Author:
John Stephens
Date Of Creation:
24 January 2021
Update Date:
3 July 2024

Content
Shingles, also known as herpes zoster, is a painful skin rash caused by the varicella zoster virus (VZV). This is the same virus that causes chickenpox. In people who have had chickenpox, VZV still exists in the body. Normally, this virus does not cause any problems. However, sometimes the virus becomes active and causes blisters called shingles. The following article will describe how to treat shingles.
Steps
Part 1 of 4: Diagnosis of shingles
Know the symptoms associated with shingles. Once a person is infected with the chickenpox virus, the virus stays in their body, sometimes flare up into a rash and blistering. The most common symptoms include:
- Headache
- Flu-like symptoms
- Sensitive to light
- Itching, irritation, stinging, and pain in the area where the rash started but only on one side of the body.
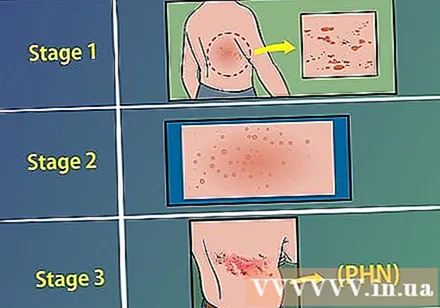
Understand that shingles has 3 stages. Determining the symptoms of each stage will help the doctor decide the best treatment for each case.- Stage 1 (before rash): itching, stinging, numbness, or pain in the area that is about to rash. Accompanied by skin irritation are diarrhea, abdominal pain and chills (usually no fever). Lymph nodes may be painful or swollen.
- Stage 2 (rash and blistering): the initial blisters begin to appear on one side of the body, gradually forming blisters. The fluid in blisters is initially clear, but then becomes cloudy. If the rash appears around the eyes, you should see a doctor immediately. A rash and blistering are sometimes accompanied by a sharp pain.
- Stage 3 (after rash and blistering appear): Pain may occur in areas where the rash appears. This is called post-shingles neuralgia (PHN), and can last for weeks, even years. PHN often leads to extreme sensitivity, chronic pain, soreness, or burning.
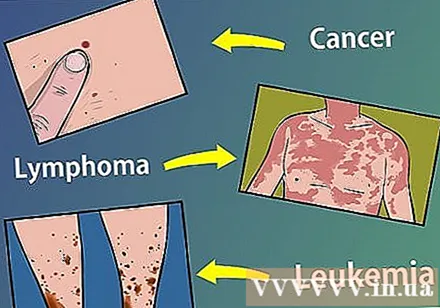
Know if you are at high risk of shingles. If you often take immunosuppressant drugs (such as steroids) after an organ transplant, you have a higher risk of shingles. You are also at high risk if you have the following conditions:- Cancer
- Lymphoma
- Human immunodeficiency virus (HIV) infection
- Leukemia
Part 2 of 4: Treatment of shingles

See your doctor early. The earlier the diagnosis of shingles, the better. (Sorry, but self-diagnosis is not recommended). Patients who start treatment within 3 days of the onset of symptoms generally have better results than patients who start therapy only after 3 days.
Talk to your doctor about treating rash and managing pain. Most shingles treatments are not too complicated, which includes treating the rash symptoms and controlling pain in the patient. Your doctor will likely prescribe the following medications:
- Antiviral medications such as acyclovir (Zovirax), valacyclovir (Valtrex), famciclovir (Famvir) to relieve pain caused by rash and shorten the duration of illness.
- Over-the-counter NSAIDS (nonsteroidal anti-inflammatory drugs) such as ibuprofen, aspirin, or acetaminophen for pain relief.
- Some antibiotics are applied topically to fight infection and prevent the spread of the rash or blisters.
See your doctor for further diagnosis if your pain persists after the rash has subsided. Your doctor may determine you have post-shingles nerve pain (PHN), which occurs in 15 out of 100 patients with shingles. In this field, the doctor may prescribe:
- Antidepressants (PHNs are often associated with depression, as some of the everyday activities become painful and / or difficult).
- Local anesthetics, including benzocaine (available over the counter) and lidocaine patch (prescription only).
- Anticonvulsants, as some studies show that these drugs have chronic pain relief.
- Opoid medications, such as codeine, for chronic pain relief.
Have some home remedies to make the shingles treatment easier. Although you should never treat shingles yourself without going to a doctor, there are some things you can do at home to combine with your doctor's prescription. These include: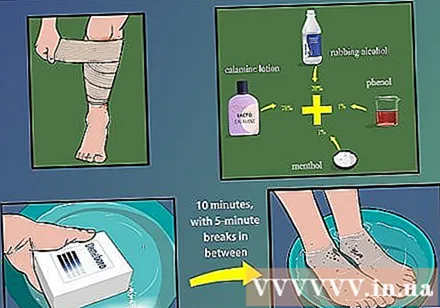
- Do not scratch and cover rashes and blisters that are too tight. You need to allow the rash and blisters to breathe, even if they crust over. If the pain keeps you awake, you can wrap the rash with a sports bandage.
- Apply ice to the affected area for 10 minutes at a time and rest for 5 minutes between sessions for several hours. Next, you can dissolve the aluminum acetate (Domeboro) with water and use a gauze dipped in the solution to moisten the rash.
- Ask your pharmacist to make the ointment. You can ask your pharmacist to mix 78% calamine lotion with 20% rubbing alcohol, 1% phenol, and 1% menthol. Apply this ointment to the blisters until they crust over.
Watch for signs of worsening illness. Some shingles have long-term complications. You should watch for the following symptoms when treating shingles or PHN: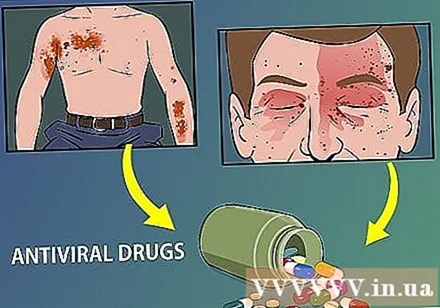
- The rash spreads to large areas of the body. This condition is called invasive zoster, which can affect internal organs as well as joints. Treatments for rampant zoster often include antibiotics and antiviral medications.
- The rash spreads to the face.This condition, called nerve shingles in the eye, can be a threat to vision if left untreated. If you notice shingles spreading to your face, see your general practitioner or ophthalmologist promptly.
Part 3 of 4: Shingles prevention
Consider whether or not to get the shingles vaccine. If you have been exposed to chickenpox and are concerned about shingles or want less painful shingles episodes, you can consider getting the shingles vaccine. This vaccine has the trade name Zostavax. People 50 years of age and older can get one shot, regardless of whether or not they have had shingles in the past.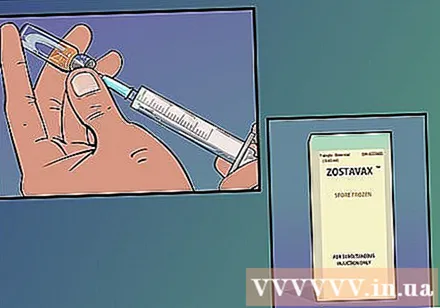
- People who have never had chickenpox or shingles should avoid getting this vaccine, with the varicella vaccine instead.
Avoid contact with infected people. People who have never had chickenpox or shingles should avoid contact with people who have these two conditions. Blisters are very contagious and should be avoided; Exposure to fluids in blisters can cause chickenpox and possible shingles outbreaks in the future.
- Shingles is more common in people over the age of 50 than in young people. People over the age of 50 should be especially wary of shingles.
Part 4 of 4: Using home remedies
Take a cool bath. Cool water will help soothe the pain and discomfort of shingles. However, keep in mind that the water must not be too cold! The extreme heat will provoke a reaction in the skin and cause additional pain. After you have finished soaking in cool water, dry yourself with a warm towel.
- You can also take an oatmeal or starch bath. Oats or starches in warm water (do not use hot or cold water), will be soothing and comforting. Read wikiHow's article How to prepare an oatmeal bath for more ideas!
- Remember to wash used towels in the washing machine in the hottest setting. You don't want germs to spread!
Use a damp washcloth. Similar to a bath, anything damp and cool makes the skin more comfortable. Just soak a towel in cool water, squeeze out the water, and apply it to your skin. After a few minutes, you can repeat the steps above to soothe your skin.
- Don't use an ice pack! The ice pack is too cold for the skin at this time - if you normally have been sensitive to the ice pack then you are even more sensitive now.
- Always wash towels after using them, especially when shingles develops.
Apply calamine lotion. Conventional lotions - especially when fragrant - can only make the condition worse. Use lotions like calamine that are soothing, and be sure to wash your hands after applying. You should only apply lotion on the affected skin area.
Use capsaicin cream. Believe it or not, capsaicin is found in hot peppers. Sure you would never dare rub chili on your face, but you may feel a softer skin when using creams containing this substance. Capsaicin cream is widely available in pharmacies.
- Remember that capsaicin cream does not cure shingles, but it will make you more comfortable. Remember that you usually recover in 3 weeks.
Apply baking soda or starch to the sore. Just put it on the sores! Baking soda and starch will dry out and help the wound heal. Simply mix 2 parts baking soda (or starch) with 1 part water to make a paste. Apply the dough for about 15 minutes, rinse and pat dry with a towel. And remember to wash the towels when done!
- You can do this a few times a day, but don't overdo it! If you apply it too many times, you can dry out the skin and make the problem worse.
Advice
- Anyone who has had chickenpox can get shingles, including children.
- There are people who should not be vaccinated or should not. People who should not get the shingles vaccine include:
- Infection with HIV / AIDS or an illness that affects the immune system.
- Are being treated for cancer with methods such as radiation therapy or chemotherapy.
- Have untreated active tuberculosis.
- Are pregnant or suspected of being pregnant. Women should not get pregnant for at least 3 months after getting the shingles vaccine.
- Have ever had a severe allergic reaction to the antibiotic neomycin, gelatin, or any ingredient in the shingles vaccine.
- Have a history of cancers that affect the lymphatic system or the bone marrow, such as cancer of the lymph nodes or leukemia.
- People with shingles can infect others when the rash is in the blistering stage; the risk disappears after the rash has crusted over.
- The virus can be passed from someone with shingles to someone who has never had chickenpox when they come into contact with the rash. People who are exposed will get chickenpox, not shingles.
- Shingles virus are not spread by coughing, sneezing or casual contact.
- The risk of shingles transmission is not high if the rash is covered.
- Take responsibility for the prevention of the spread of shingles. People with shingles should cover the rashes, don't touch or scratch the blisters, and wash their hands often.
- The shingles virus did not spread before the blisters appeared.
- Vaccination. The Advisory Committee on Immunization Practices (ACIP) recently recommended the shingles vaccine to reduce the risk of shingles in people over 60 years of age.
Warning
- 1 in 5 people continues to have severe pain even after the rash has gone. This condition is called post-shingles neuralgia. The elderly are more likely to experience neuralgia after shingles, and also more often.
- In very rare cases, shingles can lead to hearing problems, pneumonia, encephalitis, blindness, or death.