Author:
Laura McKinney
Date Of Creation:
7 August 2021
Update Date:
1 July 2024

Content
Itchy breasts are common in women, and can also occur in men. Many factors can lead to itchy breasts, from the use of new soap or detergents to more serious conditions including a fairly rare form of breast cancer. Itchy breasts can be persistent, extremely uncomfortable, and sometimes quite painful. Pay attention to the symptoms and take steps to treat the itchy area using over-the-counter remedies and make changes to the lifestyle and products you use often. In many cases, you will need to consult a doctor, conduct examinations, tests, and treat through stronger prescription medications.
Steps
Part 1 of 4: Treatment of itchy breasts caused by dry skin
Be aware of dry skin. Dry skin is the main cause of itchy breasts. Dry skin itching is more likely to occur in other areas of the body than on the chest. Treating existing dry skin will help prevent future problems.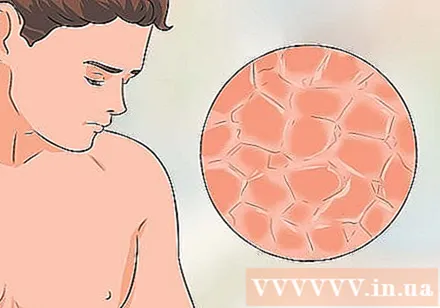
- Dry skin can develop on uneven skin. These areas are often scaly or prone to flaking. Dry skin feels tight, especially after contact with water.
- Uneven dry areas of skin are often darker or paler than normal skin tissue and may appear more wrinkled when compared to the smooth texture of healthy skin.
- Chest dryness tends to get worse during cold and dry months.

Change your bathing habits. Taking a bath or soaking in a hot tub will make the dry skin problem persist or worsen.- You should only take a bath or soak in a tub of warm water and avoid prolonged exposure to hot water.
- Use unscented, high-fat, or glycerin soaps. Stay away from scented products such as bath foaming solutions. Use a loofah or a soft washcloth and avoid rubbing your skin too hard.
- When taking a shower, you should only rub soap on your chest every 2 to 3 days. This will allow the body time to replenish the natural oils.
- Pat your skin dry after bathing and avoid wiping it too hard with a towel. Apply an odorless moisturizer right after showering.
- An alternative to applying lotion after showering is to apply the essential oil bathe right before you step out of the shower. Let your body dry naturally, do not use a towel too vigorously, especially around the itchy chest area. Bath essential oils are usually quite slippery, so be careful not to fall.
- If you are an athlete or go to the gym regularly, take a quick shower after exercising and bring your own soap.
- Limit your use of antiperspirants and perfumes as these can cause dry skin. Deodorants cause less dry skin than antiperspirants.

Protect the skin. This includes protection from the sun and harsh chemicals. Wear clothing that covers the chest area, or any unprotected skin.- Use sunscreen that contains moisturizer.
Apply skin care products throughout the day. Choose products that contain at least one of the following: glycerin, urea, sorbitol, lactic acid, pyroglutamic acid, lactate salt, and alpha hydroxyl acid.
- Remember to always use fragrance-free skincare products made specifically for sensitive skin.
- Apply a waterproof moisturizer before swimming, such as a thin layer of Vaseline cream. Bathe and moisturizer right after swimming.
- Fine, thick moisturizers like Eucerin and Cetaphil are more effective than mild body lotions. Vaseline cream is also thick enough to moisturize the skin well and is also quite cheap.

Take control of the environment when possible. You may be frequently exposed to products containing chemicals or additives, making the condition worse.- Choose laundry products that are specifically labeled for people with sensitive skin. Choose one that contains no colors and flavors.
- Use fragrance-free fabric softener. Fabric softener helps to reduce roughness when washing clothes with hard water. However, many fabric softeners can trigger an allergic reaction, so if switching to an odorless type doesn't help, you should stop using the softener altogether.
- Rinse clothes by going through one more rinse cycle to make sure all detergents and unwanted chemicals are removed.
Drink a lot of water. Drinking plenty of water every day will provide the amount of water needed to maintain a healthy body, including the largest organ in the body, your skin.
- Use a humidifier during the winter months to maintain moisture in your skin.
Wear clothes that are soft and breathable. Choose bras that are less padded and unfortunately made with stiff, itchy lace. If possible, choose cotton bras. Do not use a bra whenever possible.
- Wear shorts, blouses, or dresses that are loose fitting and made from a comfortable, breathable fabric such as cotton.
- Be sure to choose a bra that fits well, including a sports bra. Flaking and itching can be caused by a bra that doesn't fit properly.
- Take off your sports bra immediately after exercising to minimize the amount of moisture and sweat on your breast tissue.
- Do not wear a bra when sleeping. Wear comfortable, breathable, and loose-fitting nightgowns.
Avoid scratching. Trying not to scratch the itchy area is difficult, but very important in preventing complications.
- Scratching makes the skin more irritated, makes it more itchy, and can cause inflammation if the area is scratched.
- Use the palm of your hand to gently press and massage the itchy area gently, or apply a cool cloth to the area to reduce the itchiness.
- Many people scratch at night without their knowledge. You should put band-aids around your fingertips when you sleep, or put socks on your hands to avoid scratching.
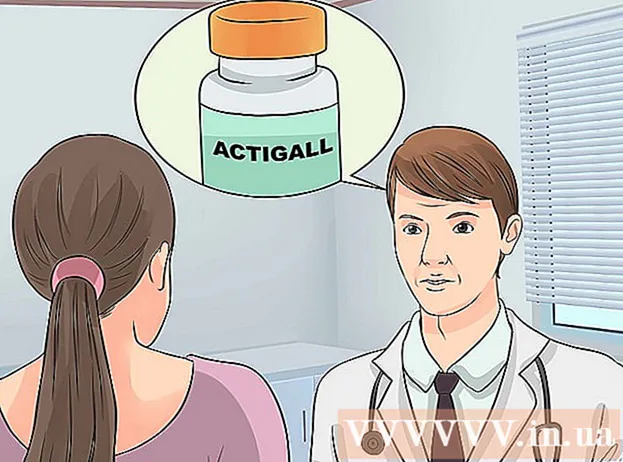
Use a cream containing 1% hydrocortisone to treat itching. You can buy over-the-counter hydrocortisone cream at most pharmacies. Apply cream to the skin to treat mild itching. You can apply 1-3 times per day.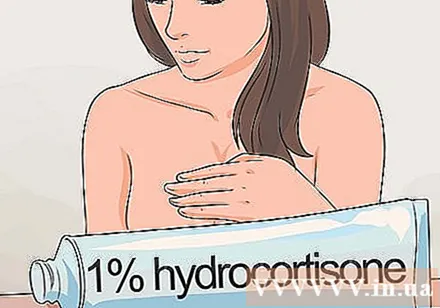
- If your symptoms do not improve within 1-2 days, seek medical attention.
- Call your doctor right away if side effects appear such as redness, swelling, or pus.
- To apply the cream, wash your skin gently and blot dry, then apply a thin layer of cream and rub it gently.
Part 2 of 4: Treatment of fungal infections of the chest
Know if you have a fungal infection. The most common place for a fungal infection on the body is in a warm, humid place that doesn't get a lot of light. The fungus is very easy to multiply under the arms, inner thighs, and below the chest.
- The under-breast fold is the fold below the chest. This area is perfect for fungus to thrive. The most common type of fungus that causes an infection under the chest is a yeast called candida.
- This type of candida yeast also causes vaginal infections and yeast infections in the mouth, also known as thrush.
- A candidiasis infection under the chest will not have serious long-term consequences, it will only darken the area permanently, and the condition is likely to spread.
Look for the rash. The rash associated with a fungal infection under the chest will be different in appearance. The rash appears in the fold between the breast tissue and the upper abdomen or chest area.
- Usually, the rash will be pink or red, itchy, with raised areas and small bumps, especially along the area with hair follicles, such as in the armpit.
- A rash is sometimes referred to as a rash caused by pigmentation.
- Infection is when an area of skin becomes infected, occurs in a warm, humid place, and when two areas of skin are pressed against each other. The rash related to ringworm can be caused by fungi, bacteria, or heavy exposure to moisture.
- Often times, this condition is accompanied by an unpleasant odor. This odor is caused by prolonged exposure to moisture and the destruction of healthy skin tissue.
Treat a fungal infection. Treatment of fungal infections involving the subcutaneous fascia can be done by altering the environment that is stimulating the growth of the fungus, and by using antifungal medications as directed by your doctor.
- To change your environment, you should take steps to avoid overlapping skin and prevent accumulation of moisture.
- Be sure to choose a bra that fits and prevent the breast tissue from sagging on the skin of the upper abdomen or chest area.
- If necessary, you can place a clean, dry cloth or a sterile padding at the bottom of your bra to absorb excess moisture and prevent the skin layers from touching.
- Wear a clean bra every day and choose loose-fitting, breathable material like cotton.
- Take off your bra whenever possible. Place a clean, dry towel or pad between the skin folds.
- For men, avoid tight shirts and tops made of fabrics that can cause you to sweat a lot. Consider wearing cotton bras to help absorb moisture.
Take steps to dry the itchy area. Make sure you dry the area under your chest thoroughly after bathing.
- After bathing, do not get dressed immediately. Allow fresh air time to contact the itchy skin.
- Lie on your back in bed or stand in front of an electric fan to let the skin fold dry completely before dressing.
Apply a cream containing aluminum acetate. Aluminum acetate 5% is available as an over-the-counter water-soluble pack or tablet for the preparation of a solution known as Burow's solution.
- This solution, often used to treat skin irritation, acts as a drying agent to help prevent the spread of the rash. As with any other product, you should consult your doctor if you are concerned about treating itchy skin at home. Seeking doctor's advice is always the right choice.
- Dissolve the packet or tablet according to the package directions and apply the solution to the rash.
- Soak a clean cloth in the solution and rub it on the rash for 15-30 minutes. Once you soak the cloth in the solution and apply it to the itchy area, do not reuse the cloth.
- Repeat this therapy about 3 times a day. Once you've removed the cloth, let your skin dry naturally before dressing.
- Discontinue use if irritation develops, or if there are any signs of allergic reaction to topical application. Signs of an allergic reaction include a rash along the area being treated, hives, blistering, or excessive itching.
- Continued use of the product beyond the recommended time on the package may result in even more dry skin.
Use an anti-fungal topical product. You can treat itchy skin with an over-the-counter antifungal product. Popular over-the-counter topical products include clotrimazole and miconazole creams.
- Stronger products used to treat fungal skin infections include nystatin-containing powder, which requires a prescription.
Seek medical attention. If the topical medication doesn't work for a few weeks, gets worse, or the itch interferes with your daily routine, consult your doctor.
- You may need a prescription for a stronger product, or an oral medication with topical use.
Treatment for mother and baby during lactation. In some cases, the mother or baby may be infected with a candida yeast or a yeast infection, and spread the infection to each other until both are effectively treated.
- If you are breastfeeding, a candidiasis rash will appear along the nipple area of the mother, and will spread to the baby's mouth, also known as thrush.
- Treating neonatal thrush and candidiasis of the chest by seeking medical attention. You should see your general practitioner or pediatrician to find a stronger prescription medication that can solve the problem for both mother and baby.
Part 3 of 4: Treatment of dermatitis or psoriasis of the chest
Make an appointment with your doctor. To effectively treat dermatitis or psoriasis of the chest, you will need a stronger prescription containing corticosteroids.
- You should not apply topical corticosteroids (including over-the-counter medications) directly to your chest without first consulting your doctor.
Identify the psoriasis spot. Psoriasis can appear anywhere on the body, including the breast tissue.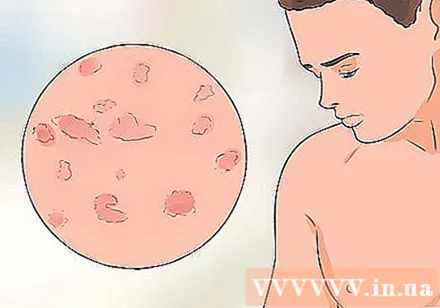
- The psoriasis will be quite thick, iridescent, sometimes red, and quite itchy and painful.
- If you experience psoriasis on your chest, you should see your doctor before taking any medicine. Be sure to use topical medications with your doctor's consent on breast tissue.
Be aware of dermatitis of the chest. Dermatitis in the chest area usually occurs in the nipples.
- The area often looks itchy, red, and sometimes has a hard crust formation and pus at the site of the pain.
See your doctor for a diagnosis of dermatitis. Since the similarity in the rash is associated with inflammatory chest dermatitis and a more serious medical condition, such as Paget's disease, medical testing is required.
- Be careful to keep the area dry, and avoid using harsh detergents or fragrant products.
Take medicines. In addition to topical medications, your doctor may prescribe oral medications to treat any existing infections, as well as prescription medications to help control itching.
- Topical products that may be prescribed include corticosteroids that help reduce inflammation and promote healing, and newer drugs, called calcineurin inhibitors. This new drug is intended only for patients experiencing severe and frequent relapses of dermatitis.
- Examples of newer active ingredients include tacrolimus and pimecrolimus. These substances help the skin to repair and prevent flare-ups of atopic dermatitis or atopic dermatitis.
Avoid scratching. In psoriasis and dermatitis, no matter where they appear on the skin, scratching can cause complications.
- Scratching causes the disease to spread, causing more skin irritation and possibly infection.
- Many people scratch at night without realizing it. Try to put bandages around your fingertips while sleeping, or wrap your hands around your hands to keep from scratching.
Part 4 of 4: Watch for serious medical conditions
Watch for symptoms of inflammatory breast cancer. This type of cancer is quite rare, ranges from only 1% - 4% of all breast cancers, and often manifests itself through itchy breasts.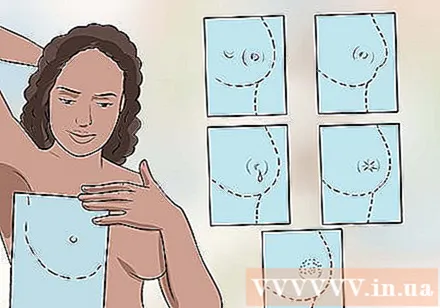
- Inflammatory breast cancers include lumps in the breast and are often accompanied by a change in the skin or breast tissue surrounding the tumor. The changes in breast tissue appear unexpectedly.
- Skin changes include itchy manifestations with pain, swelling, and redness in an area of the breast, located above and around the tumor.
- The breast tissue will become concave, similar to the skin of an orange.
- Watch for other warning signs of inflammatory breast cancer including a feeling of stiffness under the skin, warmth or heat to the touch, and pus-filled nipples.
- The nipples can also be inverted or sucked in.
Identify Paget's disease. Paget's disease is very rare, accounting for only 1% - 4% of all breast cancers. Paget's disease is a condition that looks similar to psoriasis or inflammation of the nipple skin and can cause itching.
- It begins in the nipples or areola parts, and often takes the form of a red, scaly, sometimes itchy rash. The nipples may also become flat or filled with pus.
- Most people with Paget's breast disease will have at least one lump in the breast, and about half of these people will have a sensible lump during the breast exam.
- In 90% of women with a tumor below the nipple, the cancer has spread and is considered invasive breast cancer.
- Paget's disease will be diagnosed with a tissue biopsy. Sometimes, this disease is diagnosed quite late because the symptoms appear like common skin diseases.
Remember that these conditions are quite rare. Be aware that Paget's disease and inflammatory breast cancer are very rare, accounting for only about 4% of all breast cancers.
- Seek medical help as soon as possible if you have symptoms that could be signs of either of these diseases.
- Almost any condition that causes itchy breasts is unrelated to serious medical problems.