Author:
Eric Farmer
Date Of Creation:
12 March 2021
Update Date:
1 July 2024

Content
- Steps
- Method 1 of 4: Risk Factors
- Method 2 of 4: Symptoms
- Method 3 of 4: Making a diagnosis
- Method 4 of 4: Treatment
- Warnings
Piriformis syndrome is a painful condition in which the piriformis muscle (the largest muscle that rotates the hip) compresses the sciatic nerve that runs from the spine to the lower back and legs. This pressure causes pain in the lower back, thighs, and buttocks. There is no consensus among doctors regarding piriformis syndrome: some believe that this is an overdiagnosis, others that this condition often remains undiagnosed. Only an experienced doctor can make a correct diagnosis, but you can learn to recognize the symptoms yourself so you know what to expect from your doctor's appointment.
Steps
Method 1 of 4: Risk Factors
 1 Consider your gender and age. Scientists have found that women are six times more likely to develop piriformis syndrome. Most often, this syndrome develops between the ages of 30 and 50.
1 Consider your gender and age. Scientists have found that women are six times more likely to develop piriformis syndrome. Most often, this syndrome develops between the ages of 30 and 50. - The higher number of diagnoses among women can be explained by the difference in biomechanics of the female and male pelvic organs.
- In women, this syndrome can also develop during pregnancy. As the pelvis expands while the baby is carrying, the muscles attached to the pelvis may contract. A woman's pelvis is also often tilted due to the weight of the child, which also strains the pelvic muscles.
 2 Assess your health status. The likelihood of developing piriformis syndrome is increased with a number of conditions, including pain in the lower back.
2 Assess your health status. The likelihood of developing piriformis syndrome is increased with a number of conditions, including pain in the lower back. - About 15% of cases of pain in the lower back are due to a congenital or structural abnormality of the connection between the piriformis muscle and the sciatic nerve.
 3 Remember if you have had any injuries. Most often, piriformis syndrome develops due to macro- and microtraumas.
3 Remember if you have had any injuries. Most often, piriformis syndrome develops due to macro- and microtraumas. - Macrotrauma refers to any significant injury (from a fall to a car accident). Macrotrauma to the buttocks, which cause soft tissue inflammation, muscle spasms, and nerve compression, are a common cause of piriformis syndrome.
- Microtrauma is the result of repeated minor damage to a part of the body. For example, repetitive foot injuries occur in long distance runners, which can ultimately lead to nerve inflammation and muscle spasms. Prolonged running, walking, climbing stairs, and even sitting can compress the piriformis muscle and pinch the sciatic nerve, resulting in pain.
- Another type of microtrauma that can cause the development of piriformis syndrome is inflammation of the nerve due to the pressure of an object that lies in the back pocket. If a person constantly carries a phone or wallet in the back pocket of their trousers, this object can press on the sciatic nerve and cause inflammation of the nerve.
Method 2 of 4: Symptoms
 1 Observe the sources, types, and intensity of pain. One of the most common symptoms of piriformis syndrome is pain in the buttocks, as this is where the piriformis muscle is located. If you constantly experience severe pain in one of your buttocks, this could be a sign of piriformis syndrome. This disease can also be indicated by the following types of pain:
1 Observe the sources, types, and intensity of pain. One of the most common symptoms of piriformis syndrome is pain in the buttocks, as this is where the piriformis muscle is located. If you constantly experience severe pain in one of your buttocks, this could be a sign of piriformis syndrome. This disease can also be indicated by the following types of pain: - pain when sitting, standing, or lying down that lasts more than 15–20 minutes;
- pain that radiates to the back of the thigh and sometimes even to the back of the calf and foot;
- pain that goes away with movement and increases with a stationary position;
- pain that does not completely go away when changing position;
- pain in the groin and pelvis. Women may feel pain in the vagina, and men - in the scrotum;
- dyspareunia (painful intercourse) in women;
- pain during bowel movements.
 2 Pay attention to your gait. Compression of the sciatic nerve from piriformis syndrome can make it difficult for a person to walk. Legs may become weak. If you find it difficult to walk, consider if you have the following two signs:
2 Pay attention to your gait. Compression of the sciatic nerve from piriformis syndrome can make it difficult for a person to walk. Legs may become weak. If you find it difficult to walk, consider if you have the following two signs: - Antalgic gait, which is a gait that develops to relieve pain. Usually, the person begins to limp or shorten their stride to relieve pain.
- Dangling of the foot that is not controlled by the person due to pain in the lower leg. In this case, the person may not be able to shorten the foot in his direction.
 3 Pay attention to tingling or numbness. Compression of the sciatic nerve as a result of piriformis syndrome may cause a person to feel numbness or tingling in the foot or leg.
3 Pay attention to tingling or numbness. Compression of the sciatic nerve as a result of piriformis syndrome may cause a person to feel numbness or tingling in the foot or leg. - These sensations are called paresthesia.
Method 3 of 4: Making a diagnosis
 1 See your doctor. Piriformis syndrome is usually difficult to recognize because the symptoms of the disease overlap with those of the more common lumbar radiculopathy (leg numbness due to lower back pain).Both diseases are triggered by pinching of the sciatic nerve. The only difference is where the nerve is clamped. Piriformis syndrome is less common than lower back pain, so it is often not recognized by therapists. See an orthopedist, an exercise therapy doctor or an osteopath.
1 See your doctor. Piriformis syndrome is usually difficult to recognize because the symptoms of the disease overlap with those of the more common lumbar radiculopathy (leg numbness due to lower back pain).Both diseases are triggered by pinching of the sciatic nerve. The only difference is where the nerve is clamped. Piriformis syndrome is less common than lower back pain, so it is often not recognized by therapists. See an orthopedist, an exercise therapy doctor or an osteopath. - You may need a referral from a GP.
 2 Be aware that there is no single test that can accurately diagnose piriformis syndrome. Your doctor may need to take a careful look at your symptoms and do a physical exam, and schedule a series of tests to make a diagnosis.
2 Be aware that there is no single test that can accurately diagnose piriformis syndrome. Your doctor may need to take a careful look at your symptoms and do a physical exam, and schedule a series of tests to make a diagnosis. - Some tests (such as magnetic resonance imaging, computed tomography, and nerve conduction studies) can rule out a number of diagnoses (such as a herniated disc).
 3 Get inspected. To make a diagnosis, your doctor will need to check the range of motion of your muscles. Your doctor will ask you to do several exercises, including lifts and leg rotations. There are other techniques that can help identify piriformis syndrome:
3 Get inspected. To make a diagnosis, your doctor will need to check the range of motion of your muscles. Your doctor will ask you to do several exercises, including lifts and leg rotations. There are other techniques that can help identify piriformis syndrome: - Lassegh's symptom: The doctor will ask you to lie on your back, bend your leg at a 90 degree angle, and then stretch it up. The presence of Lassegh's symptom means that the pressure on the piriformis muscle in this position is causing you pain.
- Freiberg's symptom: the doctor will ask you to lie on your back, rotate your leg at the hip and lift it. If you experience pain during these movements, this will indicate possible piriformis syndrome.
- Pace symptom: you will need to lie on a side that is not painful. The doctor will bend the leg at the hip and knee and then rotate the leg at the hip, applying pressure to the knee. If you feel pain, it could mean you have piriformis syndrome.
- The doctor can also feel with his fingers the ischial notch, the protrusion in the pelvic bones through which the piriformis muscle passes.
 4 Notice the change in sensation. The doctor may check the leg that is experiencing pain for changes in sensation or loss of sensation. For example, the doctor may lightly touch the leg or induce a certain sensation with the instrument. In the leg where pain is felt, the sensations will be weaker.
4 Notice the change in sensation. The doctor may check the leg that is experiencing pain for changes in sensation or loss of sensation. For example, the doctor may lightly touch the leg or induce a certain sensation with the instrument. In the leg where pain is felt, the sensations will be weaker.  5 Let your doctor examine your muscles. Your doctor may need to evaluate the size and strength of your muscles. The leg that is experiencing pain will be weaker and possibly even shorter than the other leg.
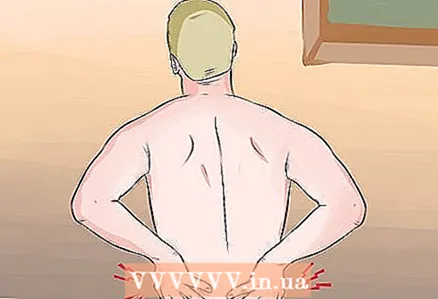
5 Let your doctor examine your muscles. Your doctor may need to evaluate the size and strength of your muscles. The leg that is experiencing pain will be weaker and possibly even shorter than the other leg. - The doctor may also feel the sciatica (the largest muscle in the buttocks) to determine the condition of the piriformis muscle. If the muscle is contracted and pinched, it will feel like a sausage to the touch.
- Your doctor will check how much pain you feel when you press on your gluteal sciatic muscle. If you feel pain or discomfort deep in your buttocks or thigh muscles when pressing, this is a sign that the piriformis muscle is contracting.
- The doctor will also look for signs of gluteal atrophy (loss of muscle tissue). In chronic cases of piriformis syndrome, muscle tissue begins to thin and shrink. This can be expressed in visual asymmetry, in which the affected buttock becomes less healthy.
 6 Ask your doctor to order a CT scan or magnetic resonance imaging for you. Although doctors can detect signs of piriformis syndrome with a visual examination, there are no diagnostic tests that can accurately diagnose. For this reason, your doctor may order a CT scan or magnetic resonance imaging (MRI) scan to determine if anything else is compressing your sciatic nerve.
6 Ask your doctor to order a CT scan or magnetic resonance imaging for you. Although doctors can detect signs of piriformis syndrome with a visual examination, there are no diagnostic tests that can accurately diagnose. For this reason, your doctor may order a CT scan or magnetic resonance imaging (MRI) scan to determine if anything else is compressing your sciatic nerve. - Computed tomography (CT) uses X-rays to create a three-dimensional image of the body inside. The tomograph records a number of projections of the spine and allows you to identify deviations from the norm in the area of the piriformis muscle and changes in the tissues of the joints.
- Magnetic resonance therapy uses radio waves and strong magnetic fields to produce images of internal organs. Magnetic resonance imaging (MRI) is used to rule out other causes of lower back pain or sciatic nerve pain.
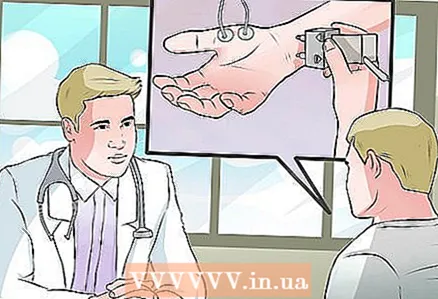 7 Ask your doctor about an electromyographic test. Electromyographic testing (EMG) is used to test how muscles respond to stimulation with electricity. This method is often used when a doctor needs to distinguish piriformis syndrome from herniated discs. In piriformis syndrome, the muscles near the piriformis muscle will respond normally to electricity, but the piriformis muscle and gluteus maximus will respond differently. In the case of a herniated disc, all muscles in this area may not respond with abnormal electricity. Electromyographic examination includes two stages:
7 Ask your doctor about an electromyographic test. Electromyographic testing (EMG) is used to test how muscles respond to stimulation with electricity. This method is often used when a doctor needs to distinguish piriformis syndrome from herniated discs. In piriformis syndrome, the muscles near the piriformis muscle will respond normally to electricity, but the piriformis muscle and gluteus maximus will respond differently. In the case of a herniated disc, all muscles in this area may not respond with abnormal electricity. Electromyographic examination includes two stages: - A nerve conduction study, in which electrodes are attached to the skin, which assess the work of motor neurons.
- Inserting a needle electrode into a muscle to detect electrical activity in the muscle.
Method 4 of 4: Treatment
 1 Do not engage in activities that provoke pain. Your doctor may recommend that you temporarily stop doing things that are causing you pain (such as running or cycling).
1 Do not engage in activities that provoke pain. Your doctor may recommend that you temporarily stop doing things that are causing you pain (such as running or cycling). - If the pain is caused by prolonged sitting, pause regularly, stand up, and stretch your muscles. Doctors recommend walking and stretching every 20 minutes. If you have to drive for a long time, stop regularly, get out of the car and stretch your muscles.
- Don't sit or stand in positions that cause pain.
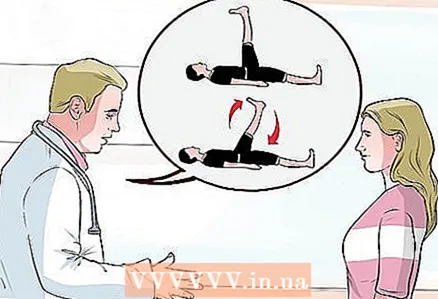
 2 Do physical therapy. Physical therapy is good for your health, especially if you start doing specific exercises as early as possible. Your doctor, together with your exercise therapy doctor, can choose an exercise system for you that will help solve the problem.
2 Do physical therapy. Physical therapy is good for your health, especially if you start doing specific exercises as early as possible. Your doctor, together with your exercise therapy doctor, can choose an exercise system for you that will help solve the problem. - Your exercise therapy doctor will show you how to do exercises related to stretching, flexion, extension and rotation of the limbs.
- Massaging the soft tissues of the gluteal and lumbosacral regions can relieve tissue irritation.
 3 Turn to alternative medicine. Chiropractic therapy, yoga, acupuncture, and massage are used to treat piriformis syndrome.
3 Turn to alternative medicine. Chiropractic therapy, yoga, acupuncture, and massage are used to treat piriformis syndrome. - Since the effectiveness of alternative medicine methods has not been scientifically proven (as opposed to more classical methods), you should discuss these treatments with your doctor before trying them.
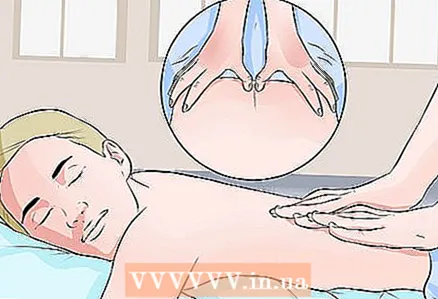 4 Treat trigger zones. Sometimes the cause of the symptoms of piriformis syndrome is the presence of trigger zones, also called muscle nodes. These are points in the piriformis or gluteus muscles. Pressure on these points can cause localized and radiating pain. Very often, pain when pressing on the trigger zones is very similar to pain in piriformis syndrome, so the results of examinations may turn out to be negative, and the diagnosis may not be established.
4 Treat trigger zones. Sometimes the cause of the symptoms of piriformis syndrome is the presence of trigger zones, also called muscle nodes. These are points in the piriformis or gluteus muscles. Pressure on these points can cause localized and radiating pain. Very often, pain when pressing on the trigger zones is very similar to pain in piriformis syndrome, so the results of examinations may turn out to be negative, and the diagnosis may not be established. - Contact a specialist who knows how to work with trigger zones: a massage therapist, chiropractor, physical therapy doctor, or even a therapist. If trigger points are the cause of the pain, a combination of acupressure and stretching and strengthening exercises can help.
 5 Ask your doctor what stretching exercises you should do and when. In addition to working with your exercise therapy doctor, your therapist can advise you on exercises to do at home. The following exercises are most often recommended:
5 Ask your doctor what stretching exercises you should do and when. In addition to working with your exercise therapy doctor, your therapist can advise you on exercises to do at home. The following exercises are most often recommended: - Roll from side to side while lying on a flat surface. Bend your knees and stretch them out on your side. Repeat the exercises, alternating legs, for five minutes.
- Stand up and stretch your arms along your body. Rotate the body for a minute. Repeat every few hours.
- Lie on your back.Bend your knees, grab your hips with your hands, and perform movements that simulate cycling.
- Bend your knee and lift it up every few hours. You can lean on a table or chair if your balance is difficult.
 6 Relieve pain with warmth and cold. A moist, warm compress can relax muscles, while an ice pack after exercise can ease pain and reduce inflammation.
6 Relieve pain with warmth and cold. A moist, warm compress can relax muscles, while an ice pack after exercise can ease pain and reduce inflammation. - If you want to make a warm compress, use a heating pad or place a damp towel in the microwave for a couple of seconds and then press it against your skin. You can also take a warm bath to relieve tension and irritation caused by piriformis syndrome. Let your body float freely in the water.
- If you want to make a cold compress, apply a towel-wrapped ice pack or a cooling bag to your body. Do not keep the cold compress on for longer than 20 minutes.
 7 Use non-steroidal pain relievers. Non-steroidal anti-inflammatory drugs relieve pain and reduce inflammation. These drugs are recommended for the relief of pain and inflammation caused by piriformis syndrome.
7 Use non-steroidal pain relievers. Non-steroidal anti-inflammatory drugs relieve pain and reduce inflammation. These drugs are recommended for the relief of pain and inflammation caused by piriformis syndrome. - The most common non-steroidal anti-inflammatory drugs include aspirin, ibuprofen (Ibuklin, Nurofen), and naproxen (Nalgezin).
- Talk to your doctor before taking these medications. They can interact with other drugs and diseases.
- If nonsteroidal pain relievers do not relieve pain enough, your doctor may prescribe muscle relaxants for you. Take them as directed.
 8 Ask your doctor about injections. If piriformis pain persists, ask your doctor about topical injections of pain relievers, steroids, or Botox.
8 Ask your doctor about injections. If piriformis pain persists, ask your doctor about topical injections of pain relievers, steroids, or Botox. - Pain relievers (most often lidocaine or bupivacaine) are injected into the trigger zone and relieve the patient's condition in combination with exercise therapy in 85% of cases.
- If local anesthetics do not relieve pain, your doctor may prescribe an injection of steroids or botulinum toxin type A (botox). Both drugs can ease muscle pain.
 9 Ask your doctor about surgical treatments. Surgery is considered a last resort in treating piriformis syndrome and is only used if all other methods have failed. If none of the treatments relieve pain, ask your doctor about surgery.
9 Ask your doctor about surgical treatments. Surgery is considered a last resort in treating piriformis syndrome and is only used if all other methods have failed. If none of the treatments relieve pain, ask your doctor about surgery. - Surgical decompression of the piriformis muscle will only be effective if there are neurological disorders. Using electromyography and other tests, the doctor will determine whether surgery to correct compression neuropathy, in which the sciatic nerve is released, can relieve pain.
Warnings
- If you experience pain in your buttocks, see your doctor for a diagnosis and start treatment as soon as possible.