Author:
Peter Berry
Date Of Creation:
16 February 2021
Update Date:
16 May 2024

Content
A woman's bladder when it gets out of position and swoops down into the vagina is called a "bladder prolapse." Anatomically, the bladder is located between the pubic bone (front) and the uterus (back) and above the vagina. Bladder prolapse, also known as bladder hernia, occurs when the muscles of the vaginal wall weaken and cannot hold the pelvic organs in the correct position. In this case, the bladder is bulging or indented in the vagina. About 11% of women need surgery to correct a prolapsed bladder. Bladder prolapse can be uncomfortable and uncontrollable, so it's important to diagnose and fix your symptoms as quickly and effectively as possible.
Steps
Part 1 of 4: Recognize the symptoms of bladder prolapse

Feel the presence of a lump in your vagina. In severe cases, you may feel your bladder drop down into your vagina. When you sit down, feel like you are sitting on a ball or an egg; This sensation goes away when getting up or lying down. This is the most recognizable symptom of bladder prolapse, and you should see a specialist or gynecologist as soon as possible.- This sensation is considered a sign of severe bladder prolapse.
Watch for pelvic pain or discomfort. If you experience pain, pressure, or discomfort in your lower abdomen, pelvis, or vagina, see your doctor. Certain medical conditions, including bladder prolapse, may cause any of the above symptoms.- If you have bladder prolapse, you may experience more pain, tightness, or discomfort when you cough, sneeze, exert yourself or put pressure on the pelvic floor. Then you need to describe clearly with your doctor.
- If you have a bladder prolapse, you may feel as if something has come out of your vagina.

Watch for urinary tract symptoms. If you often experience watery urine from coughing, sneezing, laughing, or exerting yourself, you are experiencing "pressure incontinence." Women who have just had a baby are at risk, and the main cause could be bladder prolapse. You need to see a doctor to fix this problem.- Watch for any changes in urination, including difficulty starting to urinate, not passing urine (also called urinary retention), and urination.
- Watch for the frequency of bladder or urinary tract infection (UTI). "regular" is defined if there has been more than one UTI during a six month period. Women with prolapsed bladder also often have bladder infections, so it's important to be careful about how often a UTI occurs.
Watch for painful sex. Pain during sex is called "painful intercourse" and can be caused by a number of physical causes, including prolapse of the bladder. If this happens, you should see your general practitioner or gynecologist as soon as possible.
- If painful sexual intercourse develops, and you have just delivered a baby through the vagina, it may be due to bladder prolapse. In this case, you need to see a doctor as soon as possible.
Watch for back pain. Some women with prolapse of the bladder often experience pain, tightness, or discomfort in the lower back. Back pain is a common symptom of many medical conditions - or nothing serious. However, you still need to see a doctor if other symptoms are present.
Note that some women have no symptoms at all. If the case is mild, you will not experience any of the symptoms listed above. Some bladder cases are discovered during gynecological examination.
- However, if you notice any of the above symptoms, you should see your general practitioner or gynecologist.
- Usually, you don't need treatment if you don't have symptoms,
Part 2 of 4: Find out what causes bladder prolapse
Know that pregnancy and childbirth are the main causes of bladder prolapse. During pregnancy and childbirth, the pelvic muscles and supporting tissues are often stretched. These are groups of muscles that hold the bladder in place, so if they overstretch or weaken, the bladder will sink into the vagina.
- Women who have ever been pregnant, especially women who have had multiple vaginal deliveries, are at a higher risk of developing bladder prolapse. Even women who have a caesarean section can experience this.
Recognize the role of menopause. Women who have gone through menopause are often at risk of bladder prolapse due to lower levels of the female hormone estrogen. Estrogen is responsible for maintaining the strength, firmness and elasticity of the vaginal muscles. Therefore, the drop in estrogen levels with the transition to menopause can make the muscle group thinner and less elastic, causing overall weakness.
- Note that the drop in estrogen persists even if you go into menopause unnaturally, such as a hysterectomy and / or ovarian surgery. These surgeries not only damage the pelvis, but also affect estrogen levels. So, even though you are younger than menopausal women in good health, you still run a risk of bladder prolapse.
Recognize that muscle tension is also a factor in bladder prolapse. Excessive stress or heavy lifting sometimes contributes to bladder prolapse. When you stretch the pelvic floor muscles, you are at risk for bladder prolapse (especially if the vaginal wall muscles are weakened by menopause or childbirth). Here are some muscle-tensioning activities that can cause bladder prolapse:
- Very heavy lifting (including children)
- Chronic and severe cough
- Constipation and straining when using the toilet
Pay attention to your weight. If you are overweight or obese, you are more likely to experience a bladder. Excess weight adds pressure to the pelvic floor muscles.
- You can tell if a person is overweight or obese by the body mass index (BMI), which is a measure of body fat.BMI is calculated by dividing body mass in kg by square of height in m. A BMI of 25-29.9 is considered overweight, and greater than 30 is considered obese.
Part 3 of 4: Diagnosis of bladder prolapse
Seek medical attention. If you think you have a bladder prolapse, see your general practitioner or gynecologist.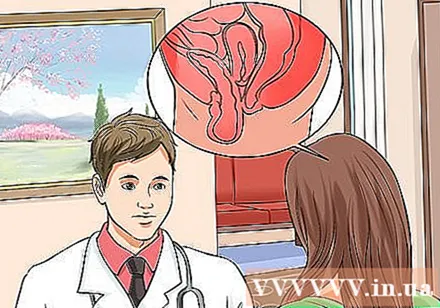
- Provide full information for the doctor, including medical history and detailed description of symptoms of the disease.
Get a gynecological exam. First, the doctor will do a regular gynecological examination. During the exam, your doctor can detect bladder prolapse by pressing the back of your vagina with a speculum (gynecological device) against the back of your vagina while you lie flat, bend your knees, and rest your feet on the pedal. The doctor will ask you to “push” (like when pushing the fetus or waste products out) or cough. If you have a bladder prolapse, your doctor will see or feel a soft bulge in front of the vaginal wall as you stretch.
- Bladder swooping down into the vagina is diagnosed with bladder prolapse.
- In some cases, in addition to the usual gynecological examination, your doctor may have to do further exams while you are standing. This helps the doctor accurately assess the bladder prolapse in each different position.
- If you notice a prolapse of the bladder in the posterior vaginal wall, your doctor will perform a rectal exam. This step helps the doctor determine muscle endurance.
- There is no need to prepare for this test in advance, and it doesn't take long. You will only feel a bit uncomfortable during the gynecological examination, but for many women this is just a routine screening like a smear of the cervix.
Get some other tests if you experience bleeding, incontinence, or impaired sexual function. Your doctor will usually recommend checking bladder pressure or urodynamics.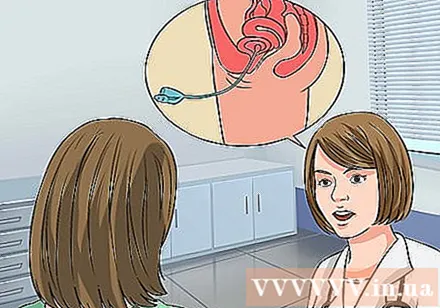
- Bladder pressure measurement measures the amount of urine in your bladder when you start to feel the urge to urinate, when the bladder feels "full," and when the bladder is really full.
- Your doctor will ask you to urinate in a container connected to the computer to take the measurement. Then, you will lie down on the examination table so the doctor will place a thin, flexible urinary catheter into the bladder.
- A urodynamic measurement is a series of different tests that include measuring the flow of urine, the time at which the urination is started, the time it takes to complete the urination, and the amount of urine passed. In addition, the urodynamic measurements also include bladder pressure test as described above, excretion test and flushing phase.
- In most urodynamic tests, your doctor will place a thin, flexible urinary catheter in place while you urinate. Special sensors collect data for the doctor to analyze.
Talk to your doctor about some additional tests. In some cases, your doctor will recommend further testing if bladder prolapse gets worse. Some additional tests include:
- Urine analysis During this test, the urine will be tested for infection (such as a UTI). Your doctor will also check your bladder to see if it is completely empty after urination by inserting a catheter into your urethra to drain urine and measuring the amount of urine remaining after excretion (PVR). If PVR is more than 50-100 ml, it is considered urinary retention, one of the symptoms of bladder prolapse.
- PVR ultrasound The ultrasound test emits sound waves and when it reaches the bladder, it bounces back to the ultrasound machine, creating an image of the bladder. The picture also shows the amount of urine remaining in the bladder after excretion.
- X-ray of the bladder-urethra during urination (VCUG) This is a test that uses X-rays during secretion to look at your bladder and evaluate your condition. The VCUG displays bladder shape and analyzes the urine flow to detect obstruction if present. This test can also be used to diagnose urinary incontinence that is obscured by bladder prolapse. The doctor needs to make these two diagnoses, as the patient also needs surgery for incontinence in addition to treating bladder prolapse (if surgery is needed).
Specific diagnosis. After the doctor concludes that bladder prolapse, you need to ask for more diagnostic information. Bladder prolapse is divided into several levels depending on the severity. Treatment will depend on the type of bladder prolapse, as well as how symptoms appear. Bladder prolapse can fall into one of the following "levels":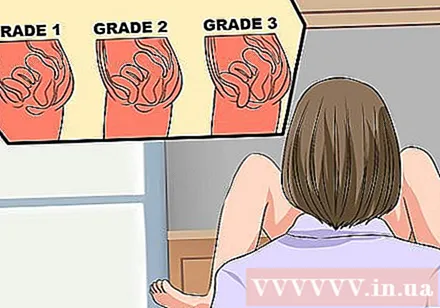
- Mild grade 1 bladder prolapse. If you have grade 1 bladder prolapse, only part of the bladder will enter the vagina. You may experience mild symptoms such as mild discomfort and urination, but some women will have no symptoms. Some remedies include doing Kegel exercises, resting, avoiding heavy lifting and excessive muscle tension. If you are postmenopausal, you may consider estrogen replacement therapy.
- Moderate bladder prolapse. At this point the entire bladder laps into the vagina. They may drop near the vaginal opening. Symptoms such as irritability and urinary incontinence were moderate. Surgical correction of the bladder may be required in this case, but you can still correct the symptoms with a vaginal implant (small plastic or silicone device placed inside the vagina to secure the vaginal wall).
- Severe grade 3 bladder prolapse. During this stage, part of the bladder protrudes out of the vaginal opening. Symptoms of discomfort and urinary incontinence become severe. Treatment includes surgery to correct bladder prolapse and / or using a vaginal lift similar to grade 2 bladder prolapse.
- Grade 4 bladder prolapse is extremely severe. At this point, the entire bladder falls out of the vaginal opening. Then you may have some other more serious problems including prolapse of the uterus and rectum.
Part 4 of 4: Treatment of bladder prolapse
Ask your doctor about treatment. Grade 1 bladder prolapse usually does not require medical treatment, as long as it doesn't cause pain or discomfort in the patient. You need to talk with your doctor about whether you need medical treatment or just follow-up. If your symptoms don't affect much, your doctor will recommend some basic treatments including Kegel exercises and physical therapy.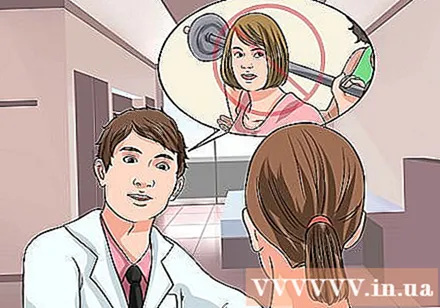
- Note that your doctor may recommend that you stop certain activities like weightlifting or activities that strain the pelvic muscles. However, you can still exercise regularly.
- You should also consider how your symptoms affect your quality of life to make a treatment decision. For example, you may experience severe bladder prolapse but not be affected by accompanying symptoms. In this case, there are some milder treatments you can talk to your doctor about. In other cases, you may experience mild bladder prolapse, but the symptoms are very painful or inconvenient. You can then consult with your doctor about some stronger treatment options.
Practice Kegel. This exercise is done by stretching the pelvic floor muscles (like when urinating), holding for a certain amount of time, and then completely relaxing. You can often work out to strengthen your muscles, as it doesn't require special equipment and can be done anywhere (including waiting in line, sitting at your desk, or taking notes). stretch on the upholstered chair). In mild cases, this exercise can help reduce the bladder sink further. How to practice the Kegel exercises as follows:
- Tense, or contract, the pelvic floor muscles. This is the muscle group used to stop the flow of urine during excretion.
- Tighten your muscles for about five seconds, then relax for about five seconds.
- Gradually increase the time to ten seconds at a time.
- The goal is to do 3 to 4 repetitions each consisting of 10 repetitions
Use a vaginal ring. This small, plastic or silicone ring is inserted inside the vagina to keep the bladder (and other parts of the pelvis) in place. Some are designed for you to insert into your vagina; others need help from a medical professional. Vaginal implants come in many shapes and sizes for the doctor to choose the best ring for the patient.
- The vaginal ring can be uncomfortable, and some women experience a ring that falls out.In addition, they can cause ulcers (if they don't have the right size) and vaginal infections (if not taken apart and cleaned monthly). You need to use estrogen cream to avoid damaging the vaginal wall.
- Despite its limitations, vaginal implants are an effective alternative, especially if you want to delay or not be able to have surgery. Talk to your doctor, and consider the benefits in your case
Try estrogen replacement therapy. Low estrogen levels often cause vaginal muscle weakness, so your doctor may recommend estrogen therapy. Your doctor may prescribe estrogen in the form of pills, a vaginal cream, or a vaginal ring to strengthen the weakened pelvic floor muscles. Creams are not very penetrating, so they only work best in the area of direct contact.
- Estrogen therapy poses a number of risks. Women wearing certain cancers should not take estrogen, and you should discuss the potential risks and benefits of this approach with your doctor. In general, topical estrogen treatments are less risky than oral "systemic" estrogen treatments.
Get surgery. If other treatments don't work, or bladder prolapse becomes particularly severe (grade 3 or 4), your doctor may recommend surgery. This method is more effective in some women. For example, if you are trying to have a baby, you can delay surgery after the baby is born to avoid recurring bladder prolapse after the baby is born. Older women are at high risk during surgery.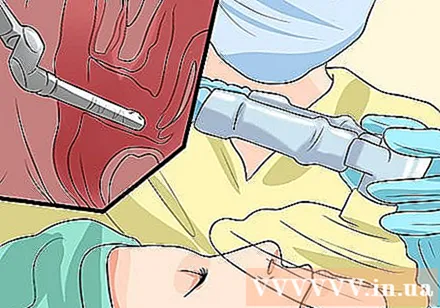
- Vaginal cosmetic surgery is a popular surgical treatment. Your doctor will reposition your bladder, which can then tighten or strengthen the vaginal muscles so that the organs are in place. There are several other types of surgery you can consider, and your doctor will recommend the best surgery for you.
- Your doctor will explain the surgical procedure, the risks and benefits, as well as some of the possible complications prior to surgery. Potential complications include UTI, incontinence, bleeding, inflammation, and in rare cases, urinary tract damage and surgery. In addition, you may feel itchy or painful intercourse after having surgery due to the stitches or scar tissue inside the vagina.
- Depending on the specific situation, you will receive local anesthesia, regional anesthesia, or general anesthesia. Many patients can be discharged from hospital one to three days after surgery and most are able to return to normal activities after about six weeks.
- If you have a prolapse, your doctor may recommend a hysterectomy. If bladder prolapse is associated with pressure incontinence, your doctor may have to perform a parallel urethral suspension procedure.
Advice
- Although it can be painful, uncomfortable, and inconvenient, cystic prolapse can still be cured and is not life-threatening. Don't be alarmed when you think you have a bladder; you just need to see a doctor and talk to your doctor about the right treatment. Then your condition will improve completely.