Author:
Lewis Jackson
Date Of Creation:
11 May 2021
Update Date:
1 July 2024

Content
Hard, dry bowel movements are very painful because the bowel obstructs the bowels and makes it difficult to move out. Making changes in your diet and lifestyle can help handle this problem. On the other hand, if the home remedies aren't working, you should see your doctor to make sure.
Steps
Method 1 of 3: Soften stool through diet
Drink a lot of water. Dehydration can cause the body to secrete more water as food moves through the digestive tract, causing stools to dry and hard. Drinking enough water helps the stools become softer and easier to move.
- Sometimes your doctor may recommend drinking about 2 liters or 8 glasses of water per day. However, this recommended amount may not be enough and needs to be increased depending on the level of activity and the climate in which you live.
- Signs of not getting enough fluids include frequent headache, fatigue, dizziness, nausea, irregular urination, dark or cloudy urine, and lack of sweat.

Eat foods that are mildly laxative and rich in fiber. Most of these foods contain sorbitol. Sorbitol absorbs water into the stool, making it soft and easier to move out.- Plum or plum juice
- Dig
- pear
- Plum
- Apple
- Dream
- Raspberry
- Strawberry
- Kinds of bean
- Small beans
- Spinach (spinach)

Increase fiber. Fiber is an indigestible ingredient in plant foods. The body pushes the fiber out without absorbing it, meaning that the fiber contributes to soft and crumbled stools for easy excretion.- Most of us do not eat the recommended amount of fiber per day, usually 25-30 g. Note that you should include both water-soluble fiber (fiber that turns into a gel-like substance in water) and fiber that is insoluble in water.
- Soluble fiber is found in oats, legumes, apples, citrus fruits, carrots and barley.
- Insoluble fiber is found in whole wheat flour, wheat bran, nuts, beans and vegetables like cauliflower and green beans.
- Many plants contain both soluble and insoluble fiber, so you can get both by eating a variety of nuts and vegetables.
- Eating more fiber is most effective when you drink more water to help dissolve the water-soluble fiber.

Maintain a healthy gut flora by eating yogurt. The digestive tract needs to maintain a balance of bacteria in order to digest food effectively. When the microbiota is out of balance, you will be more prone to constipation and inefficient absorption of nutrients. Live yeast yogurts and other fermented dairy products such as Kefir can help restore and rebalance gut bacteria. Yogurt helps resemble hard stools due to:- Irritable bowel syndrome
- Unexplained diarrhea or constipation
- Diarrhea or constipation after antibiotics kill some of the natural bacteria in your gut.
Include supplements in your diet to maintain a healthy digestive system. Note that you should ask your doctor first because some supplements can change the process of handling medicines in your body.
- Add fiber as supplements. The fiber in supplements helps make stools firmer, softer and easier to move out. These supplements are called stool laxatives and should be tried before moving on to other laxatives. Look for products that contain the active ingredients methylcellulose, psyllium husk, calcium polycarbophil and Guar Gum (eg FiberCon, Metamucil, Konsyl and Citrucel).
- Try probiotic supplements. Probiotics are bacteria and yeasts that resemble the bacteria naturally in the gut. Probiotic supplements can help if you experience recurrent diarrhea and constipation or irritable bowel syndrome.
Stimulate the intestines with a cup of coffee. Coffee has a mild laxative effect, so drinking 1-2 cups of coffee a day can help you have more regular bowel movements.
- If you have a habit of drinking coffee, you may need to drink more or your body is too accustomed to coffee and coffee no longer works.
Method 2 of 3: Lifestyle changes
Reduce consumption of foods that cause constipation. Many foods are high in sugar and fat, but very low in fiber. These foods make you feel full before you eat enough fiber, for example:
- Milk and cheese
- Red pumpkin
- Sweets like cake, pudding, candies and pies
- Pre-packaged, processed foods often contain a lot of sugar, salt, and fat.
Eat several small meals instead of just one big meal. Eating in moderation helps the digestive system to be stimulated continuously but at low intensity, while improving digestion and regular contraction of the intestines.
- Eat slowly so your body can process the food. Eating too quickly will make it easier for you to overeat and put pressure on your digestive system.
- Chew it thoroughly to facilitate digestion and maintain a healthy portion size.
Exercise for at least 30 minutes a day. Exercise stimulates the intestines to contract and move food through the intestines.
- The intensity of the activity should be strong enough to increase your heart rate, like brisk walking, swimming, jogging, or cycling.
- Sometimes this secret works surprisingly quickly. Therefore, you should exercise somewhere near the toilet.
- Talk to your doctor first if you have health problems that prevent you from exercising.
Reduce stress in your life. Research shows that stress can cause constipation and diarrhea - both health problems come with hard, dry stools. Try relaxation techniques like:
- Deep breath
- Yoga
- Meditate
- Thai Cuc kungfu
- Massage
- Listen to relaxing music
- Imagine places that relax you
- Dynamic relaxation, muscle tension - muscle relaxation, the process of going through the body and intentionally causing tension-relaxing each muscle group.
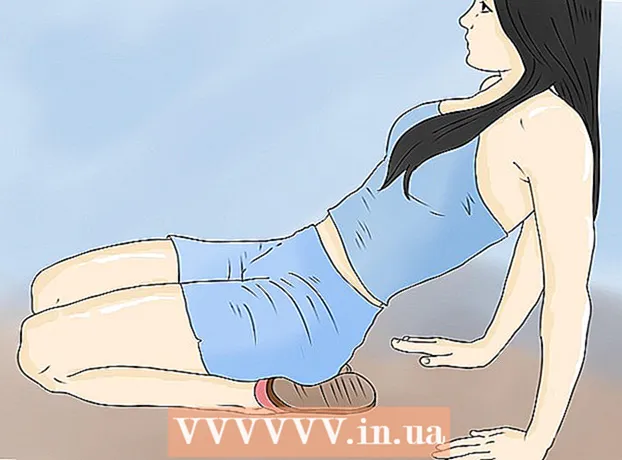
Spend time on the bathroom after each meal. You can also do relaxation techniques to stimulate bowel movements.
- Spend at least 10 minutes in the bathroom about 30 minutes after meals.
- Place your feet on a low platform and sit with your knees above your hips. This position makes bowel movements easier.
Use biofeedback to relax pelvic floor muscles. This method helps make bowel movements easier.
- Your therapist will use a machine to measure the tension in your rectum and help stretch your pelvic floor muscles.
- It's a good idea to see a therapist recommended by your doctor to ensure reliability.
Method 3 of 3: Take medications
Consult your doctor. Certain prescription medications can cause constipation, such as the opioid pain reliever. Your doctor may recommend that you change your medication or use more laxatives to treat constipation. Your doctor may recommend over-the-counter or strong prescription medications. See your doctor right away if you experience:
- Rectal bleeding
- Severe weight loss
- Tired
- Severe abdominal pain
Lubricate the intestines with a small amount of mineral oil. Consult your doctor to determine the right dose.
- Wait at least 2 hours after eating as the mineral oil can completely prevent nutrient absorption.
- Mineral oil will take effect within 6-8 hours.
- Do not use mineral oil while lying down as you can inadvertently inhale and cause pneumonia. Also for this reason, you should not give mineral oil to children under 7 years old.
- Do not use mineral oil while pregnant, as it can interfere with the absorption of nutrients and cause bleeding in the baby if taken for a long time.
Try a stool softener. These drugs take moisture from the stomach and use it to make the stool wetter.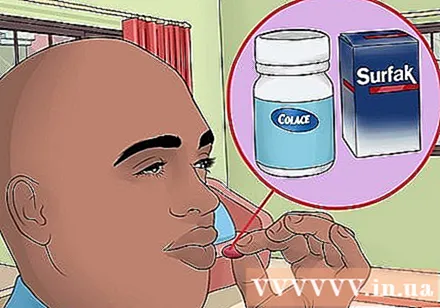
- Popular stool softeners include Colace and Surfak.
- Drink a few extra glasses of water each day while taking stool softeners.
Use an osmotic laxative to get your stool wet. These drugs create more fluid in the stomach, and at the same time stimulate stomach contraction and move stool with it. However, it takes a few days for the medicine to take effect. Common osmotic laxatives include:
- Milk of Magnesia
- Magnesium citrate
- Lactulose
- Polyethylene glycol (MiraLax)
Consider using a stimulant laxative. These medications are helpful if the stool is soft enough to move out, but the stomach does not contract to push it out. The drug will stimulate contractility and take effect after 12 hours. Common stimulant laxatives include:
- Senna
- Bisacodyl
- Sodium Picosulphate
Break the stool. If your rectum is blocked by dry, hard stools, you can use a suppository, enemas, or remove the stuffiness by hand.
- A suppository is a pill capsule that is inserted into the anus to dissolve and be absorbed.
- An enema is a liquid medicine that is inserted into the large intestine through the anus. Enemas should be done by a doctor.
- Manual stuffing is the process of requiring a doctor or nurse to put on gloves, and then insert 2 lubricated fingers into the rectum to break down and remove the lumpy stools.
Warning
- Pregnant women should not arbitrarily take drugs, including over-the-counter drugs, without consulting their doctor.
- Check with your doctor before giving medicine to young children.
- Carefully read and follow the manufacturer's instructions and doctor's recommendations.
- If you are taking other medications, using herbal ingredients or supplements, you should consult your doctor to make sure there are no drug interactions.