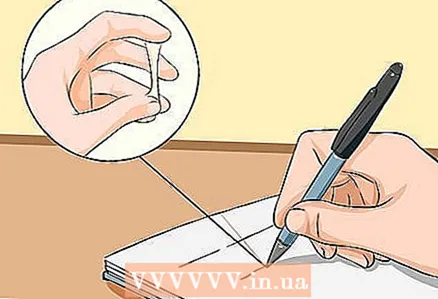
 1 Monitor your menstrual cycle. In premenopausal and perimenopausal women, note the onset and duration of your period. At menopause, mark the date of your last menstrual period. The main symptom of cervical cancer is abnormal vaginal bleeding. You need to know what is normal for you.
1 Monitor your menstrual cycle. In premenopausal and perimenopausal women, note the onset and duration of your period. At menopause, mark the date of your last menstrual period. The main symptom of cervical cancer is abnormal vaginal bleeding. You need to know what is normal for you. - In premenopausal women, the menstrual cycle is regular. For each woman, it is different in duration, but varies within 28 ± 7 days.
- During perimenopause, the menstrual cycle becomes irregular. This period begins at the age of 40-50 years and is associated with ovarian depletion, which reduces the secretion of estrogen. This period can last from several months to 10 years, after which menopause occurs.
- Menstruation is absent during menopause. The hormone levels are such that ovulation does not occur, so pregnancy is not possible.
- Menstruation is absent after a hysterectomy (removal of the uterus). Since the uterus is removed, there is no endometrial rejection, so there is no bleeding. If you have ovaries that work as before, this is not a menopause.
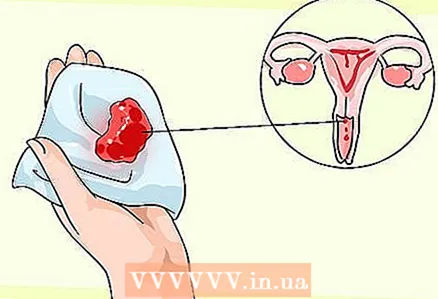 2 Pay attention to spotting between periods. When you have spotting, there is much less blood and a slightly different color than your regular menstrual flow.
2 Pay attention to spotting between periods. When you have spotting, there is much less blood and a slightly different color than your regular menstrual flow. - In premenopausal women, the cycle can sometimes be irregular. Spotting discharge is also possible. A large number of factors contribute to this, in particular illness, stress or physical activity. See your doctor if your menstrual cycle remains irregular for several months.
- Spotting can also be a normal phase of your perimenopause. However, at this age, it is necessary to be especially vigilant and attentive to other symptoms of cervical cancer.
 3 Pay attention to longer, heavier periods. During each menstrual cycle, the amount, color, consistency of the discharge may change. See your doctor if these changes are significant.
3 Pay attention to longer, heavier periods. During each menstrual cycle, the amount, color, consistency of the discharge may change. See your doctor if these changes are significant.  4 See your doctor if your period starts again unexpectedly. Remember that during menopause or after a hysterectomy, any vaginal bleeding is abnormal.
4 See your doctor if your period starts again unexpectedly. Remember that during menopause or after a hysterectomy, any vaginal bleeding is abnormal. - In a hysterectomy, the cervix is not removed. Removal of the uterus and cervix is performed with a total hysterectomy. Supracervical hysterectomy is performed for non-malignant surgeries, so the risk of cervical cancer remains. Ask your gynecologist what type of surgery you had.
- The absence of menstruation for 12 months implies the onset of menopause.
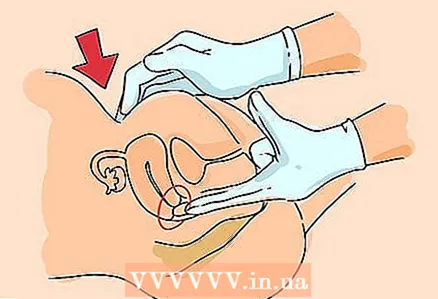 5 Note the change in vaginal bleeding after normal activities. These include vaginal intercourse, douching, and examination by a gynecologist. Be sure to inform the gynecologist about the nature of the bleeding.
5 Note the change in vaginal bleeding after normal activities. These include vaginal intercourse, douching, and examination by a gynecologist. Be sure to inform the gynecologist about the nature of the bleeding. - During a gynecological examination, the doctor inserts two fingers into the vagina, and with the other hand presses on the lower abdomen. So the doctor examines the uterus, cervix and ovaries for pathology. This examination should not cause a significant increase in bleeding.
 6 Watch for any unusual vaginal discharge. Discharge between periods can be bloody and have a foul odor.
6 Watch for any unusual vaginal discharge. Discharge between periods can be bloody and have a foul odor. - The cervix secretes mucus of varying consistency depending on the day of the menstrual cycle, which promotes or prevents pregnancy. This discharge should not be bloody unless it is during your period.
- If menstrual blood accumulates in the vagina for 6 to 8 hours, an unpleasant odor develops. The smell of this discharge is different from the foul smell of discharge between periods.
- Get medical attention. A foul-smelling discharge may be due to infection and be accompanied by pain and bleeding, precancerous lesions, or cancer.
 7 If you experience lower abdominal pain or after sex, see your doctor. In some cases, pain after sex is possible: 3 out of 4 women have experienced pain after sex at some point in their lives. However, if these pains are severe or occur frequently, tell your doctor. Learn to distinguish between pain during menstruation and pain in the pelvis and lower abdomen.
7 If you experience lower abdominal pain or after sex, see your doctor. In some cases, pain after sex is possible: 3 out of 4 women have experienced pain after sex at some point in their lives. However, if these pains are severe or occur frequently, tell your doctor. Learn to distinguish between pain during menstruation and pain in the pelvis and lower abdomen. - During menopause and perimenopause, the vagina undergoes changes due to changes in estrogen levels. The vaginal wall may become thinner, drier, less elastic, and more prone to irritation (atrophic vaginitis). During such periods, sex can become painful due to the above changes.
- Pain during sex can also occur when the skin is irritated or when there is not enough lubricant from the vagina.
Method 2 of 2: Get medical attention
 1 Seek medical attention right away if symptoms occur. Delaying a visit to the doctor will lead to the progression of the disease and reduce the chances of effective treatment.
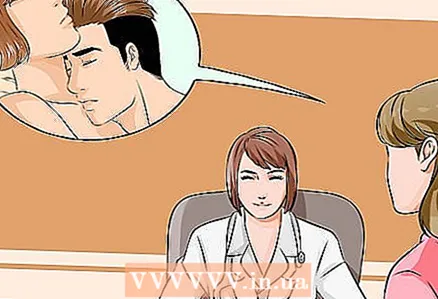
1 Seek medical attention right away if symptoms occur. Delaying a visit to the doctor will lead to the progression of the disease and reduce the chances of effective treatment. - During the appointment, the doctor should listen to the complaints and take your and family history.The doctor should also identify individual risk factors, which include a large number of sexual partners, early onset of sexual activity, sexually transmitted diseases in partners, decreased immunity, smoking.
- After taking the history, the doctor should conduct an examination to determine the overall health. During the appointment, he may take a smear for PAP and HPV - these are screening tests (to detect signs of cervical cancer), but not diagnostic (not confirming the presence of cancer).
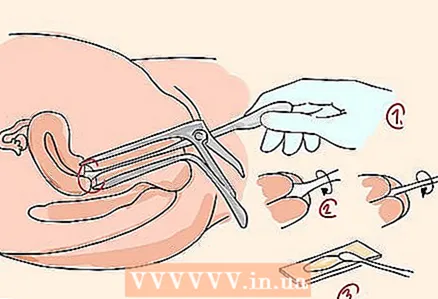
- Diagnostic tests are performed only after a positive PAP test and / or in the presence of symptoms of cervical cancer. These studies include colposcopy. Colposcopy is a procedure in which a speculum is inserted into the vagina to view the cervix under magnification. If necessary, a scraping of the endocervix (the inner lining of the cervical canal) is taken and / or a cone biopsy is done. The materials obtained as a result of these examinations are studied by a pathologist in order to detect precancerous and cancerous changes in the cells.
 2 Get regular screening for cervical cancer. There are two tests that doctors prescribe to detect precancerous lesions: a PAP smear and an HPV test.
2 Get regular screening for cervical cancer. There are two tests that doctors prescribe to detect precancerous lesions: a PAP smear and an HPV test.  3 Get a PAP smear regularly. The PAP smear, or PAP test, is used to detect precancerous cells that, if left untreated, can become cervical cancer. A PAP smear should be taken for all women between the ages of 21 and 65. The swab is taken by a gynecologist in the treatment room.
3 Get a PAP smear regularly. The PAP smear, or PAP test, is used to detect precancerous cells that, if left untreated, can become cervical cancer. A PAP smear should be taken for all women between the ages of 21 and 65. The swab is taken by a gynecologist in the treatment room. - During the analysis, the doctor inserts a speculum into the vagina to examine the walls of the vagina and the cervix, and then collects some cells, mucus from the cervix and surrounding tissues. A tissue sample is applied to a glass slide or placed in a flask with liquid, after which it is sent to a laboratory, where a laboratory assistant examines the tissue through a microscope to detect pathologies.
- It is necessary to have a regular PAP smear, even during periods of abstinence from sex and after menopause.
- A PAP smear can be taken at any hospital or clinic, as it is included in the list of compulsory health insurance services.
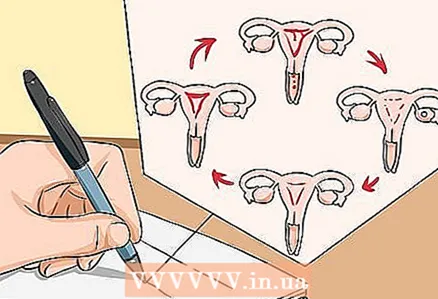
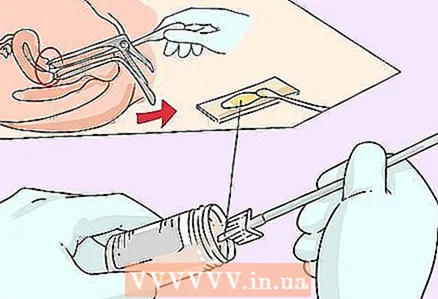 4 Get your HPV test. The HPV test is used to detect the human papillomavirus, which causes precancerous changes in the cells of the cervix. Most cases of cervical cancer are associated with HPV infection. Human papillomavirus is transmitted from person to person during sex. Cells collected on a PAP smear can be tested for HPV infection.
4 Get your HPV test. The HPV test is used to detect the human papillomavirus, which causes precancerous changes in the cells of the cervix. Most cases of cervical cancer are associated with HPV infection. Human papillomavirus is transmitted from person to person during sex. Cells collected on a PAP smear can be tested for HPV infection. - The cervix is in the shape of a cylinder and is the lower part of the uterus. Exocervix is the part of the cervix that the doctor sees during examination in the mirrors. The endocervix is the inner lining of the cervix that runs into the endometrium. Cervical cancer most often occurs in the zone of transition of the exocervix to the endocervix. Cervical cell samples are usually taken from this area.
- For women over 30, a Pap smear and HPV test should be done every 6 years.
 5 Talk to your doctor about how often you need to have a Pap smear and HPV test. The frequency with which these screening tests are required depends on several factors, such as age, number of sexual partners, history, and previous PAP smear and HPV test results.
5 Talk to your doctor about how often you need to have a Pap smear and HPV test. The frequency with which these screening tests are required depends on several factors, such as age, number of sexual partners, history, and previous PAP smear and HPV test results. - Women aged 21-29 should have a PAP smear every 3 years. Women aged 30-63 should have a PAP smear every 3 years or a PAP smear and HPV test every 5 years.
- If you have a weakened immune system, such as due to HIV infection, and have positive PAP smear results, talk to your doctor about more frequent testing.
- Cervical cancer is one of the most common cancers in women around the world. However, the incidence of this cancer is much lower in many developed countries due to the widespread and regular use of PAP smears and HPV tests.
- Early diagnosis and treatment is the key to health. Precancerous cervical cells with pronounced changes are a significant risk of developing cancer. Transformation of normal to abnormal invasive cancer cells usually occurs within 10 years, but sometimes it can happen earlier.