Author:
Alice Brown
Date Of Creation:
26 May 2021
Update Date:
24 June 2024

Content
- Steps
- Method 1 of 4: Identifying High Risk Situations
- Method 2 of 4: Recognizing bleeding associated with PPH
- Method 3 of 4: Recognizing Additional Symptoms
- Method 4 of 4: Create a nursing plan (for nurses and doctors)
- Tips
- Warnings
Postpartum hemorrhage is an abnormal amount of blood released from the vagina after childbirth.Bleeding can occur 24 hours after delivery or after several days. It is one of the leading causes of maternal mortality after childbirth, accounting for 8%. The percentage of deaths from postpartum haemorrhage is significantly higher in underdeveloped and developing countries. However, it is normal for bleeding (known as lochia) after you have given birth. This type of bleeding can last for several weeks. It is very important to know how to distinguish postpartum haemorrhage from lochia in the early stages in order to avoid complications.
Steps
Method 1 of 4: Identifying High Risk Situations
 1 Learn what factors can cause postpartum hemorrhage. Several causes that occur before, during, and after childbirth can lead to postpartum hemorrhage. Some of these conditions require a woman's close observation during and after childbirth to rule out PPH. It is important to be aware of these conditions as they increase a woman's risk of PPH.
1 Learn what factors can cause postpartum hemorrhage. Several causes that occur before, during, and after childbirth can lead to postpartum hemorrhage. Some of these conditions require a woman's close observation during and after childbirth to rule out PPH. It is important to be aware of these conditions as they increase a woman's risk of PPH. - Placenta previa, placental abruption, retained placenta and other placental abnormalities
- Multiple pregnancies
- Preeclampsia or increased blood pressure during pregnancy
- History of PPH during previous labor
- Obesity
- Uterine abnormalities
- Anemia
- Emergency caesarean section
- Bleeding during pregnancy
- Long-term labor more than 12 hours
- Birth of a child weighing over 4 kg
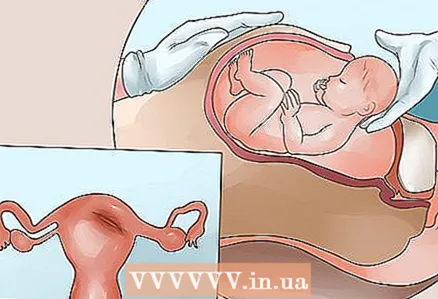
 2 Understand that uterine atony is the cause of a lot of blood loss. Postpartum hemorrhage or excessive blood loss after childbirth is one of the leading causes of maternal death, even after a successful birth. There are several reasons why excessive bleeding occurs, more than 500 ml after delivery. One of them is called uterine atony.
2 Understand that uterine atony is the cause of a lot of blood loss. Postpartum hemorrhage or excessive blood loss after childbirth is one of the leading causes of maternal death, even after a successful birth. There are several reasons why excessive bleeding occurs, more than 500 ml after delivery. One of them is called uterine atony. - Uterine atony is when the mother's uterus (the part of the female reproductive system that the baby was in) has difficulty returning to its original position.
- The uterus becomes hollow and uncontracted, while it should be toned and contract. It helps the blood move quickly and easily, which contributes to the occurrence of postpartum hemorrhage.
 3 Be aware that trauma during childbirth can lead to postpartum hemorrhage. This is another reason why excessive bleeding occurs when trauma occurs when the baby leaves the birth canal.
3 Be aware that trauma during childbirth can lead to postpartum hemorrhage. This is another reason why excessive bleeding occurs when trauma occurs when the baby leaves the birth canal. - Injuries can be in the form of cuts that can be caused by the use of assistive devices during childbirth.
- In addition, damage can occur when the child is larger than average and exits quickly. This can cause tears in the vaginal opening.
 4 Understand that sometimes blood does not flow directly from a woman's body. Bleeding caused by PPH does not always come from the body. Sometimes bleeding occurs inside, and if there is no outlet for blood, it will move towards the genitals and form what is called a hematoma.
4 Understand that sometimes blood does not flow directly from a woman's body. Bleeding caused by PPH does not always come from the body. Sometimes bleeding occurs inside, and if there is no outlet for blood, it will move towards the genitals and form what is called a hematoma.
Method 2 of 4: Recognizing bleeding associated with PPH
 1 Track your blood count. The type of bleeding that occurs immediately after delivery, within 24 hours after delivery, or a few days after delivery is an important factor to rule out the possibility of PPH. The most important parameter for this is the amount of blood.
1 Track your blood count. The type of bleeding that occurs immediately after delivery, within 24 hours after delivery, or a few days after delivery is an important factor to rule out the possibility of PPH. The most important parameter for this is the amount of blood. - Any bleeding more than 500 ml after vaginal delivery and more than 1000 ml after cesarean section can already be considered postpartum bleeding.
- In addition, bleeding that exceeds 1000 ml is called severe bleeding and requires immediate medical attention, especially if additional risk factors are present.
 2 Look at the flow and texture of the blood. PPH usually creates a continuous, profuse flow of blood, with or without several large clots.However, blood clots most clearly characterize PPH, which develops several days after delivery, and this type of bleeding may also flow more smoothly.
2 Look at the flow and texture of the blood. PPH usually creates a continuous, profuse flow of blood, with or without several large clots.However, blood clots most clearly characterize PPH, which develops several days after delivery, and this type of bleeding may also flow more smoothly.  3 Also be aware that the smell of blood can help determine if it is PPH or not. Some additional characteristics that can help differentiate PPH from normal postpartum hemorrhage or lochia (vaginal discharge consisting of blood, tissue from the lining of the uterus, and bacteria) are odors. Suspect PPH if the lochiae has a foul odor or if blood flow suddenly increases after childbirth.
3 Also be aware that the smell of blood can help determine if it is PPH or not. Some additional characteristics that can help differentiate PPH from normal postpartum hemorrhage or lochia (vaginal discharge consisting of blood, tissue from the lining of the uterus, and bacteria) are odors. Suspect PPH if the lochiae has a foul odor or if blood flow suddenly increases after childbirth.
Method 3 of 4: Recognizing Additional Symptoms
 1 Seek medical attention if you identify any serious symptoms. Acute PPH is often accompanied by signs of shock, such as low blood pressure, tachycardia or low heart rate, fever, chills, weakness, or collapse. These are the most characteristic signs of PPH and the most dangerous. They require immediate medical attention.
1 Seek medical attention if you identify any serious symptoms. Acute PPH is often accompanied by signs of shock, such as low blood pressure, tachycardia or low heart rate, fever, chills, weakness, or collapse. These are the most characteristic signs of PPH and the most dangerous. They require immediate medical attention.  2 Watch for "cues" that appear a few days after giving birth. Some of them do not require urgent medical attention, but they represent hidden danger signs of secondary PPH, which usually appear several days after delivery. These include fever, abdominal pain, painful urination, general weakness, tenderness to palpation of the abdomen over the suprapubic region, and adnexia.
2 Watch for "cues" that appear a few days after giving birth. Some of them do not require urgent medical attention, but they represent hidden danger signs of secondary PPH, which usually appear several days after delivery. These include fever, abdominal pain, painful urination, general weakness, tenderness to palpation of the abdomen over the suprapubic region, and adnexia. 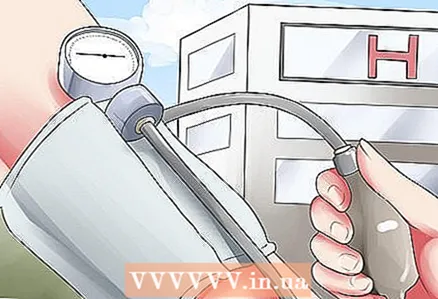 3 Be sure to go to the hospital if you notice these warning signs. PPH requires urgent medical attention and immediate hospitalization and measures to stop the bleeding. Therefore, this is not a condition that can be ignored. If you experience any of the following symptoms after childbirth, see your doctor right away, as shock may develop.
3 Be sure to go to the hospital if you notice these warning signs. PPH requires urgent medical attention and immediate hospitalization and measures to stop the bleeding. Therefore, this is not a condition that can be ignored. If you experience any of the following symptoms after childbirth, see your doctor right away, as shock may develop. - Low blood pressure
- Low heart rate
- Oliguria or decreased urine output
- Sudden and persistent vaginal bleeding or large clots
- Fainting
- Chills
- Fever
- Stomach ache
Method 4 of 4: Create a nursing plan (for nurses and doctors)
 1 Learn what a nursing plan is. The most important thing for reducing the risk of mortality after childbirth is the ability to detect early signs of bleeding in time and determine its cause. A quick determination of the cause of the bleeding allows a quick and correct response.
1 Learn what a nursing plan is. The most important thing for reducing the risk of mortality after childbirth is the ability to detect early signs of bleeding in time and determine its cause. A quick determination of the cause of the bleeding allows a quick and correct response. - A nursing plan is a very useful tool. There are five stages to this plan. These steps include patient assessment, diagnosis, planning, surgical or medical options, and final assessment.
- It is important to know what to look for and what to do at each of these stages in order to plan for the care of patients with postpartum haemorrhage.
 2 Pay special attention to mothers who are predisposed to developing postpartum haemorrhage. It is important to take note of the mother's medical history before making an assessment. There are several predisposing factors that increase a woman's tendency to have postpartum haemorrhage, since all women who have recently given birth are prone to excessive blood loss. If one or more of the following factors are present in the mother, the assessment should be done at least every 15 minutes during and after childbirth until the mother shows no signs of bleeding.
2 Pay special attention to mothers who are predisposed to developing postpartum haemorrhage. It is important to take note of the mother's medical history before making an assessment. There are several predisposing factors that increase a woman's tendency to have postpartum haemorrhage, since all women who have recently given birth are prone to excessive blood loss. If one or more of the following factors are present in the mother, the assessment should be done at least every 15 minutes during and after childbirth until the mother shows no signs of bleeding. - Such predisposing factors include: distension of the uterus, which was caused by the bearing of a large child or the presence of excess fluid in the placenta (the sac surrounding the baby), the birth of more than five children, prolonged labor, prolonged childbirth, the use of assistive devices, cesarean, manual removal of the placenta and eversion uterus.
- Predisposing factors for heavy bleeding also include mothers who have suffered from problems such as placenta previa, placenta accrete, who have taken medications such as oxytocin, prostaglandins, tocolytics or magnesium sulfate, and who have undergone general anesthesia if the mother has poor blood clotting; suffered from bleeding during previous childbirth, had uterine fibroids or had a bacterial infection of the membranes (chorioamnionitis).
 3 Evaluate the mother frequently. There are certain physical aspects in assessing the mother's condition that need to be checked regularly to determine if there is ongoing postpartum haemorrhage and to help determine the cause. These physical aspects include:
3 Evaluate the mother frequently. There are certain physical aspects in assessing the mother's condition that need to be checked regularly to determine if there is ongoing postpartum haemorrhage and to help determine the cause. These physical aspects include: - The bottom of the uterus (the upper part of the uterus, opposite the cervix), the bladder, the amount of lochia (fluid that leaves the vagina, which is made up of blood, mucus, and uterine tissue), four vital signs (temperature, pulse, respiratory rate and blood pressure) as well as skin color.
- When evaluating these areas, it is important to note what needs to be looked at. Follow the instructions below for more information.
 4 Check your fundus. It is important to check it in order to determine its location. Usually, when palpated, it should be elastic and turned towards the umbilical cord (navel). If there is any deviation from this - for example, if the bottom is soft to the touch or difficult to determine - this could be a sign of postpartum hemorrhage.
4 Check your fundus. It is important to check it in order to determine its location. Usually, when palpated, it should be elastic and turned towards the umbilical cord (navel). If there is any deviation from this - for example, if the bottom is soft to the touch or difficult to determine - this could be a sign of postpartum hemorrhage.  5 Examine the bladder. There may be times when the bladder is the cause of bleeding, and this is expressed by the fact that the fundus of the uterus will be displaced above the umbilical zone (navel).
5 Examine the bladder. There may be times when the bladder is the cause of bleeding, and this is expressed by the fact that the fundus of the uterus will be displaced above the umbilical zone (navel). - Let the woman urinate, and if after that the bleeding goes away, then the cause is in the bladder, causing the uterus to displace.
 6 Rate the lochia. When assessing the amount of blood flowing out of the vagina, it is important to weigh the pads used before and after to get an accurate conclusion. Excessive bleeding is detected if the pad is filled in 15 minutes.
6 Rate the lochia. When assessing the amount of blood flowing out of the vagina, it is important to weigh the pads used before and after to get an accurate conclusion. Excessive bleeding is detected if the pad is filled in 15 minutes. - Sometimes the amount of blood is often overlooked, but you can check the amount by asking the mother to turn on her side; so you can check the area underneath, especially the buttocks.
 7 Check the main indicators of the state of the body. These include blood pressure, respiratory rate (number of breaths in and out), heart rate, and temperature. During postpartum hemorrhage, her heart rate should be below normal (60 to 100 per minute), but it may change depending on her previous heart rate.
7 Check the main indicators of the state of the body. These include blood pressure, respiratory rate (number of breaths in and out), heart rate, and temperature. During postpartum hemorrhage, her heart rate should be below normal (60 to 100 per minute), but it may change depending on her previous heart rate. - However, these vital signs may not show abnormalities until the mother is suffering from excessive blood loss. Therefore, you should evaluate any deviation from the normal state of the body, paying attention to warm, dry skin, pink lips and mucous membranes.
- You can also check your nails by pressing and releasing them. At the second interval, the nail plate should return to pink again.
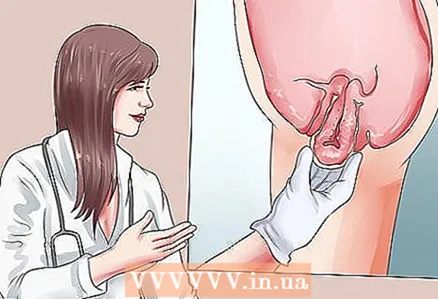
 8 Understand that trauma can lead to excessive bleeding. If any of these changes are assessed, the mother may be suffering from postpartum hemorrhage caused by the inability of the uterus to contract and return to its original shape. However, if the uterus has been checked and found to be contracting normally and not dislocated, but heavy bleeding is still ongoing, it could be due to injury. In assessing trauma, the nature of the pain and the external color of the vagina must be taken into account.
8 Understand that trauma can lead to excessive bleeding. If any of these changes are assessed, the mother may be suffering from postpartum hemorrhage caused by the inability of the uterus to contract and return to its original shape. However, if the uterus has been checked and found to be contracting normally and not dislocated, but heavy bleeding is still ongoing, it could be due to injury. In assessing trauma, the nature of the pain and the external color of the vagina must be taken into account. - Pain: The mother will experience deep, severe pain in the pelvic or rectal area. This could be a sign of internal bleeding.
- External vaginal opening: It can be swollen and discolored (typically purple to bluish black). It can also be a sign of internal bleeding.
- If the laceration or wound is on the outside, it can be easily assessed by visual inspection, especially if done under proper lighting.
 9 Notify other healthcare providers. If there is significant blood loss and the cause has been identified, the next step in your health care plan is diagnosis.
9 Notify other healthcare providers. If there is significant blood loss and the cause has been identified, the next step in your health care plan is diagnosis. - When confirming a diagnosis of postpartum haemorrhage, the first planned step is always to inform the physician and other health care providers involved in caring for the mother.
- The main role of the nurse is to monitor the woman, apply a variety of methods to minimize blood loss and respond appropriately if there is any significant change from the previous condition. It is desirable, of course, that there be no deterioration.
 10 Massage the woman's uterus and monitor for blood loss. The nurse is responsible for monitoring vital signs and weighing the pads and bedding. Massaging the uterus will also help it contract, and it will be toned again. Warn doctors or midwives when there is still bleeding (even during massage) - this is also very important.
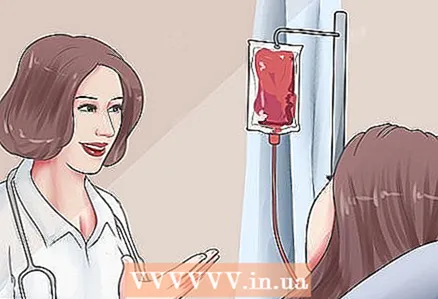
10 Massage the woman's uterus and monitor for blood loss. The nurse is responsible for monitoring vital signs and weighing the pads and bedding. Massaging the uterus will also help it contract, and it will be toned again. Warn doctors or midwives when there is still bleeding (even during massage) - this is also very important.  11 Adjust the mother's blood level. The nurse should have a supply of blood if there is a need for blood transfusion. The regulation of the intravenous flow is also the responsibility of the nurse.
11 Adjust the mother's blood level. The nurse should have a supply of blood if there is a need for blood transfusion. The regulation of the intravenous flow is also the responsibility of the nurse.  12 Put the woman in the Trendelenburg position. The mother should be positioned in the so-called modified Trendelenburg position, where the legs are raised at least 10 degrees and a maximum of 30 degrees. The body is in a horizontal position, the head is also slightly raised.
12 Put the woman in the Trendelenburg position. The mother should be positioned in the so-called modified Trendelenburg position, where the legs are raised at least 10 degrees and a maximum of 30 degrees. The body is in a horizontal position, the head is also slightly raised.  13 Give the woman medicine. The mother will take a range of medications as usual, such as oxytocin and methylergometrine, and the nurse should determine the side effects of these medications, as they can also be life-threatening for the mother.
13 Give the woman medicine. The mother will take a range of medications as usual, such as oxytocin and methylergometrine, and the nurse should determine the side effects of these medications, as they can also be life-threatening for the mother. - Oxytocin is used primarily for the induction of labor and is safe to use during labor, but it is also used postpartum. The drug causes contraction of the smooth muscles of the uterus. It is usually injected intramuscularly (usually in the upper arm) by injection at a dose of 0.2 mg every 2–4 hours, with a maximum of 5 doses postpartum. Oxytocin has an antidiuretic effect, which means the drug will interfere with urination.
- Methyl ergometrine is a drug that is never given before childbirth, but may be given later. This is because the action of Methylergometrine is to accelerate the sustained contraction of the uterus, and, therefore, causes a decrease in the baby's oxygen consumption while still inside the uterus. Methylergometrine is also injected intramuscularly at a dose of 0.2 mg every 2-4 hours. A side effect of methylergometrine is an increase in blood pressure in the body. You need to be careful if the pressure is higher than usual.
 14 Watch your mother's breathing. The nurse should be aware of any changes in the body, such as the accumulation of fluid within the body, by constantly listening to the sounds of breathing. This is done to detect fluid in the lungs.
14 Watch your mother's breathing. The nurse should be aware of any changes in the body, such as the accumulation of fluid within the body, by constantly listening to the sounds of breathing. This is done to detect fluid in the lungs.  15 Assess the woman's condition when she feels better. The last step in the nursing process is assessment. The assessment will check any concerns about the woman suffering from bleeding.
15 Assess the woman's condition when she feels better. The last step in the nursing process is assessment. The assessment will check any concerns about the woman suffering from bleeding. - The fundus of the uterus should be at the level of the navel. The uterus should be firm on palpation.
- The mother should not change pads too often (using only one every hour or so) and there should be no blood or liquid on the sheet.
- The main indicators of the state of the body should return to the normal level, which was before childbirth.
- A woman's skin should not be cold or damp, and her lips should be pink.
- Since the release of fluid in the body no longer occurs in large quantities, its diuresis should return to a volume of 30 to 60 ml per hour.This shows that a woman has enough fluid in her body for normal circulation.
 16 Check the woman for any open wound that could weaken her. If the bleeding was due to an injury, the doctor should suture any open wounds. These wounds should be monitored continuously to make sure the stitches have not come apart.
16 Check the woman for any open wound that could weaken her. If the bleeding was due to an injury, the doctor should suture any open wounds. These wounds should be monitored continuously to make sure the stitches have not come apart. - There should be no severe pain, although there may be some local pain due to the sutured wound.
- If there has been accumulation of blood inside muscles or tissues, treatment should help remove the purplish-black, bluish skin tone.
 17 Check medications for side effects. The medicines mentioned earlier should be checked regularly for any side effects until you stop using them. Although monitoring of the treatment for PPH is done in collaboration with the doctor, the nurse will also be able to assess the effectiveness of the intervention by monitoring the gradual improvement of the woman's condition.
17 Check medications for side effects. The medicines mentioned earlier should be checked regularly for any side effects until you stop using them. Although monitoring of the treatment for PPH is done in collaboration with the doctor, the nurse will also be able to assess the effectiveness of the intervention by monitoring the gradual improvement of the woman's condition.
Tips
- In quantitative terms, any bleeding over 500 ml after normal delivery and over 1000 ml after cesarean section is considered PPH.
Warnings
- If there is even the slightest risk that the mother's condition will worsen, it is imperative to inform the doctor about it.