Author:
Peter Berry
Date Of Creation:
11 February 2021
Update Date:
15 May 2024

Content
Although familiar, do you know when to get the tetanus vaccine? In the US, as in other developed countries, tetanus is very rare due to its high vaccination rate. Vaccination is of utmost importance because tetanus does not yet have a cure and it stems from bacterial toxins found in soil, dirt and animal waste. This toxic bacteria in the form of spores is difficult to destroy because they are heat resistant and resistant to many drugs and chemicals. Tetanus bacteria attack the nervous system and cause pain with muscle contractions, especially in the jaw and neck.It can also cause choking and lead to death. For the reasons above, it's very important to know when to get the tetanus vaccine.
Steps
Part 1 of 3: Know When to Get a Tetanus Vaccination

Booster shots when suffering certain injuries. Normally, bacterial toxins enter the body through a tear created by the tetanus bacteria carrier. If you have one or more injuries or injuries that easily lead to tetanus, you should get a booster shot. These include:- Any wound contaminated by dirt, dust or horse droppings.
- The stab wound. Objects that cause this type of injury include wood chips, nails, needles, glasses, and bites from humans or animals.
- Skin burns. Second degree (topical) and third degree (full thickness burns) burns have a higher risk of infection than first degree (superficial) burns.
- Collision injury results in tissue damage caused by compression between two heavy objects. They can also happen when a body part has been hit by a heavy object.
- The wound involves tissue necrosis or death. The absence of nourished blood increases the risk of infection (along with severe damage) of these tissues. For example, the ultraviolet (dead tissue) is at a higher risk of infection.
- The wound contains foreign material. Wounds that contain foreign objects such as debris, glass chips, stones, or other objects are at greater risk of infection.
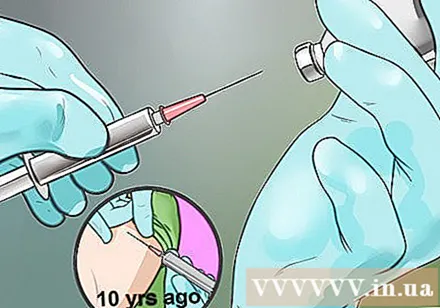
Know if it's time to get a tetanus shot. In the event that you have never had a tetanus series (the first series of shots) or when your last shot is uncertain, you should get a tetanus shot. If you are injured, you may wonder if a booster tetanus shot is needed. You will need it if:- The wound was caused by the "clean" object, but your last tetanus nose was more than 10 years ago.
- The wound was caused by the "dirty" object and the last tetanus nose more than 5 years ago.
- You're not sure if the injured object is "clean" or "dirty" and the last tetanus nose was more than five years ago.

Injections during pregnancy. To pass tetanus antibodies to the atrium, you should get the vaccine during a 27-36 week pregnancy.- Your doctor will likely recommend a Tdap (tetanus, diphtheria and pertussis) vaccine in the third trimester of your pregnancy.
- If you have not had the Tdap vaccine before and did not get it during pregnancy, you should do it right after delivery.
- If there was a cut or wound dirty during pregnancy, you should get a booster shot of tetanus.
Become immune. The best way to "cure" tetanus is to prevent it in the first place. Although moderate reactions are fairly common after injection, serious cases are rare. Moderate reactions include swelling, pain, and redness at the injection site. However, they usually disappear within 1-2 days. Don't worry about getting a booster shot. Usually it doesn't matter if you don't wait 10 years for the next shot. Some of the vaccines against tetanus include:
- DTaP. The vaccines against diphtheria, tetanus, and pertussis (long-term cough) are usually given at 2, 4, 6 months of age and as a booster at 15 to 18 months of age. DTap is especially effective for young children. Children usually need a booster nose between 4 and 6 years old.
- Tdap. Over time, tetanus immunity declines. Therefore, older children need booster shots. The booster nose contains a sufficient dose of tetanus vaccine and reduces the dose of diphtheria and pertussis. Anyone between 11 and 18 years old is advised to get a booster shot, with the best age being 11 or 12 years old.
- Td. If you are an adult, get a booster shot of Td (tetanus and diphtheria) every ten years to maintain immunity. Since antibody levels decline after 5 years, booster shots are recommended if you have deep, septic wounds and have not been vaccinated for more than 5 years.
Part 2 of 3: Knowing and Identifying Tetanus
Find out who is prone to tetanus and how it spreads. Nearly every case of tetanus occurs only in people who have never had a tetanus shot or in adults who don't follow their 10-year booster schedule. However, unlike other vaccinated diseases, tetanus is not passed from person to person. Instead, it is spread by bacterial spores - often entering the body through an open wound. They produce a powerful neurotoxin that causes muscle spasms and stiffness.
- Complications from tetanus are highest in unvaccinated people or in adults who are not sufficiently immunized in industrialized countries.
- You can also be at risk of tetanus following a disaster, especially when living in a developing country.
Reduce the risk of tetanus. As soon as you get injured or injured, wash and disinfect it. Delaying disinfection of the wound for more than 4 hours increases the risk of tetanus. This is even more important in cases where the wound is caused by an object puncturing the skin, allowing bacteria and debris to penetrate deeply into the wound, making it ideal for tetanus bacteria growth. .
- Note the cleanliness of the injector to determine the need for a booster nose. Dirty or contaminated objects will be covered with dirt / soil, saliva or feces / waste and clean objects will not. Remember, you don't have to know exactly whether the material contains bacteria or not.
Pay attention to the symptoms. The incubation period of tetanus is heterogeneous, ranges from 3 to 21 days and the average incubation period is 8 days. The severity of tetanus is determined on a scale from I to IV. The longer the incubation period, the milder the illness is usually. Common tetanus symptoms (in the order of appearance) include:
- Jaw muscle contraction (commonly known as "lockjaw")
- Neck stiffness
- Difficulty swallowing (dysphagia)
- Abdominal muscles tighten like boards
Be aware of other tetanus symptoms. Symptoms are the sole basis for a diagnosis of tetanus. No blood test can diagnose tetanus, so it's important to recognize all the symptoms. You may also have signs of fever, sweating, increased blood pressure, or a fast heartbeat (tachycardia). Possible complications include:
- Laryngeal spasm or spasm of the vocal cords leading to difficulty breathing
- Fracture
- Seizures / convulsions
- Abnormal heart rhythm
- Secondary infections such as pneumonia due to prolonged illness
- Pulmonary embolism or blood clot in the lung
- Mortality (10% of all reported cases)
Part 3 of 3: Treatment of Tetanus
Healthcare. If you think or even suspect you have tetanus, seek medical attention immediately. It is a medical emergency and you need to be hospitalized because it is a disease with a high mortality or mortality rate (10%). In the hospital, you will be given an anti-tetanus serum such as tetanus immune globulin. It helps neutralize any toxins that have yet to attack your nerve cells. The wound is completely cleaned and you will be given a tetanus vaccine to prevent future infection.
- Tetanus infection does not mean that you will be immune in the future. In fact, in order not to re-infection, you need the tetanus vaccine.
Let your doctor decide what treatment is for you. There is no blood test that can diagnose tetanus. Therefore, laboratory testing is useless in evaluating this disease. Therefore, most doctors cannot wait and follow but choose active treatment when they suspect an infection.
- Doctors diagnose mainly based on symptoms and current clinical signs. The more severe the symptoms, the more urgent the treatment will be.
Treatment of tetanus symptoms. As there is no cure for tetanus, the symptoms and associated complications are the subject of the treatment. You will be given oral, injectable or intravenous antibiotics and drugs to control muscle spasms.
- Some medications that control muscle spasms include benzodiazepines (such as diazepam (Valium), lorazepam (Ativan), alprazolam (Xanax), and midazolam (Versed) pain relievers.
- Antibiotics are usually ineffective with tetanus, but they can be prescribed to inhibit the spontaneous reproduction of the Clostridium tetani bacteria. This can slow the production of toxins.
Advice
- There are vaccines that also protect against diphtheria and pertussis (Tdap) and diphtheria only (Td). Both types are effective for 10 years.
- The last booster date is on the immunization record at your doctor's office. Personal card showing date of injection can be obtained from your doctor.
- If there is a risk of infection, make sure you understand the signs and complications of tetanus. Spasms can become so severe that they interfere with normal breathing. Seizures can be so severe that it can lead to a fracture of the spine or long bones.
- If you are particularly concerned about tetanus infection, get vaccinated.
- A few rare diseases can have symptoms similar to tetanus. Malignant hyperthermia is an inherited disease that causes rapid fever and severe muscle spasm under anesthesia. Nervousness syndrome is an extremely rare disease involving the nervous system, causing cyclical muscle contractions. Symptoms usually begin around 45 years old.
Warning
- Seek emergency medical attention for any serious injury or injury. If you suspect a tetanus infection, don't wait for symptoms to appear for appropriate treatment. Tetanus is incurable, we can only deal with symptoms until the disease is over.



