Author:
Roger Morrison
Date Of Creation:
24 September 2021
Update Date:
1 July 2024

Content
- To step
- Part 1 of 3: Symptoms in adults and children
- Part 2 of 3: Signs of meningitis in babies
- Part 3 of 3: Understanding the different types better
Meningitis is an inflammation of the membranes that surround the brain and spine. Meningitis is usually caused by a virus, but it can also be caused by a bacterial or fungal infection. Depending on the type of inflammation, meningitis can either be easily treated or be life-threatening.
To step
Part 1 of 3: Symptoms in adults and children
 Watch for severe headaches. Headaches caused by inflammation of the meninges feel different from other types of headaches. It is much more severe than a headache due to dehydration or even a migraine. People with meningitis develop a persistent, very severe headache.
Watch for severe headaches. Headaches caused by inflammation of the meninges feel different from other types of headaches. It is much more severe than a headache due to dehydration or even a migraine. People with meningitis develop a persistent, very severe headache. - You cannot relieve headaches caused by meningitis with a painkiller from the drug store.
- If you have a very bad headache without any other symptoms of meningitis, the headache can also be caused by another disease. If you have a headache that lasts for more than a day, call your doctor.
 Watch for vomiting and nausea if accompanied by the headache. Migraines also often lead to nausea and vomiting, so these symptoms do not automatically indicate meningitis. However, it is important to keep an eye out for other symptoms if someone is nauseous and vomiting.
Watch for vomiting and nausea if accompanied by the headache. Migraines also often lead to nausea and vomiting, so these symptoms do not automatically indicate meningitis. However, it is important to keep an eye out for other symptoms if someone is nauseous and vomiting.  Check if you have a fever. A high fever, in addition to these other symptoms, can mean that someone has meningitis, not a cold or strep throat. Take the patient's temperature to determine if a fever can be added to the list of symptoms.
Check if you have a fever. A high fever, in addition to these other symptoms, can mean that someone has meningitis, not a cold or strep throat. Take the patient's temperature to determine if a fever can be added to the list of symptoms. - Fever in meningitis is usually around 38.5ºC, and any temperature above 39.5ºC is cause for concern.
 Feel if the neck is stiff and painful. This is a well known symptom of meningitis. The stiffness and pain are caused by pressure from the inflamed membranes. If you or the person has a sore neck that doesn't seem to be related to other common causes of pain and stiffness, such as a pulled muscle or whiplash, meningitis could be the culprit.
Feel if the neck is stiff and painful. This is a well known symptom of meningitis. The stiffness and pain are caused by pressure from the inflamed membranes. If you or the person has a sore neck that doesn't seem to be related to other common causes of pain and stiffness, such as a pulled muscle or whiplash, meningitis could be the culprit. - If this symptom flares up, have the patient lie flat on their back and flex and extend their hips. If this causes neck pain, it may be a sign of meningitis.
 Look for trouble concentrating. Because the membranes around the brain are inflamed with meningitis, cognitive problems often occur. Not being able to finish an article, not being able to concentrate on a conversation, not being able to perform a task in combination with severe headaches can be warning signs.
Look for trouble concentrating. Because the membranes around the brain are inflamed with meningitis, cognitive problems often occur. Not being able to finish an article, not being able to concentrate on a conversation, not being able to perform a task in combination with severe headaches can be warning signs. - He / she may not be himself / herself and may be sleepy or lethargic.
- In rare cases, a person may be difficult to wake up or even be comatose.
 Be aware of hypersensitivity to light. If someone is hypersensitive to light, light can cause a lot of pain. Eye pain and sensitive eyes have been associated with meningitis in adults. If you or the patient cannot go outside or be in a room with a lot of light, see the doctor.
Be aware of hypersensitivity to light. If someone is hypersensitive to light, light can cause a lot of pain. Eye pain and sensitive eyes have been associated with meningitis in adults. If you or the patient cannot go outside or be in a room with a lot of light, see the doctor. - This can present as a general sensitivity or fear of bright light. Watch for this behavior if other symptoms appear as well.
 See if anyone has seizures. Seizures are uncontrolled muscle movements, often aggressive in nature, that can lead to loss of bladder control and general confusion. Shortly afterwards, the person who has a seizure often does not know what the date is, where he / she is or how old he / she is.
See if anyone has seizures. Seizures are uncontrolled muscle movements, often aggressive in nature, that can lead to loss of bladder control and general confusion. Shortly afterwards, the person who has a seizure often does not know what the date is, where he / she is or how old he / she is. - If this person has epilepsy or has had seizures before, it may not be a symptom of meningitis.
- If you see someone having a convulsion, call 911. Put them on their side and remove any objects they could hit or kick against. Usually convulsions go away on their own after one or two minutes.
 Look for a red or purple rash. Certain types of meningitis, such as meningococcal meningitis, cause a rash on the skin. This rash is red or purple and blotchy, and it could be a sign of blood poisoning. If you see a rash, you can assess whether it is caused by meningitis using the glass test:
Look for a red or purple rash. Certain types of meningitis, such as meningococcal meningitis, cause a rash on the skin. This rash is red or purple and blotchy, and it could be a sign of blood poisoning. If you see a rash, you can assess whether it is caused by meningitis using the glass test: - Press a glass on the rash. Use clear glass so you can see the skin through it.
- If the skin under the glass does not turn white, it means blood poisoning. Then go to the hospital immediately.
- Not all types of meningitis cause a rash. If there is no rash, it does not mean that the patient does not have meningitis.
Part 2 of 3: Signs of meningitis in babies
 Be aware of the difficulties. It is very difficult to diagnose meningitis in children and especially babies, even for an experienced pediatrician. Because there are so many less serious viruses that pass on their own in children, where they develop a fever and cry a lot, it can be difficult to spot meningitis in young children and babies. That is why many hospitals and doctors' offices are very vigilant about meningitis, especially in babies 3 months and younger, especially if they have not yet had all vaccinations.
Be aware of the difficulties. It is very difficult to diagnose meningitis in children and especially babies, even for an experienced pediatrician. Because there are so many less serious viruses that pass on their own in children, where they develop a fever and cry a lot, it can be difficult to spot meningitis in young children and babies. That is why many hospitals and doctors' offices are very vigilant about meningitis, especially in babies 3 months and younger, especially if they have not yet had all vaccinations. - Vaccination has greatly reduced the number of cases of bacterial meningitis. Viral meningitis can still occur, but it is often milder and resolves on its own with minimal care.
 Watch for a high fever. Babies, like adults and children, get a high fever when they have meningitis. Check your baby's temperature to determine if he has a fever. Take your baby to the doctor if he has a fever, whether there is meningitis or not.
Watch for a high fever. Babies, like adults and children, get a high fever when they have meningitis. Check your baby's temperature to determine if he has a fever. Take your baby to the doctor if he has a fever, whether there is meningitis or not.  See if your child is constantly crying. This can be the case with all kinds of illnesses, but if your baby is very upset and does not calm down after changing, feeding, or other measures that you usually take, call the doctor. Constant crying in combination with other symptoms may indicate meningitis.
See if your child is constantly crying. This can be the case with all kinds of illnesses, but if your baby is very upset and does not calm down after changing, feeding, or other measures that you usually take, call the doctor. Constant crying in combination with other symptoms may indicate meningitis. - A baby crying from meningitis cannot be comforted. Pay attention to differences with your child's normal crying pattern.
- Some parents find that their baby cries even louder when it is lifted, if there is meningitis.
- When a baby has meningitis, he sometimes cries in a higher tone than usual.
 Watch for drowsiness and lack of activity. A floppy, sleepy, irritable child who is normally active may have meningitis. Look for noticeable changes in behavior that indicate decreased consciousness and whether it is difficult for your child to wake up completely.
Watch for drowsiness and lack of activity. A floppy, sleepy, irritable child who is normally active may have meningitis. Look for noticeable changes in behavior that indicate decreased consciousness and whether it is difficult for your child to wake up completely.  Pay attention to whether your child sucks less hard when feeding. A baby with meningitis may suck less hard when it is drinking. If your baby is having trouble sucking, call the doctor immediately.
Pay attention to whether your child sucks less hard when feeding. A baby with meningitis may suck less hard when it is drinking. If your baby is having trouble sucking, call the doctor immediately.  Look for changes in your baby's neck and body. If your baby has difficulty moving the head and the body looks unusually stiff and stiff, this could be a sign of meningitis.
Look for changes in your baby's neck and body. If your baby has difficulty moving the head and the body looks unusually stiff and stiff, this could be a sign of meningitis. - Your child may also have neck and back pain. It may just be stiff at first, but if your child seems to be in pain when it moves, it could get worse. Notice if your child automatically raises his legs when you bend his neck forward, or if it hurts when his legs are bent.
- He may also not be able to stretch his lower legs if the hips are at a 90 degree angle. This is usually noticeable when changing the diaper, when you cannot stretch your legs.
Part 3 of 3: Understanding the different types better
 Learn about meningitis viral. Viral meningitis usually resolves on its own. There are a few specific viruses such as the herpes simplex virus and HIV that do need to be treated with antiviral drugs. Viral meningitis spreads through contact between people. A group of viruses called enteroviruses are the main cause and usually emerge in late summer or early fall.
Learn about meningitis viral. Viral meningitis usually resolves on its own. There are a few specific viruses such as the herpes simplex virus and HIV that do need to be treated with antiviral drugs. Viral meningitis spreads through contact between people. A group of viruses called enteroviruses are the main cause and usually emerge in late summer or early fall. - Although it is possible to spread from person to person, an outbreak of viral meningitis is rare.
 Know what Streptococcus pneumoniae are. There are three types of bacteria that can cause bacterial meningitis, and they are the most dangerous and deadly. Streptococcus pneumoniae is the best known form infants, children and adults can get. There is a vaccine against this bacteria, so it is preventable. It usually spreads through a sinus or ear infection, and one should be aware if someone with a sinus or ear infection develops other meningitis symptoms.
Know what Streptococcus pneumoniae are. There are three types of bacteria that can cause bacterial meningitis, and they are the most dangerous and deadly. Streptococcus pneumoniae is the best known form infants, children and adults can get. There is a vaccine against this bacteria, so it is preventable. It usually spreads through a sinus or ear infection, and one should be aware if someone with a sinus or ear infection develops other meningitis symptoms. - Certain people are more at risk, such as those without a spleen and older people. Often these people are vaccinated.
 Know what Neisseria meningitidis is. Another bacteria that can cause meningitis is Neisseria meningitidis. This is a highly contagious form that can also infect healthy teens and young adults. It is passed from person to person, and sometimes there is an outbreak in school or dormitories. It is extremely dangerous and can lead to multiple organ failure, brain damage and death if not recognized and treated quickly with antibiotics.
Know what Neisseria meningitidis is. Another bacteria that can cause meningitis is Neisseria meningitidis. This is a highly contagious form that can also infect healthy teens and young adults. It is passed from person to person, and sometimes there is an outbreak in school or dormitories. It is extremely dangerous and can lead to multiple organ failure, brain damage and death if not recognized and treated quickly with antibiotics. - It's characterized by petechiae, a rash that looks like a lot of small bruises, so it's important to keep an eye out for this.
- From the National Immunization Program, children have been given a meningococcal C vaccination since 2002 when they are 14 months old.
 Learn about Haemophilus influenza. The third bacterium that can cause meningitis is Haemophilus influenza. This used to be a very common cause of bacterial meningitis in babies and children. The number of cases has decreased drastically due to the vaccination program. Due to the combination of immigrants from countries that do not vaccinate against this and parents who do not want to vaccinate, not everyone is protected against this form of meningitis.
Learn about Haemophilus influenza. The third bacterium that can cause meningitis is Haemophilus influenza. This used to be a very common cause of bacterial meningitis in babies and children. The number of cases has decreased drastically due to the vaccination program. Due to the combination of immigrants from countries that do not vaccinate against this and parents who do not want to vaccinate, not everyone is protected against this form of meningitis. - If this or any other form of meningitis is suspected, it is very important to find out the vaccination history, preferably from the medical record or the yellow vaccination booklet.
 Know that meningitis can also be caused by a fungus. Fungus meningitis is rare, occurring almost exclusively in people with AIDS or others with severely weakened immune systems. It is one of the diagnoses by which AIDS can be distinguished, and it occurs when a person has very little resistance, is extremely vulnerable, and is at risk of almost any infection. Most of the time, the culprit is Cryptococcus.
Know that meningitis can also be caused by a fungus. Fungus meningitis is rare, occurring almost exclusively in people with AIDS or others with severely weakened immune systems. It is one of the diagnoses by which AIDS can be distinguished, and it occurs when a person has very little resistance, is extremely vulnerable, and is at risk of almost any infection. Most of the time, the culprit is Cryptococcus. - The best prevention in someone with HIV is to give antiretroviral therapy to keep viral load low and T cells high to protect against this form of infection.
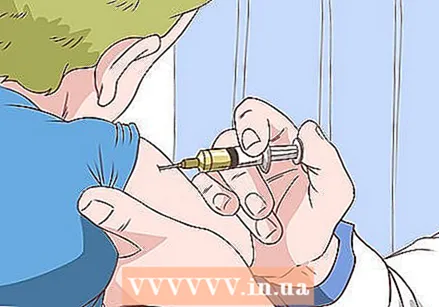
- Benefit from meningitis vaccination if needed. The following groups with a high risk of meningitis are recommended to be vaccinated:
- All children aged 14 months or older
- Soldiers
- People with a damaged spleen, or whose spleen has been removed
- Students sleeping in a dormitory
- Microbiologists exposed to meningococcus
- All people with a severely weakened immune system
- All people traveling to countries where there is an outbreak of meningitis
- All people who have been exposed to meningitis during an outbreak



