Author:
Monica Porter
Date Of Creation:
21 March 2021
Update Date:
1 July 2024

Content
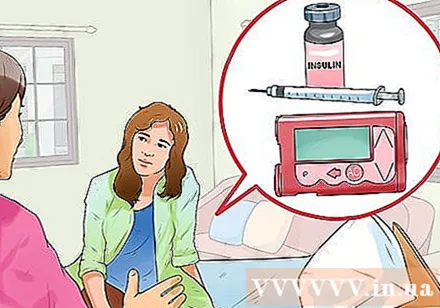
Children with diabetes need daily insulin intake to stay healthy and are likely to take it for life. Unfortunately, insulin cannot be taken by mouth and requires an injection. The best way to convince your child to get the shot is to educate them about diabetes and to encourage them to take responsibility for their own health.
Steps
Part 1 of 3: Adolescent education
Establish a team of experts. Finding a doctor who specializes in adolescent diabetes plays an important role in maintaining the best health care for your child in the years to come. Refer children to each doctor and let them know that doctors are the ones who help bring about good health. Maintain a close relationship with the team, especially as soon as any problems and major changes are diagnosed in your child's life.You need to be in contact with:
- Pediatrician who specializes in juvenile diabetes.
- Diabetes nurse.
- Nutritionist.
- Doctor specializes in endocrine disorders such as diabetes.
- Psychologist. This is the person who will help the child cope with the emotions caused by the diagnosis. Many children are often shocked, angry, and rejected before accepting the diagnosis.

Practice testing blood sugar and insulin injection with your child. Make sure they understand what is going on and why. This way, the child will feel less afraid.- If your baby is older, you can enable them to practice their own finger prick test to measure blood glucose and inject drugs.
- If your baby has a small fruit and is unable to do a finger prick test or injection on their own, you can allow them to join the process by asking them to pinch the skin during the injection. This helps to prepare the child to prepare self-medication as he gets older.

Explain the different types of insulin. This helps children understand the connection between insulin and diet and learn to control them. Depending on the child's needs, a doctor may recommend a variety of combinations. Insulin types include:- Fast acting insulin. Two common types are insulin lispro (Humalog) and insulin aspart (NovoLog). They work within 15 minutes and maximum effect in about an hour.
- Short acting insulin (Humulin R, Novolin R and others). They work within 30 minutes and are effective up to two to four hours later.
- Long-acting insulin. Some common types include insulin glargine (Lantus) and insulin detemir (Levemir). They last for 20 to 26 hours.
- Intermediate-acting insulin (Humulin N, Novolin N). They take effect after half an hour and are most effective within four to six hours. Children taking this type of insulin need to eat a sufficient amount of carbohydrates at the right time because insulin mediates the ability to lower blood sugar.
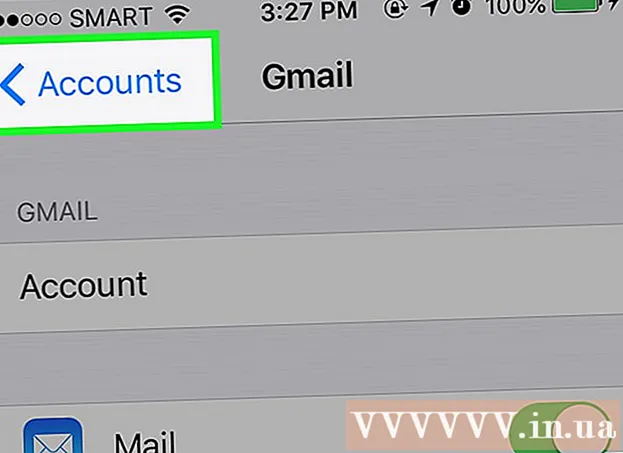
Allow your child to choose how to take the medication if he is old enough. The ability to discuss and understand how to take medications helps children take responsibility for their treatment plans. Here are a few of the available methods:- Insulin injection. This includes regular injections. It can be injected with an insulin syringe and needle or pen. The injection pen has insulin space inside.
- Insulin pump. The pump is about the size of a deck of cards and a carry on. The device is attached to a urinary catheter that is continuously implanted under the skin. The pump is programmed to fill with insulin, but can be adjusted as needed. Wireless pumps using small tubes containing insulin are a new type of pump.
Part 2 of 3: Recognize the symptoms
Supporting children to recognize hypoglycemia. This can occur from poor diet, frequent vomiting, excessive exercise, or too much insulin. You need to teach your child how to recognize symptoms and let you know when blood sugar drops. After knowing the symptoms, your child will know that controlling their diabetes helps them feel better. Some of the symptoms include: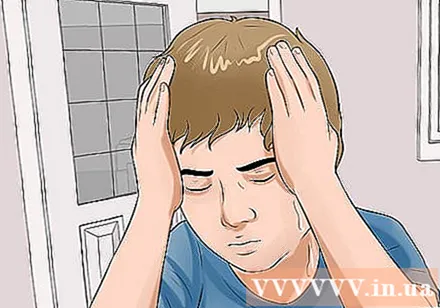
- Shivering
- Sweat
- Asleep
- Hungry
- Dizziness
- Headache
- Bad mood
- Behavior change
- Confused
- Concerned
- Convulsions
- Fainting
Teach children how to recognize hyperglycemia. Hyperglycemia is caused by eating more than usual, eating the wrong foods, not getting enough insulin, or being sick. When children begin to recognize symptoms of hyperglycemia, they will understand that medication plays an important role in recovery. Some of the symptoms include:
- Urinate often
- Thirsty
- Dry mouth
- Poor eyesight
- Fungal infections
- Struggling
- Nausea
Help your child recognize diabetic ketones. This happens when the body begins to break down fat due to lack of energy. You can teach your child how to recognize symptoms and check for the condition with drugstore urine test kits to detect high ketone levels. Symptoms of diabetic ketone production include:
- There is no feeling of hunger
- Nausea or vomiting
- Stomachache
- Dry or red skin
- The breath smells sweet or fruity
- Confused
- Tired
- Difficulty breathing or breathing deeply or quickly
Part 3 of 3: Helping your child control diabetes
Talk to the school. As children get older, they are responsible for controlling their diabetes medication while in school. Whether it's self-administered or going to the school nurse's office for the shot, it's important for your child to know how to manage his or her condition. Some things to discuss with the school include:
- Refer your child to the school health team. Make sure your child knows where the clinic is located so they can seek help and is not feeling well.
- Talk to teachers. Children need to have snacks or quick-acting sugar available. Make sure the teacher knows that children sometimes need to leave class for insulin injections or junk food.
- Consult your school about how your child should use it to get rid of a used needle. If they self-inject, they need to know where to safely dispose of needles.
Recognize the signs of a child with needle phobia. This is a common syndrome in children with diabetes. Parents and children may have difficulty getting insulin injections regularly. Children who are afraid of needles may avoid the injection or exhibit some of the following anxiety symptoms:
- Dizziness
- Dry mouth
- Heart palpitations
- Sweat
- Shivering
- Breathe too quickly or too deeply
- Fainting
- Nausea or vomiting
Help your child overcome the needle phobia. There are many ways to fix this. Your child may want to try a variety of methods to see which works. You may need to talk to a psychologist who understands the challenges your child with diabetes is facing.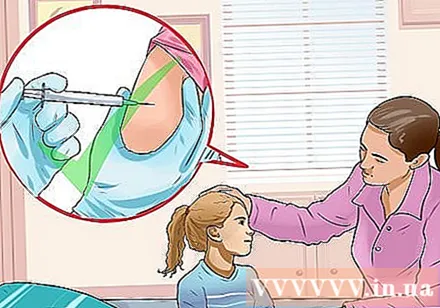
- Ask your child to sketch a hierarchy of fears. Ask your child to make a list of the parts of the injection that range from least scary to most frightening. Then start with the easiest part, such as holding the syringe or watching someone else inject, and ask your child to use relaxation techniques until the fear is gone. Practice until your child can pass the entire hierarchy.
- Teach your child to use relaxation techniques such as deep breathing, meditation, visualizing calming images, or progressive contractions and relaxation of each muscle group in the body.
- Try the injection in a different place, such as in a different room or at a loved one's home. This helps to eliminate the anxiety factor.
- Try injections on multiple body parts. Many people feel comfortable with an injection into the abdomen, but it can be injected into the thigh or buttocks. This will help your child feel the pain caused by the old shot.
- Help your child find a support group. Your doctor may know a few support groups for children with diabetes. Alternatively contact your local health center or search the internet for diabetes research and education organizations.
Help your teen practice independence. For a child with diabetes, the difficulties that arise during puberty are more complicated than usual. You need to communicate openly with your children and be aware that they can make mistakes. Teenagers often do not adhere to a diet or inject insulin due to rebelliousness or begging for friends. Some difficulties to discuss include:
- Driver. Talk to your children about the importance of ensuring safety while driving. Instruct your child on how to check blood sugar before the ride and always have snacks that can be stored in the cart. Make sure your child is aware of the need to stop and correct hypoglycemia, even when it's late. Instruct your child not to leave diabetes tools in the car as hot or cold temperatures can damage objects.
- Feel your body appearance. Some diabetics have difficulty controlling their weight. If your child is facing this challenge, you should support them. Teenagers are also at risk of having an eating disorder or quitting insulin to lose weight. They also want confidential support from a counselor or support team.
- Wine. This substance can alter blood sugar levels. In addition, the cognitive changes that occur when drunk are similar to those with low blood sugar.Make sure your kids understand that alcohol is especially dangerous for them.
Warning
- Note the child's feelings. If your child constantly experiences sadness or pessimism, or if you notice a significant change in life, such as sleep habits, friends, or school, you should take your child to a doctor to see if they are show depression.
- Talk to your child's doctor if you notice they are losing weight or are not eating.