Content
Coughing is the reflex that pushes foreign material out of your lungs and keeps your upper airways clear. A chronic cough is a cough that lasts for more than 8 weeks (or 4 weeks in children) and is one of the most common problems in family health care. Often times, a chronic cough is a symptom of other medical conditions, including asthma, allergies, acid reflux or sinus problems. A chronic cough can also result from smoking, exposure to secondhand smoke or a contagious disease. If left untreated, a chronic cough can lead to complications such as headaches, dizziness, incontinence, broken ribs, abdominal pain, excessive sweating, and even conditions like chronic obstruction. count (COPD) or emphysema. Treatment for a chronic cough is highly dependent on identifying and treating the cause. If you have a chronic cough, see your doctor: although not usually dangerous, it is may is a sign of a serious illness, including lung cancer.
Steps
Method 1 of 2: Cough relief

Stay hydrated. Drink a lot of water. In general, the recommended daily intake for men is about 13 cups (3 liters) of water and for women it is about 9 cups (2-2.5 liters) of water. Water not only soothes the throat, but also helps to loosen phlegm.
Gargle with salt water. This is a long-standing remedy for coughs and sore throats. Although it does not cure a chronic cough, it can reduce swelling and provide some relief.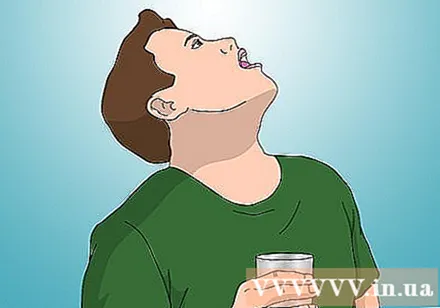
- Mix 1 teaspoon of salt with 250 ml of warm water. Gargle every few hours.

Use cough medicine. Cough medicine works by blocking the cough reflex. It is important to note that cough medicine does not treat the main cause of your cough, but only as a cough suppressant, especially if the cough disturbs your sleep.- For a long time, codeine has been considered the "gold standard" for cough medicine because it reduces the brain activity that leads to coughs. However, recent research indicates that codeine is not effective at relieving coughs. Furthermore, this drug has the ability to cause addiction and makes many patients and treaters feel uncomfortable.
- A common cough medicine is dextromethorphan (eg Triaminic Cold & Cough, Robitussin Cough, Delsym, Vicks 44 Cough & Cold). Use caution when using over-the-counter cough medicine.Always talk to your doctor before use and use the recommended dosage, follow the directions for use.
- Do not give cough medicine to children under four years old.
- If the cough has phlegm - no dry cough, don't use cough medicine.

Use cough lozenges. Most lozenges, such as Halls and Fisherman's Friend's, contain throat-soothing anesthetics.- You can buy a lozenge or "lozenge" (as it is often called) with mint extract or eucalyptus to further cleanse and soothe your airways.
- Do not give cough lozenges to children under 4 years of age as they can choke.
Eating fruit. Scientific research indicates that the fiber and flavonoid content in fruit helps prevent chronic coughs.
- Research has shown the ability to successfully treat apples, pears, and grapes. However, you can also try other brightly colored fruits like cranberries, cherries, oranges and strawberries.
Avoid allergens. If you suspect that your cough is caused by an allergic reaction, try to avoid the triggers that are causing the allergy, often including pollen, dust, grass, perfumes or perfumes and animal hair.
- You can also take an antihistamine or decongestant to relieve the cough associated with an allergy.
Use a humidifier. Using a humidifier all night helps to maintain a humid environment, repels dry air, and thus maintains a clear respiratory tract ventilation. The air that contains cool, warm, or moisture can not only reduce swelling, but also help relieve itching and dry throat.
- If you don't have a humidifier, you can also place a shallow tub of water in your bedroom at night to add moisture in the air.
- You can also take a hot shower. Similar to a humidifier, the water of the shower assists in clearing mucus from the nasal passages.
Use honey. Honey is widely used in the treatment of long-term coughs. Research has shown that honey is just as effective as the cough suppressant dextromethorphan in repelling a night cough without any side effects. You can add a teaspoon of honey to hot tea to soothe a sore throat that is sore from a non-stop cough.
- Do not use honey for children under 1 year old.
Use benzonatate (Tessalon Perles, Zonatuss). The non-narcotic benzonatate is believed to alleviate cough symptoms by reducing the cough reflex in the lungs, thereby reducing the chronic cough. Popular prescription forms of benzonatate include Tessalon Perles and Zonatuss.
- Tessalon Perles is a non-addictive capsule and is used only as directed by your doctor. This drug must be taken as a whole. Do not take more than the recommended dose due to the risk of serious side effects.
- You may need to talk to your doctor about using Tessalon Perles, as it can affect other health-related conditions, including pregnancy and other medications.
Method 2 of 2: Radical treatment
See a doctor. If your cough does not go away, make an appointment with your doctor. Your doctor will determine the cause of the cough and treat it.
- While it can be difficult, it is especially important to identify the cause behind the cough, because in most cases, once the underlying condition is identified and treated, the chronic cough stops. The three most common causes of chronic cough are asthma, posterior nasal discharge, and gastroesophageal reflux disease (GERD), accounting for 90% of cases.
- Doctors will usually begin by looking at your entire medical history and doing a physical exam. In general, your doctor will try to treat one of the most common causes of cough, and if that doesn't work, they will do additional tests, including X-rays, CT scans (computed tomography), bacteriological test, lung function test (respiratory sign), ...
- Your doctor will also ask for information about your current medications. Sometimes, prescription medications can be the cause of a cough. Angiotensin converting enzyme inhibitors, used to treat high blood pressure, are a common cause of chronic cough.
- In children, the doctor may conduct tests, including chest x-ray and lung function, if the physical examination and history do not show any clear cause.
Treatment of asthma. Coughing from asthma can come and go seasonally, but can also develop when you first have an upper respiratory infection, also known as a cold. Coughing from asthma can get worse with cold or exposure to certain chemicals or fragrances. Additionally, asthma has a form known as "cough tracheal asthma", characterized by an overreaction of the respiratory tract to pollutants and often accompanied by seasonal allergies.
- Most doctors will recommend that you use inhalers with corticosteroids to treat asthma, such as Flovent and Pulmicort, with the effect of reducing inflammation and widening the airways. Your inhaler is only available by prescription, so you will need to talk to your doctor directly. In general, the inhaler is used twice daily. The user must follow certain procedures to take effect of the inhaler: after breathing out strongly, inhale deeply, and at the same time squeeze the pump of the inhaler. Rinse mouth after use to avoid the risk of oral thrush from steroids remaining in the oral cavity.
- If you have asthma, your doctor will prescribe a bronchodilator like Albuterol to relax the airways (thus preventing coughing spasms) and help increase the amount of air entering the lungs. The drug is used 4 to 6 hours apart, as needed. However, inhaled steroids are currently the most suitable therapy for asthma that causes severe coughing.
- If your cough is caused by asthma, your doctor may also prescribe montelukast (Singulair), a cough medicine, and other symptoms.

Treatment of stomach acid reflux. This is a very common condition: stomach acid backs up into your esophagus, the tube that connects your stomach to your throat, and irritates your esophageal lining. This irritation over time can lead to a chronic cough. Coughing, on the other hand, worsens GERD, forming a vicious cycle if GERD is left untreated. If your cough is accompanied by frequent bloating or heartburn, it is more likely that GERD is the cause of your condition.- To treat GERD, you can either take an acid secretion or a proton pump inhibitor (PPI). Antacids (also known as H2 blockers) work to reduce the amount of acid your stomach secretes. The most widely recommended H2 blockers are ranitidine, or Zantac, which can be bought with or without a prescription. Ranitidine can be taken orally in tablet form. In general, most H2 blockers are taken 30 to 60 minutes before meals (but no more than twice a day).
- PPIs work by inhibiting a chemical system called the hydrogen-potassium adenosine triphosphatase enzyme system that produces stomach acids. This medication reduces the amount of acid secreted, and increases the tone of the lower esophageal sphincter, thereby preventing the acid from moving to the upper respiratory tract and triggering a cough. Only one PPI, Prilosec, is provided over-the-counter, while others, including Aciphex, Nexium, Prevacid, Protonix, and a potent Prilosec, are available by prescription. PPIs should not be used for more than 8 weeks unless directed by your doctor.
- To learn more about GERD treatments, including dietary advice, check out our acid reflux natural remedies article. Common suggestions include: avoiding foods that "trigger" coughs like fried or greasy foods, drink plenty of fluids and eat small meals throughout the day.

Treatment for posterior nasal discharge. Posterior nasal discharge occurs when mucus in the nasal passages and sinuses drains down the back of the throat. This can trigger your cough reflex. The above condition is also known as upper respiratory cough syndrome.- The standard treatment of posterior decongestant syndrome is antihistamines such as Claritin, Zyrtec Xyzal, Clarinex and decongestant group (such as Sudafed tablets and solution, Neo-Synephrine, and Afrin nasal spray). The drug is available without a prescription at the pharmacy. Follow all directions on the package and do not take more than the recommended dose because they have side effects, including dizziness and dry mouth. You should consult your doctor before use, especially if you have other health problems such as high blood pressure or are taking medication.
- Recently, Flonase, an inhaled corticosteroid, has been introduced in an over-the-counter form. It's a non-addictive nasal spray that should not be confused with decongestant decongestant sprays.

Quit smoking. Smoking is a common cause of chronic bronchitis - which can cause a chronic cough. Chronic bronchitis leads to persistent inflammation in the bronchial tubes, the major airways of the body. Injuries can become permanent if left untreated or stop smoking. In addition to a chronic cough, chronic bronchitis can also cause wheezing, an inability to breathe deeply and clearly.- Tobacco smoke also triggers coughs from other causes and can lead to serious problems like lung cancer.
- Most people with chronic bronchitis are or have ever smoked.
- It's also important to avoid secondhand smoke, as it can also lead to a chronic cough, even if you're not a smoker.
Take anti-allergy medicine. If environmental allergens are the cause of your chronic cough, an over-the-counter allergy medicine can help with symptom relief. Antihistamines (such as Claritin, Zyrtec, Tavist, Clarinex and Xyzal), antihypertensive drugs (Sudafed, Neo-Synephrine, Afrin, and Visine), and the combination of antihistamines and antihistamines (Allegra-D or Zyrtec-D) ) are commonly used drugs.
- Antihistamines work by inhibiting histamine in the cells, which is produced when the body responds to an "attack" by an allergen on the immune system. Histamine causes redness, itching, and swelling. Note that while some antihistamines can cause drowsiness, newer ones on the market are clearly labeled as not drowsy. Use as a guide.
- Decongestants help to clear the nose and are often recommended in conjunction with antihistamine use. Anti-congestion nasal sprays and eye drops should only be used for a few days at a time, as they can make symptoms worse. Liquid pills and tablets can be used for a longer time. Follow the dosage and directions on the bottle or package.
- Nasal corticosteroid sprays such as Flonase and Nasacort can be very effective at relieving the symptoms of nasal allergy and allergy-induced cough.
Take antibiotics when you have a bacterial infection. With pneumonia or bacterial sinusitis, bronchitis, tuberculosis or pertussis, your doctor will prescribe the exact type and dose of antibiotic to take, depending on your specific needs.
- Make sure to finish the treatment with the drug. For example, if your doctor prescribes 10 days of treatment, take the antibiotics as prescribed for the full 10 days, even if you feel your symptoms have improved.
Warning
- When coughing up blood or vomiting, see a doctor right away.
- See your doctor right away if your cough is accompanied by high or persistent fever, weight loss, chest pain, or difficulty breathing.
- Root treatment of chronic cough is required. If left untreated, the condition can cause irreversible damage.