Author:
Louise Ward
Date Of Creation:
7 February 2021
Update Date:
1 July 2024
Content
The damaged liver produces new tissue to heal itself, but a cirrhotic liver is unable to regenerate itself because it has been replaced by connective fibers and changes its structure. Early-stage cirrhosis is reversible by treating the underlying cause, but end-stage cirrhosis is often irreversible and requires a liver transplant. If left untreated, cirrhosis will eventually lead to liver failure and / or cancer. Recognizing the signs of cirrhosis will help you manage it early in the curable phase.
Steps
Method 1 of 4: Understanding Risk Factors
Consider how much alcohol you drink. Alcohol damages the liver by blocking the liver's ability to process carbohydrates, fats, and proteins. When these substances accumulate in the liver to dangerous levels, the body reacts with reactive inflammation, leading to hepatitis, fibrosis and cirrhosis. However, excessive alcohol consumption is not enough to develop alcoholic liver disease. Only 1 in 5 people who drink a lot of alcohol develop hepatitis, and 1 in 4 people develop cirrhosis.
- Men are considered "drunkard" if they drink 15 or more drinks in a week. Women are considered this if they drink 8 or more drinks a week.
- You can still get cirrhosis even if you stop drinking alcohol. However, all people with cirrhosis need to abstain from alcohol. This will help with treatment and healing, at any stage.
- Although cirrhosis is common in men, cirrhosis is usually caused by alcohol in women.

Get tested for hepatitis B and C. Chronic hepatitis and liver damage caused by both viruses will develop cirrhosis after a few decades.- Risk factors for hepatitis B include unprotected sex, blood transfusion, and sharing contaminated needles. In the US and other developed countries, this risk is less likely due to vaccination.
- Risk factors for hepatitis C infection include infection from needle sharing, blood transfusions, piercing or tattoos.
- Cirrhosis of the liver due to hepatitis C is the most common cause of liver transplant surgery.

Understand the relationship between cirrhosis and diabetes. In 15-30% of patients with cirrhosis, diabetes is a risk factor for developing “non-alcoholic steatohepatitis (NASH). Diabetes also often leads to hepatitis C - the most common cause of cirrhosis - possibly due to impaired pancreatic function.- Another cause of cirrhosis often associated with diabetes is hemochromatosis.
- This condition is characterized by iron accumulating in the skin, heart, joints, and pancreas. Iron accumulation in the pancreas leads to diabetes.
Consider your weight. Obesity leads to a wide range of health concerns, from type 2 diabetes and heart disease to arthritis and stroke. Furthermore, the excess fat in the liver causes damage and inflammation, leading to the development of non-alcoholic steatohepatitis.- To determine whether or not you have a healthy weight, use an online BMI (body mass index) calculator.
- Calculating your BMI depends on factors your age, height, gender and weight.
Know the risks of autoimmune and heart disease. If you have autoimmune conditions like inflammatory bowel disease, rheumatism or thyroid disease, you should be careful. Although these diseases do not directly contribute to cirrhosis, they do increase the risk of complications from other disorders that lead to cirrhosis. Heart disease is a risk factor for non-alcoholic steatohepatitis that leads to cirrhosis. Furthermore, heart disease is associated with right-sided heart failure, which can lead to liver congestion and heart cirrhosis.
Family history check. Certain liver diseases that lead to cirrhosis are inherited. You should consider your family history to see if you are at risk for cirrhosis:
- Iron overload disease is inherited
- Wilson's disease (copper metabolism disorder)
- Alpha-1 antitrypsin (AAT) deficiency
Method 2 of 4: Recognize Symptoms and Signs
Know the symptoms of cirrhosis. If you observe these symptoms, talk to your doctor as soon as possible. Your doctor will make a specialist diagnosis and quickly start the treatment process. If you want to know if someone else has cirrhosis, make sure that person checks with you, as there are symptoms that cannot be observed from the outside. Symptoms of cirrhosis include:
- Exhausted or feeling tired
- Easy bruising or bleeding
- Lower extremity edema (swelling)
- Jaundice (jaundice)
- Fever
- Loss of appetite or weight loss
- Nausea
- Diarrhea
- Itching (pruritus)
- Increased waist circumference
- Confused
- Sleep disorders
Look for signs of spider veins. The more specialized terms for this condition are spider angiomata, spider nevi, good spider telangiectasias. Spider veins are abnormal tufts of veins emanating from the central blood vessel with damage. They usually appear on the body, on the face and upper extremities.
- To locate a spider veins, press a piece of glass against the suspicious vein.
- The red spot in the center of the bun will beat - red as the blood flows in, and then pale as the blood flows to the smaller blood vessels.
- Large and cramped spider veins are a sign of serious cirrhosis.
- However, this phenomenon is also commonly seen in pregnant women or people with severe malnutrition. Sometimes it occurs in healthy people as well.
Observe the palm of your hand for red spots. Palmar erythema looks like patches of red spots or red spots in the palm of the hand caused by altered sex hormone metabolism. Palmar erythema mainly appears on the palm margin, along the thumb and little finger, not in the center of the palm.
- Other causes of palmar erythema include pregnancy, rheumatism, hyperthyroidism and blood problems.
Notice any nail changes. Liver disease usually affects the skin, but observing the nails can provide additional useful information. Muehrcke nails have pale horizontal stripes on the base of the nail. This is due to the inadequate production of albumin, which is only done by the liver. When pressed against the fingernail, these stripes will fade and disappear before they quickly reappear.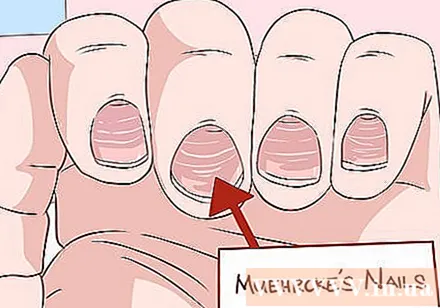
- On the nails of Terry, the two-thirds of the nail are white. One third of the tip of the nail is red. This phenomenon is also caused by a deficiency of albumin.
- The fingertips are rounded and / or larger. In a heavy form, the nails can take the form of a drumstick, hence the term "drumstick finger". This phenomenon is often seen in cholestatic cirrhosis.
Check long bones for swelling. For example, if you see a swollen knee or ankle that goes back and forth many times, it could be a sign of "osteoarthritis" (HOA). Inflammation: This is the result of chronic inflammation in the connective tissue around the bones, which can be very painful.
- Note that the common cause of HOA disease is lung cancer and should be ruled out.
Look for bent finger signs. "Dupuytren spasm" is a condition in which tissue that connects parts of the palm of the hand thickens and contracts. This affects the finger flexibility, causing the fingers to bend permanently. Usually this occurs in the ring and little finger and is accompanied by pain, soreness or itching. It is difficult for the patient to hold objects because this disease affects the grip.
- Dupuytren spasms are common in alcoholic cirrhosis, accounting for about a third of all cases.
- However, this also occurs in smokers, drinkers without cirrhosis, workers with repetitive hand movements, diabetics and Peyronie patients.
Check for solid mass in male breasts. Gynecomastia in men is the growth of mammary gland tissue that expands from the nipple. This leads to an increase in the hormone estradiol and accounts for two-thirds of cirrhosis cases. The gynecomastia may appear like the gynecomastia, where the breast enlarges due to fat but not due to an increase in mammary glands.
- To distinguish the two above cases, you lie on your back, place your thumb and index finger on each breast.
- Slowly push the breasts together. You should feel the solid, solid tissue just below the nipple area.
- If you feel the mass, there is gynecomastia. If the mass is not palpable, the prostate gland is feminized.
- Other tumor disorders, such as cancer, are often located in unusual places (not around the nipples).
Watch for symptoms of hypogonadism in men. Men with chronic liver diseases such as cirrhosis reduce testosterone production. Symptoms of hypogonadism include erectile dysfunction, infertility, decreased libido, and testicular atrophy. It can also be caused by damage to the testicles or from problems in the hypothalamus and pituitary gland.
Watch for signs of abdominal pain and bloating. These may be ascites signs that are fluid accumulating in the peritoneum (abdominal cavity). If a lot of fluid builds up, shortness of breath may occur.
Examine your abdomen for floating blood vessels. Caput medusa is an open umbilical vein that causes blood to accumulate in the portal vein system. This blood flow is then diverted into the umbilical vein and into the blood vessels in the abdominal wall. This condition makes the blood vessels stand out on the abdomen. This phenomenon is called caput medusa, because the shape of the blood vessels resembles the head (caput) of Medusa, a figure from Greek mythology.
The breath smells musty. Musty breath is also caused by severe cases of high blood pressure causing caput medusa and Cruveilhier-Baumgarten murmur. The bad smell comes from dimethyl sulfide, which is the result of hypertension.
- The sound will be quieter as the doctor presses the skin above the navel.
Pay attention to jaundice of the skin and eyes. Jaundice is a yellow discoloration caused by increased bilirubin concentrations when the liver is unable to process it efficiently. The mucous membranes may also turn yellow and the urine will become darker.
- Jaundice can also be caused by eating too much carotene such as carrots. However, carrots will not turn the whites of the eyes yellow, as is the case with jaundice.
Check your hand for symptoms of motor posture thinking (asterixis). Ask the person who is suspected of having cirrhosis to open his hands in front of his face, palms face down. The person's hand will begin to move and "wave" at the wrist like a bird's wing.
- Motor posture failure also occurs in hyperemia syndrome (uremia) and severe heart failure.
Method 3 of 4: Professional Diagnosis
Ask your doctor to check for any change in the size of the liver or spleen. When probed, the cirrhotic liver often feels stiff and has lumps. Splenomegaly (enlarged spleen) is caused by hypertension that causes congestion in the spleen. Both of these conditions are signs of cirrhosis.
Ask your doctor to check for Cruveilhier-Baumgarten murmur. Most primary care doctors do not check for this symptom. This is a blowing in the veins heard by a stethoscope in the epigastric (upper central part) of the abdomen. Like the caput medusa, this phenomenon is caused by malfunctioning of the interconnection of different venous systems in the body when there is an increase in blood pressure in the veins.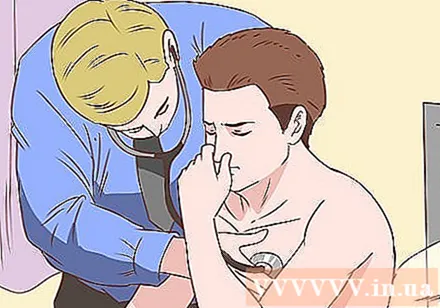
- The doctor will perform the Valsalva maneuver - a technique to probe increased abdominal pressure. This helps the doctor to hear the blow more clearly if any.
Have your doctor do a blood test for cirrhosis. The doctor will take blood and send it to a laboratory to diagnose cirrhosis. These tests include: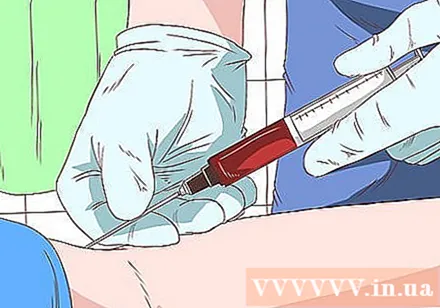
- A complete blood count test for anemia, leukopenia (leukopenia), neutropenia, and thrombocytopenia are common in cirrhosis and several factors. other.
- The test looks for elevated levels of liver enzymes (serum aminotransferases), which indicate alcoholic cirrhosis. Common alcoholic cirrhosis of the liver has a ratio of AST / ALT greater than 2.
- Measure your total bilirubin level compared to your baseline allowance. Results will likely be normal in the early stages of cirrhosis, but levels will increase as the cirrhosis worsens. Note that elevated bilirubin levels are a bad prognostic sign in primary biliary cirrhosis.
- Measure the level of albumin. A cirrhotic liver's inability to synthesize albumin results in low albumin levels. However, this is also seen in patients with congestive heart failure, nephrotic syndrome, malnutrition and certain intestinal diseases.
- Some other tests include the alkaline phosphatase test, the liver enzyme gamma-glutamyl transpeptidase (GGT), prothrombin time, globulins, sodium serum, and hyponatremia (hyponatremia).
Ask your doctor to review images. Body imaging may help identify cirrhosis, but it is even more helpful in detecting complications of cirrhosis such as ascites.
- Diagnostic ultrasound is a non-invasive and accessible method. On ultrasound, a small, lumpy cirrhosis of the liver will be found. The typical finding of cirrhosis is that the right lobe shrinks and the left lobe enlarges. Lumps seen on ultrasound may be benign or malignant and require biopsy. Ultrasound can also detect an increase in portal vein diameter or the shape of the branch veins, indicating an increase in portal venous pressure.
- Computer tomography is often not used in diagnosing cirrhosis, as it gives the same information as ultrasound. Furthermore, the patient is exposed to radiation and contrast. You can consult for other opinions or ask why your doctor recommends using this technique.
- Magnetic resonance imaging is often limited due to the high cost and rejection of patients due to the long and uncomfortable imaging times. Low signal levels on T1-weighted images indicate iron overload due to hereditary hemochromatosis.
Do a biopsy for a definitive diagnosis. Checking for signs and symptoms and doing blood tests are good methods to identify a suspected cirrhosis. However, the only way to know for sure if you have cirrhosis is with a biopsy. After processing and examining a piece of liver under a microscope, the doctor can confirm whether the patient has cirrhosis or not. advertisement
Method 4 of 4: Getting Treatment for Cirrhosis of the liver
Follow the instructions of your healthcare provider. In cirrhosis, most mild and moderate cases are usually treated outpatient, with a few exceptions. If the patient has gastrointestinal bleeding, severe infection or sepsis, kidney failure or altered mental status, inpatient treatment is required.
- Your doctor will ask you to abstain from alcohol, drugs, and drugs if your liver is contaminated. Your doctor will evaluate this condition individually. What's more, some herbs like kava and mistletoe can cause further damage to the liver. Talk with your doctor about the herbal / alternative treatments you are taking.
- Your doctor will give you vaccinations for pneumococcal disease, flu, hepatitis A and B.
- Your doctor will develop a NASH regimen for you, under which you will be part of a plan for weight loss, physical exercise and optimal control of lipids and glucose (fats and sugars / carbs).
Take medication according to the instructions. As mentioned above, there are many potential causes of cirrhosis. Medications that your doctor prescribes are prescribed specifically for you. These drugs will treat the underlying causes (Hepatitis B, Hepatitis C, cholestatic cirrhosis) and symptoms from cirrhosis and liver failure.
Ready for a surgical option. Surgery is not always recommended by doctors, but it is necessary when certain conditions arise from cirrhosis. These conditions include:
- Varicose veins and can be treated with venous ligation.
- Ascites, which is a buildup of fluid in the abdominal cavity, is handled by aspiration, a procedure to drain fluid.
- Severe liver failure, which is a rapid onset of hepatic encephalopathy (changes in liver structure / function for 8 weeks after cirrhosis is diagnosed). This condition requires a liver transplant.
- Liver cell carcinoma is the development of liver cancer. Treatment efforts include radiofrequency ablation, surgical removal (removing cancer cells), and liver transplantation.
Know your prognosis. Usually after being diagnosed with cirrhosis, one can experience 5-20 years with no or few symptoms. Once severe symptoms and complications from cirrhosis have appeared, a patient usually dies within 5 years without a liver transplant.
- Liver and kidney syndrome is a potentially serious complication caused by cirrhosis of the liver.This term refers to the development of kidney failure in a patient with liver failure that requires treatment for kidney failure.
- Hepatopulmonary syndrome, another serious complication of pulmonary artery dilatation in liver patients, leads to shortness of breath and hypoxemia (low oxygen levels in the blood). The treatment for this is a liver transplant.
Advice
- Do not take any medicine until and unless your doctor prescribes it. Keep your body active by taking vitamins, juices and fruits.
- The early stages of cirrhosis are reversible by treating underlying causes like controlling diabetes, abstaining from alcohol, treating hepatitis and reversing obesity to regain a normal weight.
Warning
- Late stage of cirrhosis is generally irreversible - the disease and its complications eventually lead to death, so liver transplant surgery is the only option to regain health and save the patient's life.