Author:
Joan Hall
Date Of Creation:
1 July 2021
Update Date:
1 July 2024

Content
- Steps
- Method 1 of 4: Quick Action
- Method 2 of 4: Stretching Exercises to Improve Circulation
- Method 3 of 4: Changing Your Lifestyle
- Method 4 of 4: Medical Assistance
- Tips
- Warnings
Swollen (varicose) veins cause pain and ruin your appearance. Veins can swell for many reasons, although varicose veins are most often indicative of blockage of veins by blood clots or slowing of blood flow. Common causes of varicose veins are pregnancy, hereditary predisposition, overweight, old age, and thrombophlebitis (inflammation of a vein and blood clot formation). At the same time, blood vessels swell under the skin, which can sometimes be accompanied by pain. In most cases, varicose veins can be dealt with at home. Act without delay - if you leave everything as it is, varicose veins can worsen over time.
Attention:the information in this article is for informational purposes only. Before using any methods, consult your doctor.
Steps
Method 1 of 4: Quick Action
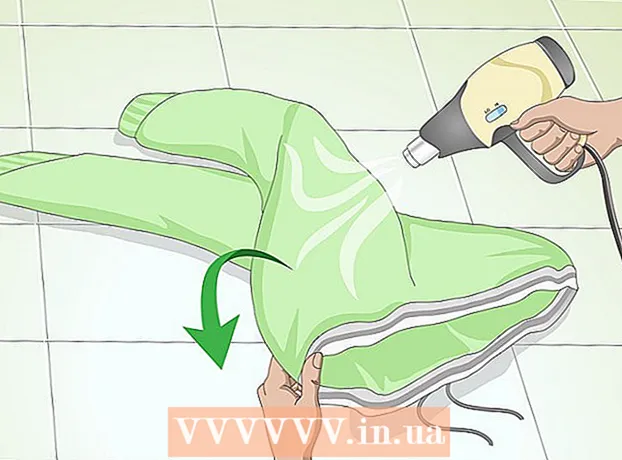
 1 Put on compression stockings. One way to relieve varicose veins is to use compression stockings. These stockings tightly squeeze the legs and help blood flow through the veins, thereby reducing the diameter of the blood vessels and improving blood circulation. There are two types of compression stockings commercially available that can be purchased without a prescription. You can also ask your doctor to prescribe stronger stockings.
1 Put on compression stockings. One way to relieve varicose veins is to use compression stockings. These stockings tightly squeeze the legs and help blood flow through the veins, thereby reducing the diameter of the blood vessels and improving blood circulation. There are two types of compression stockings commercially available that can be purchased without a prescription. You can also ask your doctor to prescribe stronger stockings. - Follow the recommendations for use, which should indicate when and for how long the compression stockings can be worn. Examine the skin under the stockings several times a day. Advanced age, diabetes mellitus, nerve damage, and several other conditions increase the risk associated with prolonged pressure and skin infections. Compression stockings should be the right size for you and not too tight.
- Supporting tights. These are just tights that are tight enough to put relatively little pressure on your legs. These tights put pressure on the entire leg, and not on any particular part, and they can be useful for mild varicose veins.
- Over-the-counter gradient compression stockings. These stockings can be purchased at the pharmacy, they exert more directed pressure. Look for stockings labeled "gradient" or "graduated compression".
- Ask your doctor to prescribe gradient stockings for you. Some compression stockings put more pressure on the leg. Compression stockings can be matched to different areas of the leg to maximize pressure. Wear stockings according to directions for use. If prescribed by your doctor, do not stop wearing compression stockings without first consulting them.
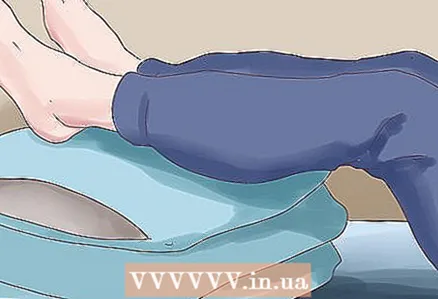 2 Raise your legs. To let the blood flow from your legs back to your heart, lie down and lift your legs above the level of your heart. Keep them in an elevated position for at least 15 minutes, 3-4 times a day.
2 Raise your legs. To let the blood flow from your legs back to your heart, lie down and lift your legs above the level of your heart. Keep them in an elevated position for at least 15 minutes, 3-4 times a day. - To lift your legs above heart level, you can place a pillow under them, or lie on the sofa and put your feet on the armrest, or lean back in a chair and put your feet on the chair in front of you.
- Do not lift your legs more than six times a day, as this puts additional pressure on the veins.
 3 Take non-steroidal anti-inflammatory drugs (NSAIDs) to reduce swelling. NSAIDs help relieve varicose veins. These drugs block the release of prostaglandins, which cause swelling and pain. To avoid stomach pain and acidity, take NSAIDs on a full stomach.
3 Take non-steroidal anti-inflammatory drugs (NSAIDs) to reduce swelling. NSAIDs help relieve varicose veins. These drugs block the release of prostaglandins, which cause swelling and pain. To avoid stomach pain and acidity, take NSAIDs on a full stomach. - Talk to your doctor before taking NSAIDs. He will recommend the correct dosage for you. Do not take NSAIDs for more than two weeks in a row, as this can lead to unwanted side effects, such as stomach or intestinal ulcers.
- Common NSAIDs include aspirin, ibuprofen (Nurofen), naproxen, and ketoprofen (Pentalgin).
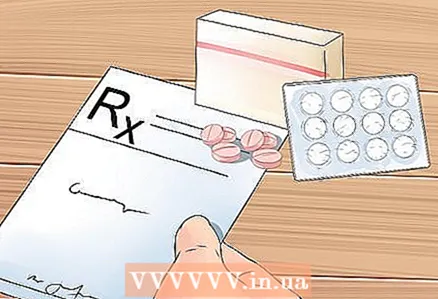 4 Consider taking other medications. Thrombophlebitis may require medications that thin the blood and dissolve blood clots. Talk to your doctor about prescribing the right medication for you.
4 Consider taking other medications. Thrombophlebitis may require medications that thin the blood and dissolve blood clots. Talk to your doctor about prescribing the right medication for you. - Blood thinning medications (anticoagulants) prevent blood clots and improve blood flow through the veins. Common anticoagulants include drugs such as heparin, fondaparinux (Arixtra), warfarin (Warfarin-FS), rivaroxaban (Xarelto).
- Blood clot-dissolving drugs act on already formed blood clots, they are usually more expensive and are used in more serious cases. These drugs include alteplase ("Aktilize"), which dissolves blood clots present in the veins.
 5 Reduce swelling with natural remedies. If you are unable or unwilling to take NSAIDs, consider using natural remedies. Before using any natural remedies, you should also consult with your doctor about the correct dosage and make sure they will not interact with any medications you are already taking.
5 Reduce swelling with natural remedies. If you are unable or unwilling to take NSAIDs, consider using natural remedies. Before using any natural remedies, you should also consult with your doctor about the correct dosage and make sure they will not interact with any medications you are already taking. - Licorice root extract is suitable for both external and internal use. Make sure the solution is at the correct concentration. Licorice root extract is not recommended for heart disease, hormone-sensitive cancers (breast, ovarian, uterine or prostate cancer), high blood pressure, diabetes, liver or kidney disease, low potassium, erectile dysfunction, pregnancy or breastfeeding.
- Apply calendula to the affected area and tie it with a bandage or wear stockings.
- Epsom salt baths can also help relieve varicose veins. Fill the tub with water, add 1–2 cups (250–500 grams) of Epsom salts and wait for it to dissolve. You don't have to plunge into the water entirely, just sit back and relax. Take at least one bath a week, or soak your feet with Epsom salts daily.
Method 2 of 4: Stretching Exercises to Improve Circulation
 1 Stretch your legs when you have to sit for long periods. If you work at a desk, sit in a car or plane, or just spend a lot of time at home, remember to warm up several times a day. Sitting for extended periods of time can impair circulation and cause varicose veins. There are various stretching exercises that can be done even while sitting.
1 Stretch your legs when you have to sit for long periods. If you work at a desk, sit in a car or plane, or just spend a lot of time at home, remember to warm up several times a day. Sitting for extended periods of time can impair circulation and cause varicose veins. There are various stretching exercises that can be done even while sitting. - Extend your legs under the table so that only your heels are touching the floor.
- Bend your toes and hold your toes extended for 30 seconds. At the same time, you should feel how the calf muscles are tense. However, do not pull your socks too far to avoid causing pain.
- Pull your socks forward and hold them in this position for 30 seconds. You will feel tension in your calf muscles, but be careful not to hurt.
 2 Stretch your chest a couple of times a day. It's not just the leg muscles that should be stretched. Stretching and strengthening your chest and back muscles will help you maintain correct posture. In turn, correct posture promotes normal blood circulation throughout the body.
2 Stretch your chest a couple of times a day. It's not just the leg muscles that should be stretched. Stretching and strengthening your chest and back muscles will help you maintain correct posture. In turn, correct posture promotes normal blood circulation throughout the body. - Sit in a chair and straighten your back. Imagine a tight rope hanging from the ceiling to keep your back straight. Cross your fingers and place your hands, palms up. Raise your chin, tilt your head back and look up at the ceiling. Take a deep breath in this position, then exhale and relax.
 3 Take advantage of any break throughout the day. Whether you're sitting at your desk or driving a car, take every opportunity to get up and stretch. Take short breaks to stretch your muscles.
3 Take advantage of any break throughout the day. Whether you're sitting at your desk or driving a car, take every opportunity to get up and stretch. Take short breaks to stretch your muscles. - If you have to drive a car for a long time, get off at gas stations, take short breaks to visit the restroom, or just leave the car for a short while and enjoy the surrounding view. You don't have to get out of your car just when you need to fill up the tank or visit the restroom. Taking short breaks will help you stretch your legs and improve circulation.
- If you work at a desk, remember to get up throughout the day. Instead of sending an email to a colleague, walk into their office and talk to them in person. During lunchtime, do not eat at your table, but try to walk a little for a snack somewhere else.
- This can be challenging on a long flight. However, you can walk around the cabin and then return to your seat. You can also go to the restroom.
Method 3 of 4: Changing Your Lifestyle
 1 Learn to recognize the symptoms of varicose veins. If you experience these symptoms, treatment should be started and it may be worth seeing a doctor. The sooner you take the appropriate action, the sooner you can relieve your condition. Varicose veins appear only in those places where the dilated veins are located.
1 Learn to recognize the symptoms of varicose veins. If you experience these symptoms, treatment should be started and it may be worth seeing a doctor. The sooner you take the appropriate action, the sooner you can relieve your condition. Varicose veins appear only in those places where the dilated veins are located. - Common symptoms of varicose veins include: fullness, heaviness, itching and aching pain in the legs, mild swelling of the feet and ankles. It is possible that dilated veins will appear under the skin, especially on the legs.
- More serious symptoms include leg swelling, pain in the legs (including the ankles) after sitting or standing for extended periods, discoloration of the skin on the legs and ankles, dry, irritated, flaky or cracked skin, long-term sores on the skin, thickened and hardened skin on the legs and ankles.
 2 Try not to stand for long periods. Standing for extended periods of time can lead to tension in the legs, which can lead to pain and impair circulation. If you have to stand, take breaks to sit down and get some rest.
2 Try not to stand for long periods. Standing for extended periods of time can lead to tension in the legs, which can lead to pain and impair circulation. If you have to stand, take breaks to sit down and get some rest. - Don't cross your legs when sitting. If possible, try to keep your legs elevated so that blood does not accumulate in them. On occasion, you can lie down and raise your legs above the level of your heart - this will help to further reduce the blood flow to your legs.
 3 Don't cross one foot over the other when you are sitting. This posture impairs blood circulation. Insufficient blood circulation can restrict blood flow in the veins and lead to stretching of the veins in the legs.
3 Don't cross one foot over the other when you are sitting. This posture impairs blood circulation. Insufficient blood circulation can restrict blood flow in the veins and lead to stretching of the veins in the legs.  4 Exercise. Choose sports that strengthen your leg muscles. The contraction of the leg muscles helps the blood return to the heart and other parts of the body and thereby relieves the pressure on the veins in the legs. Even simple flexion and extension of the leg while sitting can facilitate blood flow through the veins.
4 Exercise. Choose sports that strengthen your leg muscles. The contraction of the leg muscles helps the blood return to the heart and other parts of the body and thereby relieves the pressure on the veins in the legs. Even simple flexion and extension of the leg while sitting can facilitate blood flow through the veins. - For varicose veins, exercises such as walking, jogging and swimming are recommended. In particular, when swimming, the body is in a horizontal position, and therefore the blood does not retain in the legs and puts less pressure on the veins.
 5 Lose excess weight. If you are overweight, consider losing weight to help relieve swollen veins. Excess weight puts additional stress on the lower body, including the legs and feet. As a result, the legs require extra blood, which contributes to varicose veins.
5 Lose excess weight. If you are overweight, consider losing weight to help relieve swollen veins. Excess weight puts additional stress on the lower body, including the legs and feet. As a result, the legs require extra blood, which contributes to varicose veins. - To lose weight, try to control your diet. Limit portion sizes and make sure your diet is well balanced. Your diet should include lean proteins, low-fat dairy products, whole grains and fiber, healthy vegetable fats, and fresh fruits and vegetables. Avoid sweets, fried and processed foods, and foods high in trans and hydrogenated fats.
- Discuss your weight loss plan with your doctor. The specialist will determine whether you are setting goals for yourself and will advise you on how best to achieve them. In addition, your doctor will be able to recommend an appropriate diet based on your medications.
 6 Quit smoking. Smoking is not only bad for your overall health, but it also increases pressure in your veins. Substances contained in cigarettes are very harmful to blood vessels, including the walls of veins. Quitting smoking will help prevent varicose veins.
6 Quit smoking. Smoking is not only bad for your overall health, but it also increases pressure in your veins. Substances contained in cigarettes are very harmful to blood vessels, including the walls of veins. Quitting smoking will help prevent varicose veins.
Method 4 of 4: Medical Assistance
 1 Talk to your doctor about sclerotherapy. This is a relatively painless procedure in which a liquid substance or saline solution is injected into the veins, which causes the walls to stick together and the subsequent resorption of the vessels. Sclerotherapy is used to treat mild varicose veins or arachnoid vessels. Several treatments may be needed at intervals of 4-6 weeks. After the next procedure, an elastic bandage may be applied to the legs to reduce swelling.
1 Talk to your doctor about sclerotherapy. This is a relatively painless procedure in which a liquid substance or saline solution is injected into the veins, which causes the walls to stick together and the subsequent resorption of the vessels. Sclerotherapy is used to treat mild varicose veins or arachnoid vessels. Several treatments may be needed at intervals of 4-6 weeks. After the next procedure, an elastic bandage may be applied to the legs to reduce swelling. - There is also the so-called microsclerotherapy, which allows you to get rid of the spider veins. In this method, a solution is injected into the blood vessels through a very fine needle.
 2 Consider the possibility of laser therapy. As a rule, this method is used only for small varicose veins. It consists in the action of a laser source on areas of the skin near the expanded vein. The energy generated by the radiation heats the vein tissue and destroys nearby small blood vessels. As a result, the enlarged vein closes and after a while dissolves.
2 Consider the possibility of laser therapy. As a rule, this method is used only for small varicose veins. It consists in the action of a laser source on areas of the skin near the expanded vein. The energy generated by the radiation heats the vein tissue and destroys nearby small blood vessels. As a result, the enlarged vein closes and after a while dissolves.  3 Learn about ablation. Venous ablation is the effect of intense heat sources on the vessels, which can be radio frequency devices or lasers. In this case, the doctor pierces the vein, inserts a catheter into it, which penetrates to the groin, and passes heat through it. This heat destroys the vein and it disappears over time.
3 Learn about ablation. Venous ablation is the effect of intense heat sources on the vessels, which can be radio frequency devices or lasers. In this case, the doctor pierces the vein, inserts a catheter into it, which penetrates to the groin, and passes heat through it. This heat destroys the vein and it disappears over time. 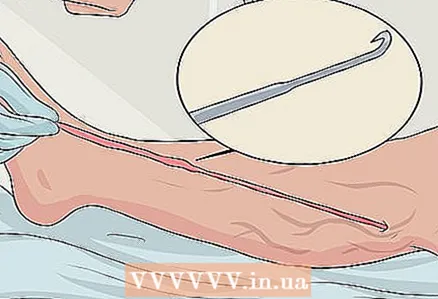 4 Talk to your doctor about outpatient phlebectomy. This surgery involves the doctor making small incisions in the skin and removing small veins through them. The veins are pulled out of the leg using small hooks. This procedure is suitable for the removal of small and spider veins.
4 Talk to your doctor about outpatient phlebectomy. This surgery involves the doctor making small incisions in the skin and removing small veins through them. The veins are pulled out of the leg using small hooks. This procedure is suitable for the removal of small and spider veins. - Under normal conditions, after this procedure, they are discharged on the same day. For phlebectomy, local anesthesia is used. After the operation, small bruises may remain, which will soon disappear.
- Phlebectomy can be done along with other procedures such as ablation. The doctor will determine if the different methods can be combined.
 5 Talk to your doctor about vein extractions. This invasive procedure removes problem veins and is usually used for severe varicose veins. The doctor makes small incisions in the skin and removes the veins from the leg. The operation is performed under general anesthesia, and the period of complete postoperative recovery takes from one to four weeks.
5 Talk to your doctor about vein extractions. This invasive procedure removes problem veins and is usually used for severe varicose veins. The doctor makes small incisions in the skin and removes the veins from the leg. The operation is performed under general anesthesia, and the period of complete postoperative recovery takes from one to four weeks. - Although the blood vessels are removed from the leg, this operation does not impair circulation, which the deeper veins in the leg do just fine.
Tips
- Feel free to do stretching exercises in public places such as on board an airliner or in your workplace. These exercises are very beneficial for varicose veins, so they are worth it.
- Do not stretch the muscles too much to the point of pain. Usually, stretching should be accompanied by only mild and tolerable discomfort that is easy to get used to.
Warnings
- If blood clots form in the blood vessels, they can travel to the lungs and cause a pulmonary embolism, which is deadly. Although this rarely happens, it is still worth discussing this danger with your doctor. Signs of pulmonary embolism include shortness of breath, cold bluish skin, irregular heartbeat, dizziness, restlessness, hemoptysis, and weak pulse.
- Varicose veins are quite common and some people are more prone to it than others. The risk of the disease increases with age, with congenital heart valve defects, obesity, pregnancy, and if someone in your immediate family has had a thrombosis or varicose veins.