Content
Gestational diabetes is a little different from other forms of diabetes you'll ever know. Gestational diabetes occurs during pregnancy, when the body goes through many significant changes. One of these changes is changes in blood glucose, or glucose levels, in the blood. 4-9.2% of women develop gestational diabetes. Say that Not is that you and your baby have the more common type of diabetes or you and your baby will have diabetes after giving birth. Most pregnant women are screened for diabetes at 28 weeks of pregnancy. In addition to talking to your doctor at regular checkups, you can also manage your pregnancy diabetes at home. For the most part, gestational diabetes is controlled through diet, increased physical activity, and in some cases medication or insulin injections.
Steps
Method 1 of 3: Treat the disease with diet and nutrition

Cook by myself. For the treatment of gestational diabetes, natural remedies are like medical treatment, but the natural treatment diet focuses on whole foods. Food should be as natural as possible. In other words, limit your intake of processed or processed foods and cook your own as much as possible.- If you need to save time, you can use a stew pot or prepare basic dishes like rice, beans, meat and vegetables first and then freeze.
- Another ingredient when preparing your own food that can help you is cinnamon. Cinnamon is used to control blood glucose levels and is considered safe for pregnant women to consume in food, equivalent to about 1000 mg of cinnamon per day.
- Despite being promoted by many "natural" food companies, in fact, there are no studies showing that organic foods can help control gestational diabetes. It's best to eat a variety of fresh, whole foods like fruits, vegetables and whole grains.

Increase your complex carbohydrates intake. Your diet should include at least 40-50% of your daily total caloric intake from fiber-rich complex carbohydrates. Eat plenty of complex carbohydrates at noon and cut down on your serving sizes for the rest of the day. This helps to regulate blood sugar and insulin production throughout the day. Complex carbohydrates are found in whole, unprocessed foods such as whole grains, sweet potatoes, and oatmeal. Another rule to keep in mind is not to consume “white” foods, such as white bread, white pasta, or white rice, as this is a single source of carbohydrates.- Although both single and complex carbohydrates are broken down into glucose in the body, it takes longer to break down complex carbohydrates. This gives the body more time to process glucose.

Avoid processed foods. Simple carbohydrates are often found in processed foods, which contain added sugars such as glucose, white sugar, and fructose such as high fructose corn syrup. New research has shown that high intakes of high-fructose corn syrup, especially from soft drinks and other beverages high in fructose corn syrup, are associated with an increased risk of heart disease and obesity.- Reading food labels carefully can help determine the amount of sugar in processed foods, but in fact, manufacturers are not required to list the amount of added sugar. Therefore, you should avoid sweets, cookies, cakes and other sweets. The reason to avoid processed foods is because they contain both simple carbohydrates and added sugars.
- Sugar itself does not cause diabetes or gestational diabetes, but consuming foods and drinks high in sugar has been linked to an increased risk of type 2 diabetes.
Increase fiber in your diet. Fiber also helps in the treatment of diabetes. Eat beans and whole grains as they are rich in fiber. In addition, you can incorporate a teaspoon of flaxseed powder in each meal to get more fiber. You can use a coffee grinder to grind your flaxseeds yourself or buy pre-frozen powder and store it in the refrigerator to keep the healthy oils from flaxseed from spoiling.
Change the type of meat you consume. You should limit the consumption of red meat in your diet. Instead of beef, you should increase your intake of skinless fish and poultry. Look for naturally caught fish such as salmon, cod, and tuna. These fish are rich in omega-3 fatty acids that are essential for the health of both mothers and babies. Poultry skin like chicken should be removed because chicken skin contains a lot of fat.
- Make sure lean meats don't contain too much fat. Only 10-20% of the daily caloric intake comes from protein sources, including protein sources other than meat such as nuts.
Increase your vegetable intake and limit fruit. To maintain a healthy diet, you need to increase vegetables. Make sure to have at least 1-2 servings of vegetables at each meal. In addition, vegetables can also be used as a snack. On the other hand, while it's healthy, fruit should be consumed with limited consumption (no more than 2 servings per day) if you have diabetes while pregnant. This will help control your fruit's sugar intake. Avoid fruits such as pineapples, melons, bananas, grapes, and raisins because they have a high glycemic index, which means that the amount of sugar affects blood sugar more than other fruits.
- Eat fruit only at lunch instead of breakfast or dinner to help lower blood sugar in the morning and evening.
- Avoid fruit juices as they are also high in sugar, even 100% pure fruit juice.
Control your daily calorie intake. The weight gain during pregnancy is usually 8-11 kg. In general, the American Diabetes Association (ADA) recommends a daily intake of 2000-2500 calories for both mother and baby. After every 3 months, as your baby grows, the amount of calories needed will increase. However, it's best to talk to your doctor and dietitian to ensure that you are getting the right amount of calories each day based on your specific case, weight and blood sugar levels.
- During your regular check-ups, your doctor will usually refer you to a registered dietitian to help manage your gestational diabetes. Should actively ask if the doctor has not introduced. Pregnancy is a stage with many nutritional needs and if you have diabetes, this need will be even more complicated. Advice from a nutritionist will help both you and your baby.
- Be sure to follow the correct list of healthy foods to increase your calorie intake in a healthy way.
Do exercise. Exercise is very important for a healthy pregnancy. You should do at least 30-minute exercises in a row, 1-2 times a day. Walking is the simplest exercise. Alternatively, you can swim or join a Yoga class. Combine it with other activities to increase interest and strengthen other muscle groups. In addition, you can work out on the Elliptical Treadmill or on-site bike machine. Moderate physical activity helps control glucose levels.
- Avoid exercises that require lying on your back or prone to falls and injuries. Also, you should exercise regularly every day. Initially, you should exercise slowly and gradually increase to a moderate level to both strengthen the muscles and gradually increase the heart rate.
- Always listen if your doctor recommends rest or exercise as little as possible.
Method 2 of 3: Take supplements
Take a multivitamin. You will likely need multivitamins and minerals, especially iron, because during pregnancy, vitamin and mineral requirements may increase and the diet may not provide enough. Low vitamin D levels can increase the risk of gestational diabetes. You should see your doctor to check your vitamin D levels and take supplements if you have a deficiency. A daily intake of 1000-2000 IU of vitamin D is a safe level for pregnant women.
Insulin injection. Insulin therapy is a widely used natural hormone replacement therapy. This therapy may be needed to inject insulin into the body, helping to push glucose into cells. Your doctor will show you how and how much insulin to inject.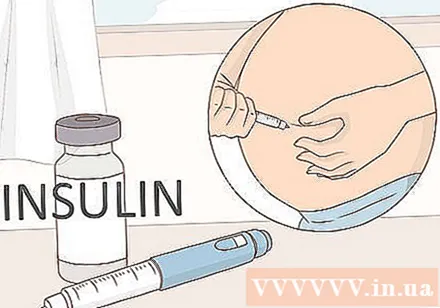
- Do not attempt to inject insulin without first consulting your doctor.
Do not arbitrarily use supplements or herbal supplements without consulting your doctor. Certain herbs and supplements can be used during pregnancy to control blood sugar levels. However, even if the product label says it is safe, you do too always right consult a doctor. This is because many herbs have not been tested for safety during pregnancy. For example, should avoid consuming bitter melon, or bitter melon (the scientific name is Momordica charantia). Bitter melon is often recommended for diabetes management but has been linked with miscarriages in animals.
- Tbsp (or Gymnema sylvestre) and prickly pear cactus (or Opuntia spp) have not been tested for safety in pregnant women, although tablespoon is not harmful for up to 20 months and prickly pear cactus Used as food for centuries.
- Tablespoon wire is usually taken in a dosage of 200 mg, twice daily; Prickly pear cactus can be taken as a single dose, 400 mg, once daily. If you want to take these two herbs, you'll need your doctor's permission.
Method 3 of 3: Understanding gestational diabetes
Understand insulin resistance. Although the cause of gestational diabetes is unknown, it has been found that some pregnant women develop insulin resistance, which means that cells in the body do not respond normally to insulin. Every cell in the body uses glucose (sugar) for the energy it needs to function. Glucose is derived from the foods you eat, mainly carbohydrates. Insulin - a hormone produced by the pancreas - is the "carrier" of the primary chemical signal that tells the cells that it is time to receive glucose. Insulin is also involved in the process of "telling" the liver to receive glucose and converting it into a stored form called glycogen.
- Insulin is also involved in many other functions such as protein metabolism and fat metabolism.
- If the cell becomes insulin resistant, the cell will either "ignore" or be unable to respond to the insulin signal. This condition increases the concentration of glucose in the blood. When this happens, the pancreas responds by producing more insulin. Since insulin does not affect insulin resistant cells, the concentration of glucose in the blood will increase. The body responds by converting glucose in the blood into fat, which in turn causes a variety of chronic inflammatory diseases and other disorders such as thriving type 2 diabetes, metabolic syndrome and heart disease.
Understand the effects of insulin resistance. If insulin resistance is not controlled during pregnancy, you may develop diabetes. Diabetes during pregnancy greatly affects the health of mother and baby. The biggest effect when the disease is not controlled is the increase in fat in the blood, which causes weight gain in the fetus, leading to difficulty in birth. Not only that, but babies are born at a higher risk of respiratory problems, obesity, lower blood sugar than normal and type 2 diabetes when they grow up.
- Mothers are at higher risk for cesarean section, postpartum type 2 diabetes, high blood pressure before and after delivery.
Recognize the symptoms of the disease. Usually, gestational diabetes in the first half of pregnancy will have no symptoms. This makes it difficult to detect the disease. However, when present, symptoms can include many of the same symptoms as type 2 diabetes:
- Vision impairment due to blurred vision or other problems
- Tired
- Easy to get skin, bladder, and vaginal infections
- Nausea and vomiting during pregnancy
- Increased appetite is associated with weight loss
- Urinate often
- Severe thirst
Diagnosis of diabetes while pregnant. To diagnose, your doctor will conduct a blood test to check your blood sugar. In addition, your doctor may order glucose tolerance tests to determine how the body processes sugar. In addition, the fetus can also be monitored (usually by ultrasound to determine if the size is normal for gestational age and check fetal heart rate using a fetal monitor.
Recognize the risk. You are at risk of gestational diabetes if you had pre-pregnancy diabetes or gave birth that weighed more than 4 kg. People who are overweight or have a parent, sibling with type 2 diabetes are also at increased risk of developing gestational diabetes.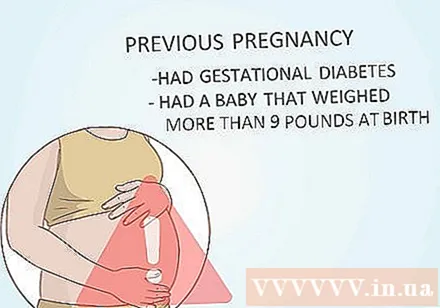
- You are also at higher risk if you were diagnosed with prediabetes, metabolic syndrome or insulin resistance before pregnancy. Metabolic syndrome is a group of problems that include high blood pressure, overweight in the waist and hips, higher than normal blood sugar and high cholesterol.
- African-American, Indian, Asian-American, Hispanic / Latina (Hispanic) or Pacific Islander Americans are at higher risk.
- Other conditions increase the risk of gestational diabetes. If you have a hormone disorder called Polycystic Ovarian Syndrome (PCOS), you have a higher chance of developing gestational diabetes. PCOS is a condition in which the ovaries contain cysts, leading to fertility and menstrual problems.